Overview
The overwhelming majority of occupational skin disorders are dermatitic
It is a major error to rely solely on the pattern of hand dermatitis when considering a diagnosis
Understanding the precise nature of a person’s job is essential (what do they do and how do they do it?)
Patch testing is the only objective method of assessing a dermatitis; it should be undertaken when assessing any persistent hand dermatitis
Delays in diagnosis predispose to chronicity; early referral to a specialist is important
Skin disorders are among the most often encountered problems in the occupational health setting, and although there are many dermatoses that have occupational relevance, the overwhelming majority are dermatitic. Occupations considered to be at greatest risk include hairdressing, nursing and similar healthcare, engineering (soluble coolant exposure) and food preparation.
Contact Dermatitis
In current terminology, the term ‘dermatitis’ is used synonymously with ‘eczema’ and describes inflammatory reactions in the skin with a spectrum of clinical and histopathological characteristics.
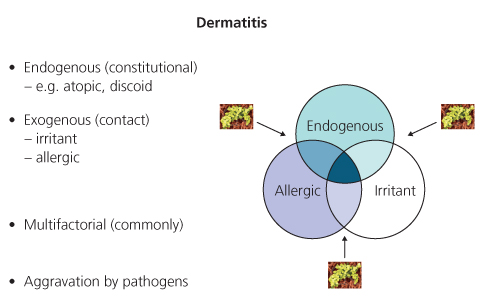
A dermatitis (Figure 10.1) may be entirely endogenous (constitutional) or be entirely exogenous (contact). The latter consists of irritant and allergic contact reactions. Commonly, a dermatitis has a multifactorial aetiology and may be aggravated by the presence of pathogens (Staphylococcus aureus). Assessment of the relative importance (contribution) of the possible factors can be difficult and subjective.
Atopic hand dermatitis and vesicular hand dermatitis are examples of endogenous conditions.
- From the distribution and morphology of a dermatitis on the hands it is not possible to be definitive about the aetiology, e.g. a vesicular hand dermatitis with a ‘classical’ endogenous distribution may be mimicked by an allergic contact dermatitis to isothiazolinone biocides or chromate sensitivity.
- It is a major error to rely on patterns of hand dermatitis in making a diagnosis.
An occupational dermatitis is one where the inflammatory reaction is caused entirely by occupational contact factors or where such agents contribute to the reaction on a compromised skin, i.e. they are partially responsible.
In the majority of cases, an occupationally related dermatitis will affect the hands alone. There may be spread onto the forearms. Occasionally the face may be the prime site of involvement (e.g. airborne); other sites may be involved.
Occupational dermatitis may be suspected when:
- dermatitis first occurred while employed
- history of aggravation by work
- there may be, at least initially, improvement (or clearance) when not at work
- exposure to irritant factors or potential allergens
- work in an ‘at risk’ occupation.
Irritant contact dermatitis is initiated by direct chemical or physical damage to the skin. All individuals are susceptible to the development of an irritant contact dermatitis if exposure to the irritant (toxic) agent(s) is sufficient. It occurs particularly where the stratum corneum is thinnest. Hence, it is often seen in the finger webs and back of the hands rather than the palms. There are two principal types of irritant contact dermatitis—acute (Figure 10.2) and chronic (Figure 10.3). The former is caused by exposure to an agent(s) causing early impairment in stratum corneum function followed by an inflammatory reaction. The latter by repeated exposure to the same or different factors resulting in ‘cumulative’ damage until an inflammatory reaction ensues which persists for a prolonged period even after further exposure is stopped. Those with a previous history of atopic eczema, and especially atopic hand eczema, are at particular risk of developing a chronic irritant contact dermatitis. A chronic irritant contact dermatitis is particularly observed where ‘wet work’ is involved.
Figure 10.2 Acute dermatitis.
Severity of reaction depends on ‘dose’ of irritant agent.
‘Chapping’ can be considered a minor form with a ‘chemical burn’ (e.g. cement burn) an extreme event.
Intermediate eczematous reactions are common, minor reactions are very common.
May occur on the face, e.g. low humidity occupational dermatosis, airborne irritant vapours.
Once the irritant factor(s) have been removed, resolution is usually spontaneous without important sequelae.

Figure 10.3 Chronic dermatitis.
Persistent dermatitis and the most common cause of continued disability from occupational skin disease.
Problem continues for long periods even with avoidance of aggravating factors.
Re-exposure to even minor irritant factors may cause a rapid flare.
After apparent healing there may be a prolonged increased susceptibility to recurrence of a dermatitis following irritant exposure.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree