APAP, autotitrating positive airway pressure; CPAP, continuous positive airway pressure.
Surgical Management
- Patients who want to consider surgery for OSA should be evaluated by an otolaryngologist to determine whether the area of upper airway obstruction is amenable to surgery.
- Tracheotomy can be curative for OSA, as the area of upper airway obstruction is bypassed.
- Uvulopalatopharyngoplasty is a common surgery performed for OSA. Response to surgery varies from 40% to 60% depending upon how surgical success is defined. Patients with higher AHIs are less likely to respond. Complications can include voice changes, foreign body sensation, and nasal reflux.20
- Laser-assisted uvulopalatoplasty differs from uvulopalatopharyngoplasty in that the tonsils and pharyngeal pillars are not excised. Currently, the recommendations for use of laser-assisted uvulopalatoplasty are only in primary snoring, not OSA.21
- Patients being considered for surgical treatment for snoring or OSA should undergo evaluation with overnight polysomnogram prior to surgery. If OSA is present on the baseline study, a postsurgical polysomnogram should be performed to document resolution of the OSA.22
- OSA may improve with weight loss following bariatric surgery.
Lifestyle/Risk Modification
- Weight loss should be encouraged.
- Patients should limit alcohol, sedatives, and narcotics.
- Driving precautions should be discussed with patients.
Insomnia
GENERAL PRINCIPLES
- Insomnia is the inability to initiate or maintain sleep.
- While approximately one-third of the general population has experienced insomnia at some point, of those patients with severe insomnia, approximately 80% have reported symptoms for more than a year.23
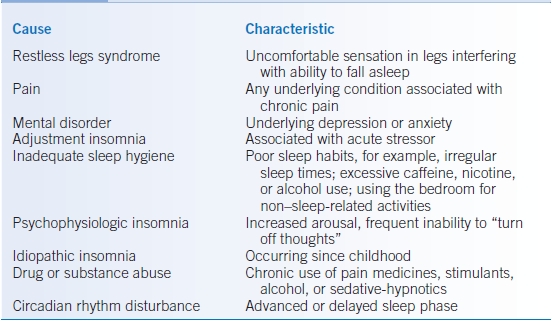
- See Table 18-2 for causes of insomnia and associated characteristics.
- Risk factors for insomnia depend upon the underlying cause, but can include depression, anxiety, acute life stressors, stimulant use, withdrawal from sedating drugs, or poor sleep hygiene.
- Following good sleep hygiene techniques can prevent insomnia. Good sleep hygiene consists of activities such as maintaining a regular sleep schedule, avoiding stimulants (caffeine and nicotine) close to bedtime, and avoiding reading or watching TV in bed. Treatment of conditions such as depression and anxiety may also help to prevent insomnia.
- Insomnia may be triggered by depression and anxiety. However, insomnia may also worsen depression and anxiety.
- Patients with insomnia may exhibit increased irritability, difficulty concentrating, and complaints of somatic pain.
TABLE 18-2 Causes of Insomnia and Associated Characteristics
DIAGNOSIS
Clinical Presentation
- Patients report difficulty with initiating and/or maintaining sleep.
- Patients may report racing thoughts that prevent them from sleeping.
- Often, patients are fatigued, but not overtly sleepy during the day.
- Elicit any history of use of medications or drugs that can contribute to insomnia or confounding medical conditions such as chronic pain, RLS, depression, or anxiety.
- In addition, the history should be directed to evaluate the patient’s sleep schedule and to assess for poor sleep hygiene.
- There are no specific physical exam findings for insomnia.
Diagnostic Criteria
- In general, a patient should complain of difficulty initiating and/or maintaining sleep that is associated with perceived limitation in daytime functioning such as fatigue, poor concentration, or irritability. There should be adequate opportunity for sleep.
- More specific criteria depend upon the cause of the insomnia.
Differential Diagnosis
Patients with paradoxical insomnia or sleep state misperception feel they suffer from insomnia. However, objective testing such as polysomnogram or actigraphy demonstrates normal sleep time and pattern. Often, their daytime impairment is less severe than patients with insomnia.
Diagnostic Testing
- If there is clinical concern, a polysomnogram can be performed to rule out other causes of poor sleep maintenance, such as periodic limb movements or sleep-disordered breathing.
- Actigraphy can be used to confirm reported sleep patterns and sleep times.
- Urine drug screen can be used to screen for use of illicit drugs that may trigger insomnia.
