Skeleton19
4.1. Skeleton
Bony skeleton (Fig. 4.1)
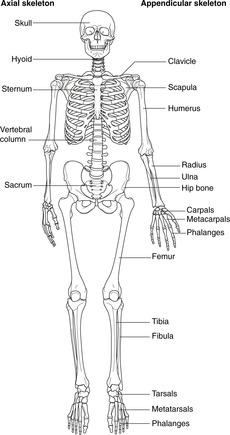
Fig. 4.1
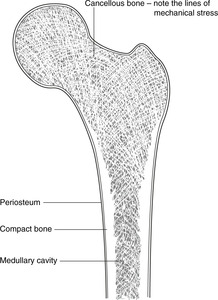
Section through bone (Fig. 4.2)
Parts of a long bone
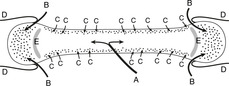
Arterial supply of a long bone (Fig. 4.3)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Skeleton and muscle
4.2 Joints21
4.3 Muscle23
Skeletal tissue exists for mechanical support. The structure and rigidity of bone reflect its weightbearing function and it is well supplied with blood. Bone formation (ossification) occurs in two ways: direct from membrane, and by means of a cartilaginous precursor. Ossification is not complete until late adolescence, thus allowing bone growth to take place. Joints can be classified as non-synovial (limited movement) and synovial (extensive movement). Another function of bone is the manufacture of blood cells (haemopoiesis). Skeletal muscle (histologically striated) is supplied by voluntary nerve impulses. Smooth muscle is supplied by involuntary nerve impulses. Cardiac muscle, although striated, has intrinsic contractility and is supplied by involuntary nerves.
You should:
• list the functions of cartilage and bone
• describe the blood supply of bone and how bone grows
• list the different types of joints and their relative mobility
• list the different characteristics of skeletal, smooth and cardiac muscle
• explain that skeletal muscles work in groups that usually share a common nerve supply.
Cartilage and bone provide mechanical support. Cartilage is more flexible than bone but confers insufficient rigidity to withstand gravity (large cartilaginous creatures are aquatic, where gravity matters less). Some cartilages remain more or less the same throughout life, while others undergo a gradual conversion to bone – ossification – which takes place before birth or during childhood and adolescence.
• Axial skeleton: skull, hyoid, vertebral column (including the sacrum), ribs, and sternum.
• Appendicular skeleton: pectoral and pelvic girdles, limb bones:
– pectoral girdle: clavicle, scapula
– upper limb: humerus, radius, ulna, carpal bones, metacarpals, phalanges
– pelvic girdle: hip bone (ilium, ischium, pubis)
– lower limb: femur, tibia, fibula, tarsal bones, metatarsals, phalanges.
Sesamoid bones are bones that develop in tendons as they cross joints. The patella is an example, and there are others in the wrist and the feet.
Important terms are:
• Cortical or compact bone: dense bone around the edges.
• Cancellous, trabecular or spongy bone in which the lines of mechanical stress are evident in the structure of the bone.
• Periosteum: the membranous covering. It has two layers: outer fibrous and inner cellular. The inner layer is vascular and contains stem cells which can when required differentiate into osteoblasts, for example in healing and repair. Damage to periosteum impairs bone healing.
• The medullary (marrow) cavity. This and the spaces in cancellous bone contain haemopoietic (blood-forming) cells; there is therefore a profuse arterial supply.
• Head: one end, usually the proximal.
• Neck: the area immediately distal to the head.
• Condyles: rounded articular surfaces.
• Epicondyles: prominences adjacent to condyles.
• Epiphysis: the name given to the developing ends of a long bone (see later).
• A large nutrient artery enters through the nutrient foramen (Fig. 4.3A). Branches of this reach the ends of a mature long bone, but not of a developing long bone (see below).
• Capsular (retinacular) vessels enter the bone with the attachments of the joint capsule (Fig. 4.3B).
• Many small arteries penetrate the periosteum directly, particularly at the site of muscular attachments and near joints (Fig. 4.3C).
• Bones have a particularly rich blood supply because haemopoiesis (formation of blood components) takes place in the central marrow cavity.