Subacute Granulomatous Thyroiditis (de Quervain)
Lester D. R. Thompson, MD
Key Facts
Terminology
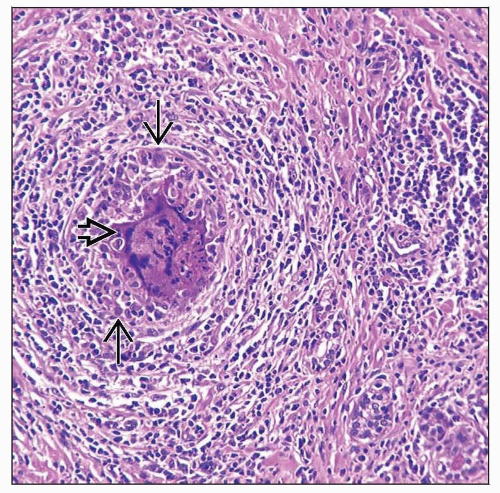
Self-limited inflammatory condition characterized by epithelioid histiocytes, multinucleated giant cells, and acute inflammatory cells
Clinical Issues
Female > > Male (3.5:1)
Entire gland usually involved
Painful thyroid gland is most common symptom
Frequently presents with hyperthyroidism
Spontaneous return to normal function in most patients within 12 months
Thyroid function varies during disease arc
Supportive therapy is treatment of choice
Microscopic Pathology
Asymmetric enlargement with tan to yellow-white ill-defined nodules
Inflammatory process unevenly affects entire gland
Topographic and temporal variation of histology depending on stage
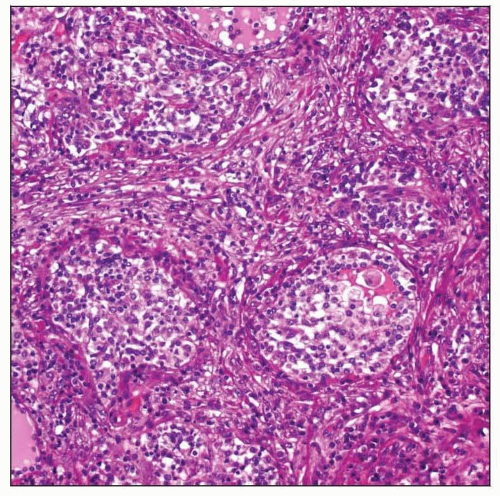
Acute stage: Folliculocentric, follicular damage, loss of epithelium and colloid, replaced by neutrophils
Mid stage: Chronic inflammation, epithelioid histiocytes, multinucleated giant cells, fibrosis
Resolution stage: Follicular tissue is regenerated, restoring normal structure
Top Differential Diagnoses
Subacute lymphocytic thyroiditis, granulomatous thyroiditis, sarcoidosis, palpation thyroiditis
TERMINOLOGY
Abbreviations
Subacute granulomatous thyroiditis (SGT)
Synonyms
Subacute thyroiditis
Granulomatous thyroiditis
de Quervain thyroiditis
Painful subacute thyroiditis
Postviral thyroiditis
Giant cell thyroiditis
Subacute nonsuppurative thyroiditis
Pseudotuberculous thyroiditis
Struma granulomatosa
Definitions
Self-limited inflammatory condition characterized by epithelioid histiocytes, multinucleated giant cells, and acute inflammatory cells (at certain times in disease development)
Requires clinicopathologic correlation with known systemic disease
Granulomatous inflammation can be seen in patients with tuberculosis, fungal infections, sarcoidosis
ETIOLOGY/PATHOGENESIS
Infectious
Systemic viral infection most common
Common prodromal signs and symptoms
Intrathyroidal activated T-cytotoxic cells with interferon γ positive lymphocytes
Incidence highest in summer months, coincident with enteroviral infections
Associated with mumps, influenza, Coxsackie adenovirus, and measles epidemics
However, a significant number of patients do not have viral infection
Develops after antiviral therapy, specifically interferon
Inherited
Genetic predisposition suggested
Increased frequency in patients with HLA-B35 haplotype
Autoimmune
Possible autoimmune component, as there are thyroid autoantibodies in a few patients
CLINICAL ISSUES
Epidemiology
Incidence
Incidence approximately 5 per 100,000 population per year
Suggested seasonal increase in spring and summer
Age
Wide range
Peak: 5th decade
Rare in children
Gender
Female > > Male (3.5:1 )
Site
Entire gland usually involved
May be localized to 1 lobe or a distinct nodule
Presentation
Prodrome heralds disease
Low-grade fever, myalgias, fatigue, sore throat
Painful thyroid gland is most common symptom
SGT is most common cause of painful thyroid
May radiate to jaw
Tender to palpation
Some patients may not have pain or tenderness
Frequently presents with hyperthyroidism
Rarely, may present with thyroid storm
Become hypothyroid in ensuing weeks to months
Spontaneous return to normal function in most patients within 12 months
˜ 7% have persistent hypothyroidism
May have other symptoms, including
Dysphagia, arthralgia, tremor, excessive sweating, weight loss
Laboratory Tests
Thyroid function varies during disease arc
Early phase: May be hyperthyroid due to follicle destruction and release of hormone
TSH is suppressed; T4 and T3 are elevated
Mid phase: Become hypothyroid after follicles are destroyed
Late phase: Regain euthyroid after disease resolution
Few patients may have transient elevation of antibodies to thyroglobulin or thyroperoxidase
C-reactive protein and erythrocyte sedimentation rate are usually elevated