INTRODUCTION
The spirochetes are a large, heterogeneous group of spiral, motile bacteria. One family (Spirochaetaceae) of the order Spirochaetales consists of two genera whose members are human pathogens, Borrelia and Treponema. The other family (Leptospiraceae) includes one genus of medical importance: Leptospira.
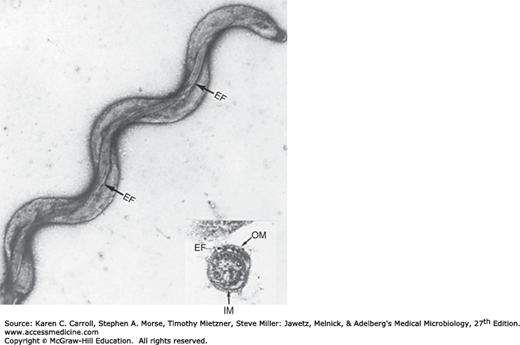
The spirochetes have many structural characteristics in common, as typified by Treponema pallidum (Figure 24-1). They are long, slender, helically coiled, spiral, or corkscrew-shaped bacilli. T pallidum has an outer sheath or glycosaminoglycan coating. Inside the sheath is the outer membrane, which contains peptidoglycan and maintains the structural integrity of the organisms. Endoflagella (axial filaments) are the flagella-like organelles in the periplasmic space encased by the outer membrane. The endoflagella begin at each end of the organism and wind around it, extending to and overlapping at the midpoint. Inside the endoflagella is the inner membrane (cytoplasmic membrane) that provides osmotic stability and covers the protoplasmic cylinder. A series of cytoplasmic tubules (body fibrils) are inside the cell near the inner membrane. Treponemes reproduce by transverse fission.
FIGURE 24-1
Electron micrograph of whole-mounted Treponema pallidum subspecies pallidum. The endoflagella are clearly visible. Inset: Electron micrograph of thin-sectioned Treponema pallidum. Note the position of the endoflagella (EF) in the periplasmic space between the inner membrane (IM) and the outer membrane (OM). (Courtesy of EM Walker.)
TREPONEMA PALLIDUM AND SYPHILIS
T pallidum are slender spirals measuring about 0.2 μm in width and 5–15 μm in length. The spiral coils are regularly spaced at a distance of 1 μm from one another. The organisms are actively motile, rotating steadily around their endoflagella even after attaching to cells by their tapered ends. The long axis of the spiral is ordinarily straight but may sometimes bend so that the organism forms a complete circle for moments at a time, returning then to its normal straight position.
The spirals are so thin that they are not readily seen unless immunofluorescent stain or dark-field illumination is used. They do not stain well with aniline dyes, but they can be seen in tissues when stained by a silver impregnation method.
Pathogenic T pallidum has never been cultured continuously on artificial media, in fertile eggs, or in tissue culture.
In proper suspending fluids and in the presence of reducing substances, T pallidum may remain motile for 3–6 days at 25°C. In whole blood or plasma stored at 4°C, organisms remain viable for at least 24 hours, which is of potential importance in blood transfusions.
Drying kills the spirochete rapidly, as does elevation of the temperature to 42°C. Treponemes are rapidly immobilized and killed by trivalent arsenical, mercury, and bismuth (contained in drugs of historical interest in the treatment of syphilis). Penicillin is treponemicidal in minute concentrations, but the rate of killing is slow, presumably because of the metabolic inactivity and slow multiplication rate of T pallidum (estimated division time is 30 hours). Resistance to penicillin has not been demonstrated in syphilis.
The T pallidum genome is a circular chromosome of approximately 1,138,000 base pairs, which is small for bacteria. Most pathogenic bacteria have transposable elements, but T pallidum does not, which suggests that the genome is highly conserved and may explain its continued susceptibility to penicillin. There are few genes involved in energy production and synthesis of nutrients, indicating that T pallidum obtains these from the host.
The fact that T pallidum cannot be cultured in vitro has markedly limited the characterization of its antigens. The outer membrane surrounds the periplasmic space and the peptidoglycan–cytoplasmic membrane complex. Membrane proteins are present that contain covalently bound lipids at their amino terminals. The lipids appear to anchor the proteins to the cytoplasmic or outer membranes and keep the proteins inaccessible to antibodies. The endoflagella are in the periplasmic space. T pallidum has hyaluronidase that breaks down the hyaluronic acid in the ground substance of tissue and presumably enhances the invasiveness of the organism. The endoflagella are composed of three core proteins that are homologous to other bacterial flagellin proteins plus an unrelated sheath protein. Cardiolipin is an important component of the treponemal antigens.
Humans with syphilis develop antibodies capable of staining T pallidum by indirect immunofluorescence, immobilizing and killing live motile T pallidum and fixing complement in the presence of a suspension of T pallidum or related spirochetes. The spirochetes also cause the development of a distinct antibody-like substance, reagin, which gives positive complement fixation (CF) and flocculation test results with aqueous suspensions of cardiolipin extracted from normal mammalian tissues. Both reagin and antitreponemal antibody can be used for the serologic diagnosis of syphilis.
Natural infection with T pallidum is limited to the human host. Human infection is usually transmitted by sexual contact, and the infectious lesion is on the skin or mucous membranes of genitalia. In 10–20% of cases, however, the primary lesion is intrarectal, perianal, or oral. It may be anywhere on the body. T pallidum can probably penetrate intact mucous membranes, or the organisms may enter through a break in the epidermis. Based on experiments in rabbits, as few as four to eight spirochetes may cause infection.
Spirochetes multiply locally at the site of entry, and some spread to nearby lymph nodes and then reach the bloodstream. Within 2–10 weeks after infection, a papule develops at the site of infection and breaks down to form an ulcer with a clean, hard base (“hard chancre”). The inflammation is characterized by a predominance of lymphocytes and plasma cells. This “primary lesion” always heals spontaneously, but 2–10 weeks later, the “secondary” lesions appear. These consist of a red maculopapular rash anywhere on the body, including the hands and feet, and moist, pale papules (condylomas) in the anogenital region, axillae, and mouth. The patient may also have syphilitic meningitis, chorioretinitis, hepatitis, nephritis (immune complex type), or periostitis. The secondary lesions also subside spontaneously. Both primary and secondary lesions are rich in spirochetes and are highly infectious. Contagious lesions may recur within 3–5 years after infection, but thereafter the individual is not infectious. Syphilitic infection may remain subclinical, and the patient may pass through the primary or secondary stage (or both) without symptoms or signs yet develop tertiary lesions.
In about 30% of cases, early syphilitic infection progresses spontaneously to complete cure without treatment. In another 30%, the untreated infection remains latent (principally evident by positive serologic test results). In the remainder, the disease progresses to the “tertiary stage” characterized by the development of granulomatous lesions (gummas) in the skin, bones, and liver; degenerative changes in the central nervous system (meningovascular syphilis, paresis, tabes); or cardiovascular lesions (aortitis, aortic aneurysm, aortic valve insufficiency). In all tertiary lesions, treponemes are very rare, and the exaggerated tissue response must be attributed to hypersensitivity to the organisms. However, treponemes can occasionally be found in the eye or central nervous system in late syphilis.
A pregnant woman with syphilis can transmit T pallidum to the fetus through the placenta beginning in the 10th–15th weeks of gestation. Some of the infected fetuses die, and miscarriages result; others are stillborn at term. Others are born live but develop the signs of congenital syphilis in childhood, including interstitial keratitis, Hutchinson’s teeth, saddlenose, periostitis, and a variety of central nervous system anomalies. Adequate treatment of the mother during pregnancy prevents congenital syphilis. The reagin titer in the blood of the child rises with active infection but falls with time if antibody was passively transmitted from the mother. In congenital infection, the child makes IgM antitreponemal antibody.
Specimens include tissue fluid expressed from early surface lesions for demonstration of spirochetes by either dark-field microscopy or immunofluorescence; such specimens can also be tested by nucleic acid amplification. Blood can be obtained for serologic tests; cerebrospinal fluid (CSF) is useful for Venereal Disease Research Laboratory (VDRL) testing (see later discussion).
A drop of tissue fluid or exudate is placed on a slide, and a coverslip is pressed over it to make a thin layer. The preparation is then examined under oil immersion within 20 minutes of collection with dark-field illumination for typical motile spirochetes. Dark-field microscopy should not be performed on lesions within the oral cavity because it is not possible to differentiate pathogenic from commensal spirochetes.
Treponemes disappear from lesions within a few hours after the beginning of antibiotic treatment.
Tissue fluid or exudate is spread on a glass slide, air dried, and sent to the laboratory. It is fixed, stained with a fluorescein-labeled antitreponeme antibody, and examined by means of immunofluorescence microscopy for typical fluorescent spirochetes.
These tests use either nontreponemal or treponemal antigens.
1. Nontreponemal tests—The nontreponemal tests are universally used as screening tests for syphilis. The tests are widely available, lend themselves to automation with ease of performance in large numbers, and have a low cost. In addition to their function as screening tests, they can be used to follow the efficacy of therapy. The drawbacks to the nontreponemal tests are that they are not very sensitive in early syphilis, and the results may not turn positive until a few weeks after initial infection; false-positive results can occur with many other diseases; and there may be a prozone phenomenon, particularly in secondary syphilis (antibody excess produces a negative result at low serum dilutions but positive results at higher dilutions). The antigens in these tests contain measured amounts of cardiolipin, cholesterol, and purified lecithin in quantities sufficient to yield a standardized amount of reactivity. Historically, the cardiolipin was extracted from beef heart or liver with added lecithin and cholesterol to enhance reaction with syphilitic “reagin” antibodies. Reagin is a mixture of IgM and IgG antibodies reactive with the cardiolipin–cholesterol–lecithin complex. All of the tests are based on the fact that the particles of the lipid antigen remain dispersed in normal serum but flocculate when combining with reagin. The VDRL and unheated serum reagin (USR) tests require microscopic examination to detect flocculation. The rapid plasma reagin (RPR) test and toluidine red unheated serum test (TRUST) have colored particles that become caught in the mesh of the antigen–antibody complex, allowing the tests to be read without microscopic magnification. Results develop within a few minutes, particularly if the suspension is agitated.
The nontreponemal tests can give quantitative results using serial twofold dilutions. An estimate of the amount of reagin present in serum can be expressed as the titer or as the highest dilution giving a positive result. Quantitative results are valuable in establishing a diagnosis and in evaluating the effect of treatment. Positive nontreponemal test results develop after 2–3 weeks of untreated syphilis and are positive in high titer in secondary syphilis. Positive nontreponemal test results typically revert to negative, often in 6–18 months and generally by 3 years after effective treatment of syphilis. A positive nontreponemal test result late after treatment for syphilis suggests ineffective treatment or reinfection.
The VDRL test is standardized for use on CSF, and the result becomes positive in patients with neurosyphilis. Reagin antibodies generally do not reach the CSF from the bloodstream but are probably formed in the central nervous system in response to syphilitic infection. The serologic diagnosis of neurosyphilis is complex.
2. Treponemal antibody tests—The treponemal tests measure antibodies against T pallidum antigens. The tests are used to determine if a positive result from a nontreponemal test is truly positive or falsely positive. A positive result of a treponemal test on a serum specimen that is also positive on a nontreponemal test is a strong indication of T pallidum infection. The traditional treponemal tests are less useful as screening tests because once positive after initial syphilitic infection the tests remain positive for life independent of therapy for syphilis. Serial dilutions of serum are not done in the treponemal tests, and results are reported as reactive or nonreactive (or occasionally inconclusive). The treponemal antibody tests tend to be more costly than the nontreponemal test, which is important when large groups of people (eg, blood donors) are being screened.
The T pallidum–particle agglutination (TP-PA) test is perhaps the most widely used treponemal test in the United States. Gelatin particles sensitized with T pallidum subspecies pallidum antigens are added to a standard dilution of serum. When anti-T pallidum antibodies (IgG, IgM, or both) react with the sensitized particles, a mat of agglutinated particles forms in the well of the microdilution tray. Gelatin particles that are not sensitized are tested with diluted serum to exclude nonspecific agglutination.
The T pallidum hemagglutination (TPHA) and the microhemagglutination T pallidum (MHA-TP) are based on the same principles as the TP-PA but use sheep erythrocytes rather than gelatin particles and may be more prone to nonspecific agglutination.
The fluorescent treponemal antibody absorbed (FTA-ABS) test is the treponemal antibody test used for many years. Because it is difficult to perform, the test is used only in selected circumstances. The test uses indirect immunofluorescence to detect reactive antibodies, including killed T pallidum and the patient’s serum absorbed with sonicated saprophytic Reiter spirochetes plus antihuman γ-globulin labeled with a fluorescent compound. The presence of IgM FTA in the blood of newborns is a good evidence of in utero infection (ie, congenital syphilis). A negative FTA-ABS result on CSF tends to exclude neurosyphilis, but a positive FTA-ABS result on CSF can occur by transfer of antibodies from serum and is not helpful in the diagnosis of neurosyphilis.
Multiple relatively similar treponemal antibody tests using enzyme immunoassay (EIA) or chemiluminescence (CIA) formats for T pallidum are available. These tests use antigens obtained by sonication of T pallidum or recombinant antigens. An aliquot of serum at a standard dilution is added to a sensitized well of a microdilution plate. After washing, addition of an enzyme-labeled conjugate, and further washing, a precursor substrate is added. A color change or CIA indicates a reactive serum. Because some of these assays are available as high-throughput automated tests, many laboratories have now reversed the traditional algorithm for screening. Instead of screening with the nontreponemal test and verifying with a treponemal assay, the high throughput allows screening with a more sensitive treponemal test. The advantage to this approach is that patients with early disease or untreated latent disease are more likely to be detected (see earlier discussion).
There are some concerns about variability in assay performance among these tests that result in more false positives when testing low-prevalence populations. Because of this, the Centers for Disease Control and Prevention (CDC) has recommended an algorithm for confirming a positive EIA or CIA test result with a quantitative RPR or other nontreponemal test. If the RPR result is positive, a current or past infection with syphilis is likely. If the RPR result is negative, then additional testing with a traditional treponemal test such as the TP-PA is recommended. If the TP-PA result is positive, syphilis is likely; if it is negative, syphilis is unlikely.
A person with active or latent syphilis appears to be resistant to superinfection with T pallidum. However, if early syphilis is treated adequately and the infection is eradicated, the individual again becomes fully susceptible. The various immune responses usually fail to eradicate the infection or arrest its progression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree