Squamous Cell Carcinoma
Lester D. R. Thompson, MD
Key Facts
Terminology
Thyroid primary squamous cell carcinoma is composed entirely of squamous cells without mucocytes and without direct invasion from adjacent organs (larynx, esophagus)
Clinical Issues
Mean: 6th and 7th decades
Female > Male (3:1)
Patients present with rapidly enlarging neck mass
Early radical resection yields best prognosis
Radical-dose radiotherapy is part of initial treatment
Prognosis is poor; mean survival: < 1 year; 5-year survival: < 10%
Microscopic Pathology
Must 1st exclude direct extension: Larynx, esophagus
Widely invasive tumor, destroying thyroid parenchyma
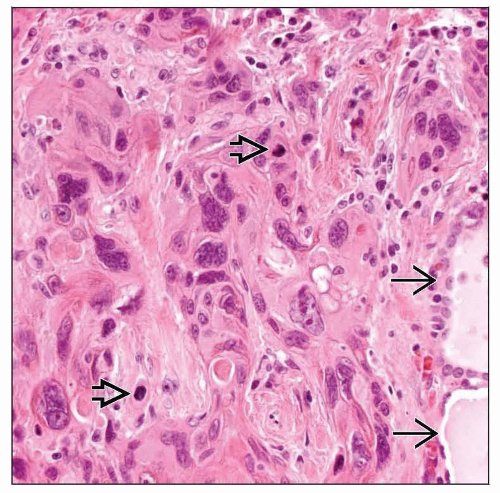
Cohesive cells arranged in sheets, ribbons, nests
Polygonal, polyhedral, and spindle tumor cells
Keratinization and keratin pearl formation
High mitotic index, including atypical forms
Classified as keratinizing or nonkeratinizing
Ancillary Tests
Positive: Keratin, CK5/6, CK19, p63
Negative: Thyroglobulin, CEA, calcitonin, CD5
Top Differential Diagnoses
Direct extension from adjacent organs
Metastatic squamous cell carcinoma
Extensive squamous metaplasia
CASTLE
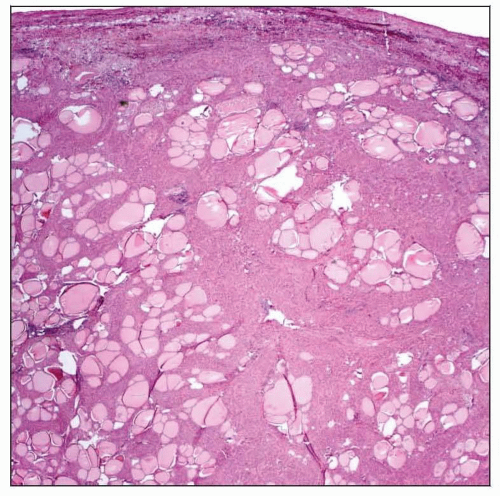 The thyroid gland is nearly completely replaced by a widely infiltrating tumor. The tumor type is not identifiable at this magnification, but effacement of the thyroid gland is obvious. |
TERMINOLOGY
Abbreviations
Squamous cell carcinoma (SCC)
Definitions
Thyroid primary squamous cell carcinoma is composed entirely of squamous cells without mucocytes and without direct invasion from adjacent organs (larynx, esophagus)
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Radiation history is occasionally present
Pathogenesis
Derived from thyroid follicular epithelium
Directly or via squamous metaplasia, then additional alterations to reach malignant tumor
Persistence of thyroglossal duct or branchial pouch embryonic remnants
CLINICAL ISSUES
Epidemiology
Incidence
Rare: < 1% of malignant thyroid tumors
Age
Mean: 6th and 7th decades
Gender
Female > Male (3:1)
Site
Affects one or both lobes of thyroid gland
Presentation
Patients present with rapidly enlarging neck mass
Many have preexisting thyroid disease
Frequent recurrent laryngeal nerve compression and pressure symptoms
Airway obstruction, dyspnea, dysphagia
Direct involvement of nerves, vessels, and soft tissues
Cervical lymph node enlargement is common
Hashimoto thyroiditis is concurrently identified in a few patients
Paraneoplastic syndrome is rare
Hypercalcemia, fever, and leukocytosis
Probably develops as result of tumor-derived humoral mediators
Endoscopic Findings
Endoscopic evaluation (laryngoscopy, esophagoscopy, bronchoscopy) to exclude direct extension
Treatment
Options, risks, complications
Airway collapse and esophagotracheal fistula may complicate course
Surgical approaches
Early radical resection yields best prognosis
Debulking if clear margins cannot be achieved
Drugs
Thyroid hormone suppression may help
Thyroid-stimulating hormone may be a growth factor
Chemotherapy does not alter disease course
Radiation
Radical-dose radiotherapy is part of initial treatment
Radiation alone for unresectable tumors &/or poor surgical candidates
Radioiodine therapy does not work
Prognosis
Nearly all patients present with advanced disease
Tumors follow rapidly fulminant course
Prognosis is poor; mean survival: < 1 year; 5-year survival: < 10%
Localized disease only; managed aggressively, patients may survive longer
Airway compromise results in death
Local invasion and lymph node metastases is common
Distant metastasis (lung) is less common (˜ 30%)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree