Solid-Pseudopapillary Tumors
Grace E. Kim, MD
Key Facts
Terminology
Solid-pseudopapillary tumor (SPT)
Low-grade malignant neoplasm of uncertain cellular differentiation
Etiology/Pathogenesis
90-100% harbor mutations in β-catenin gene
Clinical Issues
Occurs predominately in young females
Presents with nonspecific symptoms related to intraabdominal mass
Can be located in head, body, or tail of pancreas
Indolent and nonaggressive behavior
Metastasis in 10-15% of cases to liver, peritoneum, and lymph node
> 80% are cured with surgical resection
Microscopic Pathology
Well-demarcated large mass
Solid monomorphic sheets of polygonal cells
Delicate vessels surrounded by hyalinized or myxoid stroma
Characteristic degenerative change
Pseudopapillae formation
Intracytoplasmic eosinophilic hyaline globules (PASD positive)
Uniform round to oval nuclei with finely dispersed chromatin
Neoplastic cells often have nuclear grooves
Immunoreactivity for β-catenin (nuclear staining)
Top Differential Diagnoses
Pancreatic endocrine tumor
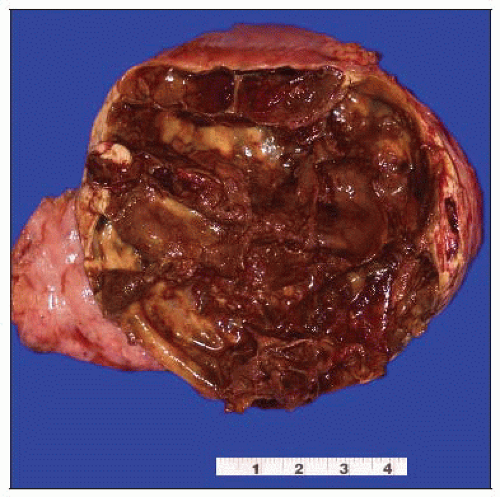
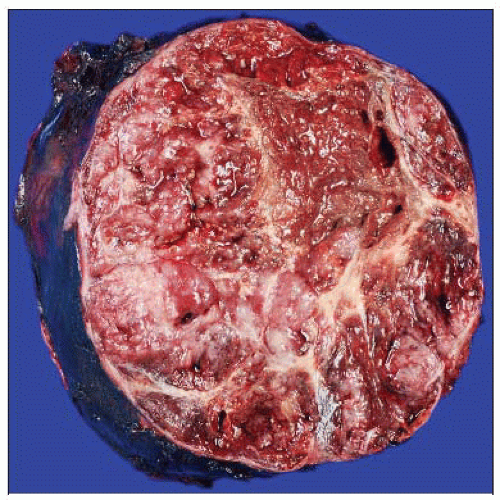 This well-demarcated tumor has a soft and friable solid surface with hemorrhagic areas. Grossly, this could mimic a pancreatic endocrine tumor. |
TERMINOLOGY
Abbreviations
Solid-pseudopapillary tumor (SPT)
Solid-pseudopapillary neoplasm (SPN)
Synonyms
Plethora of descriptive names
Solid and papillary epithelial neoplasm
Solid cystic tumor
Papillary and cystic neoplasm
Frantz tumor
Definitions
Low-grade malignant neoplasm of uncertain cellular differentiation
Originally described in 1959
ETIOLOGY/PATHOGENESIS
Cellular Lineage
Uncertain
Electron microscopy shows evidence of epithelial differentiation
Molecular
90-100% harbor mutations in β-catenin gene
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon
1-2% of all exocrine pancreatic tumors
Age
Most patients in 20s and 30s
Mean: 25-35 years
Overall age range: 7-79 years
Gender
Female predominance
Male to female ratio 1:9-20
Site
Evenly distributed throughout pancreas
Presentation
Nonspecific symptoms related to intraabdominal mass
Vague abdominal pain
Weight loss
Anorexia
May have palpable abdominal mass
Up to 1/3 of cases discovered incidentally
Complications
Rupture
Hemoperitoneum
Laboratory Tests
Serum oncomarkers, laboratory tests usually normal
Natural History
Most are indolent, slow-growing, and nonaggressive
May directly invade stomach, duodenum, spleen
Metastasis
10-15% of cases
Liver, peritoneum, lymph nodes
Peritoneal metastases more common in patients with trauma, rupture, or drainage of neoplasm
Rare, clinically aggressive variant
Treatment
Surgical resection is treatment of choice
Can recur if incompletely resected
Prognosis
Excellent
> 80% cured with surgical resection
10-15% of cases have metastases or recurrence
Even patients with metastases have favorable longterm survival
No proven morphologic predictors of outcome
IMAGE FINDINGS
General Features
Radiographic features reflect variable gross findings
Well-circumscribed neoplasm with solid and cystic components
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree