Modified from Fiore MC, Jaen CR, Baker TB, et al. Clinical Practice Guideline. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians/update/index.html. Last accessed 1/14/15.
MEDICATIONS
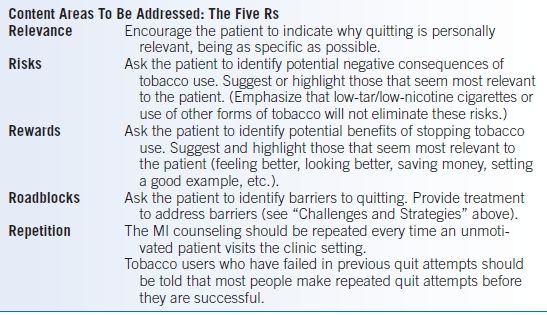
Recommendations
- Pharmacologic therapy can approximately double the quit rate as compared to placebo and should be offered to all patients except in the presence of limited special circumstances (see below).
- First-line treatments include nicotine replacement therapy (NRT), sustained-release bupropion (bupropion SR), and varenicline (see Table 45-2).
TABLE 45-2 Medications to Aid Smoking Cessation
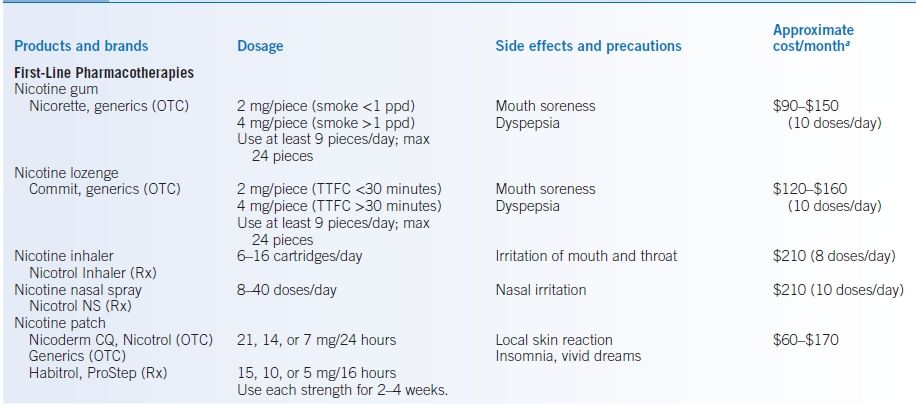
aInformal survey of prices in several pharmacies in the St. Louis, MO area, January, 2013.
bNot FDA approved for smoking cessation.
OTC, over the counter; ppd, pack per day; Rx, by prescription only; TTFC, time to first cigarette after waking.
Nicotine Replacement Therapy
- NRT provides an alternative source of nicotine to ease withdrawal symptoms while the patient learns new nonsmoking behaviors. Many studies have documented that the use of NRT can increase long-term success rates 1.5-fold (nicotine replacement gum) to 2-fold (other NRT) compared to placebo.4
- NRT is most effective when combined with counseling. The effectiveness of counseling increases with the intensity of treatment, but even brief interventions are of benefit.
- Some experts advocate so-called harm reduction—the use of NRT for as long as it takes to keep patients from smoking.12
Safety of Nicotine Replacement Therapy
- Smokers smoke in order to get nicotine, but essentially all of the adverse health effects of smoking stem from other constituents in tobacco and its smoke. Thus, a cigarette is a contaminated drug delivery device. Cigarette smoke contains over 4,000 chemical compounds (the tar), ranging from carbon monoxide to hydrogen cyanide, and 69 of which are known carcinogens, including arsenic, benzene, and polonium 210.13
- The dose-response relation for nicotine is flat making the effects of smoking plus NRT similar to smoking alone.
- NRT is a safe alternative to cigarettes and does not cause heart attacks, lung cancer, or asthma, as some have claimed.14
- The most common side effect of nicotine is local irritation, such as a rash under a nicotine patch or throat irritation from inhaled nicotine.
- Overuse of nicotine, whether from smoking or from NRT, can cause symptoms of nausea, vomiting, dizziness, sweating, palpitations, or anxiety.
- Massive overdose can cause seizures and cardiovascular collapse. All nicotine-containing products should be disposed of out of reach of small children and pets to avoid accidental poisoning. NRT is unlikely to cause addiction due to the low level of nicotine (<half that of smoking) and the slow delivery to the brain.
Safety of NRT in Patients with Cardiovascular Disease
- Oxidizing chemicals in smoke likely contribute to an increased risk of thrombotic complications and reduction in nitric oxide availability.4 Unlike cigarette smoking, NRT does not cause platelet aggregation or thrombotic complications.15
- Transdermal nicotine in smokers with known coronary artery disease (CAD) has been shown to cause no significant differences in heart rate, in blood pressure, or in duration or frequency of ischemic episodes on ambulatory ECG monitoring.16
- NRT use was not associated with an increased risk of adverse cardiovascular events in the first year after acute coronary syndrome (ACS).17
- The use of nicotine gum did not increase cardiovascular deaths or hospitalizations, even in patients who smoked while using NRT and/or used NRT for more than a year.18
- Stress testing in smokers with known CAD showed that addition of a nicotine patch improved exercise tolerance and decreased ischemia, despite continued smoking and increased serum nicotine levels. The reduction in ischemia correlated with reduced exhaled carbon monoxide levels, as the subjects spontaneously reduced their smoking while wearing the nicotine patches.19,20 This clearly shows that smoking while wearing a nicotine patch is not dangerous.
- NRT use in high-risk smokers hospitalized with ACS or decompensated heart failure was safe and was associated with a decrease in readmissions and a decrease in all-cause mortality.21
- The American Heart Association and the American College of Cardiology support the use of NRT to aid in smoking cessation in patients with atherosclerotic vascular disease.22–24
Assessing Nicotine Dependence
- An estimate of a person’s dependence on nicotine can guide dosing of NRT. Plasma levels of nicotine and cotinine vary from person to person, and only weakly correlate with the number of cigarettes smoked per day. A study in regular smokers found that among 1 pack per day (ppd) smokers, plasma cotinine levels varied 74-fold.25
- Highly dependent persons smoke within 30 minutes of waking and typically smoke >one-half ppd.
- Persons with low nicotine dependence wait more than 30 minutes for the first cigarette of the day and usually smoke <1 ppd.
- Highly dependent persons smoke within 30 minutes of waking and typically smoke >one-half ppd.
- On an adequate dose of NRT, the patient will still have cravings but should feel relatively comfortable between cravings. If the NRT dose is too low, the patient will experience ongoing withdrawal symptoms and strong cravings. If the dose is too high, the patient will experience symptoms of nicotine overdose.
Specific Products
- Nicotine gum (polacrilex) is available over the counter in 2-mg and 4-mg strengths; the 4-mg strength is recommended for those who smoke more than 1 ppd and/or smoke within 30 minutes of awakening.
- The nicotine is absorbed only through the buccal mucosa, and absorption is decreased by acidic beverages, so the patient should be instructed not to eat or drink while chewing the gum or 15 minutes before. Eating or drinking or rapid chewing will cause the nicotine to be swallowed, and it will cause heartburn, hiccups, or dyspepsia.
- The gum should be chewed slowly until a peppery taste emerges, then left between the cheek and gum for buccal absorption. The gum should be chewed slowly and intermittently for approximately 30 minutes or until the taste dissipates.
- It takes several minutes for the nicotine to reach the bloodstream, so there will not be the immediate satisfaction of smoking.
- Patients will be more successful if they use at least 9 pieces a day.26,27 They should use it on a fixed schedule, one piece every 1 to 2 hours for at least 1 to 3 months, then start to slowly taper the number of pieces per day (one piece per day every 4 to 7 days). The maximum daily dose is 24 pieces. Common side effects include mouth soreness, dyspepsia, and hiccups.
- The nicotine is absorbed only through the buccal mucosa, and absorption is decreased by acidic beverages, so the patient should be instructed not to eat or drink while chewing the gum or 15 minutes before. Eating or drinking or rapid chewing will cause the nicotine to be swallowed, and it will cause heartburn, hiccups, or dyspepsia.
- Nicotine lozenges are available over the counter in 2-mg and 4-mg strengths; the 4-mg strength is recommended for those who smoke within 30 minutes of awakening.
- Similar to the nicotine gum, the nicotine is absorbed through the buccal mucosa, so patients must not eat or drink while using it.
- Patients will be more successful if they use at least 9 pieces a day: 1 piece every 1 to 2 hours for at least 1 to 3 months, then taper off. The maximum daily dose is 24 pieces. Side effects include mouth soreness, dyspepsia, and hiccups.
- Similar to the nicotine gum, the nicotine is absorbed through the buccal mucosa, so patients must not eat or drink while using it.
- Nicotine patches are available over the counter in several strengths, typically 21, 14, or 7 mg/day.
- Most patients should start with the strongest patch, unless they smoke <10 cigarettes/day and wait more than 30 minutes to smoke after awakening. The highest strength patch is used for 2 to 6 weeks, then the intermediate strength for 2 weeks, and then the lowest strength for 2 weeks.
- Highly dependent smokers may need 2 or more full-strength patches for adequate replacement therapy.
- Each morning, a patch should be placed on a relatively hairless location on the trunk or upper arm (hair may be shaved). Locations should be rotated to minimize skin irritation. Hands should be washed after handling patches. The used patch should be folded in half and thrown away out of reach of children and pets.
- Patches either may be used overnight to minimize morning cravings or may be taken off at bedtime to minimize insomnia and vivid dreams. If the patch is not worn overnight, morning withdrawal symptoms may be treated with a faster-acting form of nicotine.
- The most common side effects include insomnia and skin irritation. It is common to feel tingling under the patch for the first hour.
- Most patients should start with the strongest patch, unless they smoke <10 cigarettes/day and wait more than 30 minutes to smoke after awakening. The highest strength patch is used for 2 to 6 weeks, then the intermediate strength for 2 weeks, and then the lowest strength for 2 weeks.
- Nicotine nasal spray is available by prescription only and is less popular with patients (expensive and awkward to use).
- The spray has a faster onset of action than the gum or patch and therefore has greater potential for dependence.
- The most common side effect is nasal irritation, which can be minimized by avoiding sniffing or inhaling while administering.
- Patients should use one spray in each nostril (for a total dose of 1 mg) and should use 1 to 2 doses/hour with a maximum of 40 doses/day.
- The spray has a faster onset of action than the gum or patch and therefore has greater potential for dependence.
- Nicotine inhalers are available by prescription only and are also less popular with patients (expensive and awkward to use).
- Each cartridge delivers 4 mg nicotine over 80 inhalations. Patients should use 6 to 16 cartridges daily for up to 6 months. The vapor is absorbed in the mouth and throat and has a fairly fast onset of action. The inhaler is puffed frequently for 20 minutes (much more frequently than a cigarette).
- Because the nicotine is absorbed only through the buccal mucosa and absorption is decreased by acidic beverages, the patient should be instructed not to eat or drink while using the inhaler or 15 minutes before.
- The most common side effects are irritation of the mouth and throat, coughing, dyspepsia, and rhinitis.
- Each cartridge delivers 4 mg nicotine over 80 inhalations. Patients should use 6 to 16 cartridges daily for up to 6 months. The vapor is absorbed in the mouth and throat and has a fairly fast onset of action. The inhaler is puffed frequently for 20 minutes (much more frequently than a cigarette).
Nonnicotine Medications
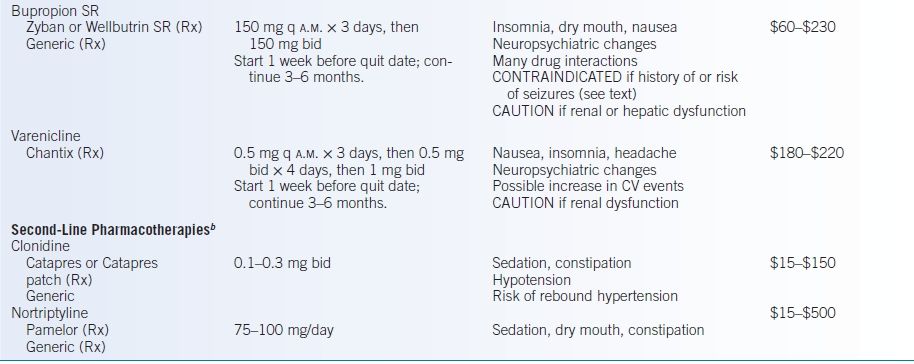
Bupropion
- Bupropion SR is thought to work by enhancing dopaminergic activity in the central nervous system.
- In randomized controlled trials, subjects treated with bupropion SR had abstinence rates of about twice that of the placebo group.28 Efficacy is independent of a history of depression.
- Bupropion SR should be started 1 to 2 weeks before the quit date at 150 mg each morning for 3 days, then 150 mg twice daily for 7 to 12 weeks. Evening dosing may lead to insomnia so the second dose should be in the late afternoon. A lower dose of 150 mg once daily may be as effective as twice-daily dosing.29
- Studies have used bupropion for 7 to 52 weeks. Longer duration was associated with delay and attenuation of relapse and weight gain.30
- The most common side effects are insomnia (about 20%), dry mouth, and nausea.
- Due to a risk of seizures (approximately 1 in 1,000), bupropion SR should not be used in patients with a history of seizure, head trauma, and brain tumor; in those with anorexia/bulimia and hepatic failure; or in those using drugs that may increase the risk of seizures (theophylline, systemic steroids, antipsychotics, antidepressants, hypoglycemics/insulin, or abuse of alcohol or stimulants).
- Bupropion SR is contraindicated in patients with use of a monoamine oxidase inhibitor within 14 days.
- In 2008, the U.S. Food and Drug Administration (FDA) warned of neuropsychiatric symptoms and suicidal events, even in individuals with no history of psychiatric disease, based on postmarketing reports.31 Patients should be monitored for changes in behavior, hostility, agitation, depressed mood, or suicidal ideation.
Varenicline
- The newest medication approved for smoking cessation is varenicline, a partial nicotine agonist. It binds to the α4β2-nicotinic acetylcholine receptors, stimulating dopamine release to reduce craving and withdrawal symptoms while also blocking binding of nicotine to reduce the reinforcing effects of smoking (satisfaction).
- Varenicline has been shown to more than double the placebo quit rate and may be more effective than bupropion.4,32,33

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