TREATMENT
Medications
- Over-the-counter medications are frequently used by patients to treat insomnia. Table 18-3 lists common over-the-counter medications and their potential side effects. There are no strong data to support the efficacy of these agents.24
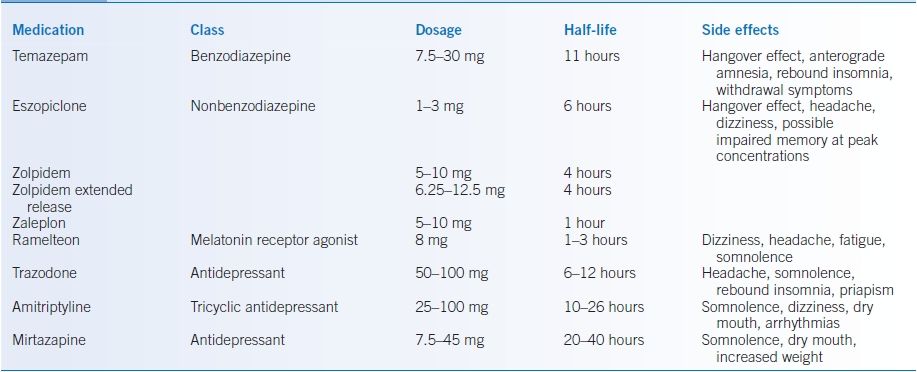
- The prescription medications that are approved for treatment of insomnia are the benzodiazepine receptor agonists and the melatonin receptor agonists. Of these, eszopiclone (nonbenzodiazepine hypnotic) and ramelteon (melatonin agonist) are the only ones FDA approved for long-term use. The benzodiazepine receptor agonists are considered controlled substances, whereas the melatonin receptor agonists are not.24
- Frequently, sedating antidepressants are also prescribed for insomnia in off-label use, although data supporting their use are lacking. Table 18-4 outlines the prescription medications for insomnia as well as some of the potential side effects.24
- Treatment of underlying medical or psychiatric conditions potentially contributing to insomnia should be instituted.
TABLE 18-3 Over-the-Counter Medications for Insomnia and Their Side Effects
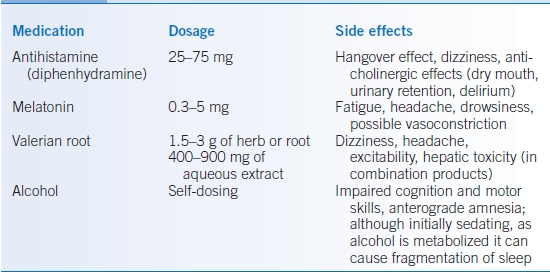
TABLE 18-4 Prescription Medications Used for Insomnia
Other Nonpharmacologic Therapies
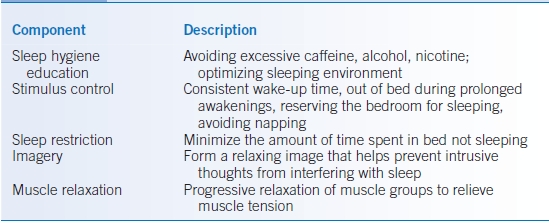
- Cognitive-behavioral therapy (CBT) encompasses a wide variety of techniques aimed at breaking the cycle of insomnia.25 Table 18-5 describes various components of CBT for insomnia.
- CBT has been shown to be beneficial in improving the nighttime and daytime symptoms associated with insomnia.26–28
TABLE 18-5 Components of Cognitive-Behavioral Therapy for Insomnia
Lifestyle/Risk Modification
- Patients should be encouraged to keep a regular sleep schedule with a consistent bedtime and waking time.
- Patients should avoid the use of stimulants such as caffeine and nicotine.
- Patients should modify their sleeping environment to minimize environmental disturbances.
- Patients should avoid activities such as watching TV or reading in bed.
Restless Legs Syndrome
GENERAL PRINCIPLES
- RLS consists of an uncomfortable sensation in the extremities (most commonly the legs), which is worse in the evening and nighttime, but can occur during the day in sedentary situations, and is temporarily relieved by movement.
- Prevalence of RLS is estimated to be between 2.5% and 15% of the population. In some patients with RLS, there is a hereditary link.29
- The severity of symptoms can be highly variable.
- The role of dopamine in RLS has been most strongly supported by the improvement of symptoms with dopamine agonists.30
- Iron is necessary for the rate-limiting step in dopamine synthesis. Therefore, low iron levels may decrease dopamine synthesis.31 Ferritin levels <50 μg/L have been associated with increased severity of RLS. Iron supplementation is recommended in the setting of RLS when ferritin is <50 μg/L.32
- RLS can be associated with other underlying conditions such as pregnancy, uremia, and anemia.
- Pharmacologic agents such as caffeine, nicotine, alcohol, dopamine antagonists, diphenhydramine, serotonin reuptake inhibitors, and tricyclic antidepressants may worsen RLS.33 Avoiding pharmacologic agents associated with RLS may help prevent symptoms.
DIAGNOSIS
Clinical Presentation
- Patients will report an uncomfortable sensation in the legs, which can sometimes involve the arms. Typically, the sensation is bilateral. If a patient reports mainly unilateral symptoms, consideration should be given to the possibility of a spinal cord lesion.
- The sensations should have a circadian rhythm to them in that they are worse in the late evening and earlier part of the night. However, some patients experience symptoms during the day when in prolonged sedentary situations.
- The sensations are typically temporarily relieved by movement, but return upon cessation of the movement.
- There are no specific physical exam findings for RLS.
Diagnostic Criteria
- RLS is a clinical diagnosis in which the four essential criteria, as outlined in Table 18-6, are met.34
- Periodic limb movements are frequently seen on the polysomnograms of patients with RLS, although a polysomnogram is not required to make the diagnosis of RLS.
- RLS is a clinical diagnosis. However, a polysomnogram can be performed if the presence of periodic limb movements would change therapy.
- A ferritin should be checked to evaluate if iron supplementation may be beneficial.
TABLE 18-6 Clinical Criteria for Restless Legs Syndrome
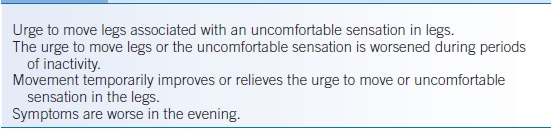
Data from Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 2003;4:101–119.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


