CHAPTER 66 Small intestine
DUODENUM
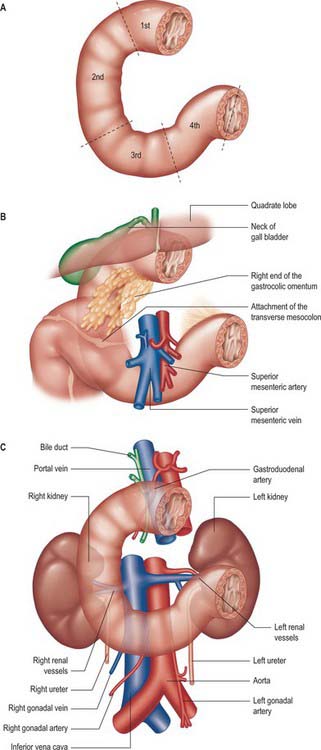
The adult duodenum is 20–25 cm long and is the shortest, widest and most predictably placed part of the small intestine. It is only partially covered by peritoneum, although the extent of the peritoneal covering varies along its length: the proximal 2.5 cm is intraperitoneal, and the remainder is retroperitoneal. The duodenum forms an elongated ‘C’ that lies between the level of the first and third lumbar vertebrae in the supine position. The lower ‘limb’ of the C extends further to the left of the midline than the upper limb. The head and uncinate process of the pancreas lie within the concavity of the duodenum which is ‘draped’ over the prominence formed from the lumbar spine, the duodenum therefore bends in an antero-posterior direction as well as following the form of a ‘C’. The duodenum lies entirely above the level of the umbilicus and is described as having four parts (Figs 66.1, 66.2).
FIRST (SUPERIOR) PART
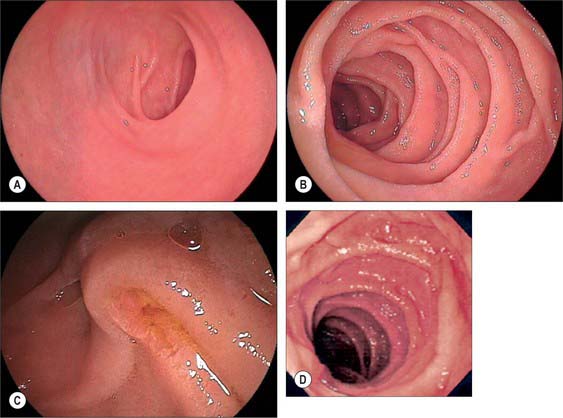
The first, and most mobile, part of the duodenum is about 5 cm long. It starts as a continuation of the duodenal end of the pylorus and ends at the superior duodenal flexure. Peritoneum covers the anterior and superior part of its posterior aspect close to the pylorus, where the duodenum forms part of the anterior wall of the epiploic foramen. Here the lesser omentum is attached to its upper border and the greater omentum to its lower border. The first 2 or 3 cm have a bland internal mucosal appearance and readily distend on insufflation during endoscopy. This part is frequently referred to as the duodenal ‘cap’. It has a triangular, homogeneous appearance during contrast radiology, shows the same pattern of internal rugae as the pylorus, and is often visible on plain radiographs of the abdomen as an isolated triangular gas shadow to the right of the first or second lumbar vertebra. The duodenum next passes superiorly, posteriorly and laterally for 5 cm before curving sharply inferiorly into the superior duodenal flexure: it rapidly becomes more retroperitoneal during this part of its course, until peritoneum only covers its anterior aspect. From the end of the duodenal cap, its internal appearance is characterized by extensive, deep mucosal folds that involve up to half of the circumference of the lumen. Even during endoscopic insufflation, these folds are pronounced (Fig. 66.3) and they are readily seen on contrast radiographs. The section from the duodenal cap to the superior duodenal flexure lies posterior and inferior to the quadrate lobe of the liver.
SECOND (DESCENDING) PART
The second part lies anterior to the hilum of the right kidney, the right renal vessels, the edge of the inferior vena cava and the right psoas major. The head of the pancreas and the common bile duct are medial and the hepatic flexure is above and lateral. A small part of the pancreatic head is sometimes embedded in the medial duodenal wall, and pancreatic ‘rests’ in the duodenal wall may produce small filling defects on contrast radiology. The internal appearance is similar to that of the distal portion of the first part of the duodenum, with pronounced mucosal folds (Fig. 66.3). The common bile duct and pancreatic duct enter the medial wall obliquely and usually unite to form the common hepatopancreatic ampulla. The narrow distal end opens on the summit of the major duodenal papilla (ampulla of Vater), which is situated on the posteromedial wall of the second part, 8–10 cm distal to the pylorus. There are variants of the ductal anatomy. The most common is a second, accessory pancreatic duct which may open 2 cm above the major papilla on a minor duodenal papilla. Peptic ulceration of the second part of the duodenum is less common than that of the first part, and tends to occur on the anterior or lateral wall.
FOURTH (ASCENDING) PART
The fourth part of the duodenum is 2.5 cm long. It starts just to the left of the aorta, runs superiorly and laterally to the level of the upper border of the second lumbar vertebra, then turns sharply anteroinferiorly at the duodenojejunal flexure to become continuous with the jejunum. The main trunk of the inferior mesenteric vein lies either posterior to the duodenojejunal flexure or beneath the adjacent peritoneal fold. (The duodenojejunal flexure is a useful landmark to locate the vein radiologically or surgically.) The aorta, left sympathetic trunk, left psoas major, left renal and left gonadal vessels are all posterior relations, the left kidney and left ureter are posterolateral, and the upper part of the root of the small bowel mesentery, the left lateral transverse mesocolon and transverse colon, which separate it from the stomach, are anterior. The peritoneum of the root of the small bowel mesentery continues over its anterior surface. The lower border of the body of the pancreas is superior.
At its left lateral end, the fourth part becomes progressively covered in peritoneum on its superior and inferior surfaces, such that it is suspended from the retroperitoneum by a double fold of peritoneum, the ligament of Treitz, at the start of the duodenojejunal flexure. The ligament of Treitz may contain a small slip of muscle, the suspensory muscle of the duodenum. When present, the suspensory muscle contains skeletal muscle fibres that run from the left crus of the diaphragm to connective tissue around the coeliac axis, and smooth muscle fibres that run from the coeliac axis: its function is unknown. It is an important landmark in the radiological diagnosis of incomplete rotation and malrotation of the small intestine (see Ch. 73). The ligament of Treitz does not form part of the duodenal mesentery because the vascular supply to the fourth part of the duodenum continues to enter its wall from the posteromedial aspect.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Arteries
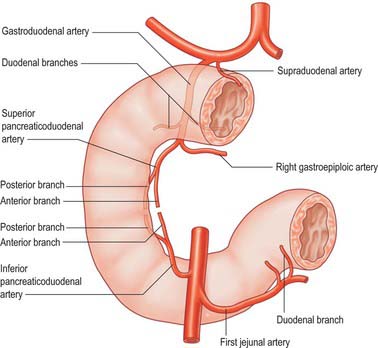
The main vessels supplying the duodenum are the superior and inferior pancreaticoduodenal arteries. The first and second parts also receive contributions from several sources including the right gastric, supraduodenal, right gastroepiploic, hepatic and gastroduodenal arteries. Branches of the superior pancreaticoduodenal artery may contribute to the supply of the pyloric canal, with a minor degree of anastomosis to the gastric arteries in the muscular layer across the pyloroduodenal junction (Fig. 66.4).
Superior pancreaticoduodenal arteries
The superior pancreaticoduodenal artery is usually double. The anterior artery is a terminal branch of the gastroduodenal artery and descends in the anterior groove between the second part of the duodenum and the head of the pancreas. It supplies branches to the first and second parts of the duodenum and to the head of the pancreas, and anastomoses with the anterior division of the inferior pancreaticoduodenal artery. The posterior artery is usually a separate branch of the gastroduodenal artery and is given off at the upper border of the first part of the duodenum. It descends to the right, anterior to the portal vein and common bile duct as the latter lies behind the first part of the duodenum. It then runs behind the head of the pancreas, crosses posterior to the common bile duct (which is embedded in the head of the pancreas), enters the duodenal wall and anastomoses with the posterior division of the inferior pancreaticoduodenal artery. The posterior artery supplies branches to the head of the pancreas, the first and second parts of the duodenum, and several branches to the lowest part of the common bile duct.