Sjogren Syndrome
Kevin R. Torske, DDS, MS
Lester D. R. Thompson, MD
Key Facts
Terminology
Reactive, focal to diffuse lymphoid infiltrate of salivary glands leading to parenchymal atrophy and degeneration of glandular elements into irregular epithelial complexes
Primary SS: Chronic, systemic autoimmune disease primarily affecting parotid and lacrimal glands
Secondary SS: Above in association with another autoimmune disorder
Clinical Issues
Mean age: 5th-7th decades
Female > > > Male (9:1)
Lacrimal and parotid glands most severely affected, commonly bilateral
Recurrent, firm, diffuse parotid enlargement lasting weeks to months, with occasional remission
Typically painless, bilateral swellings of lateral orbital margin
Diagnosis based upon results of multiple tests
Positive anti-SS-A (RO) &/or anti-SS-B (LA)
Rheumatoid factor positive in up to 95%
Treatment mostly supportive
44x increased risk of developing lymphoma
Image Findings
MR sialography is best diagnostic study
Microscopic Pathology
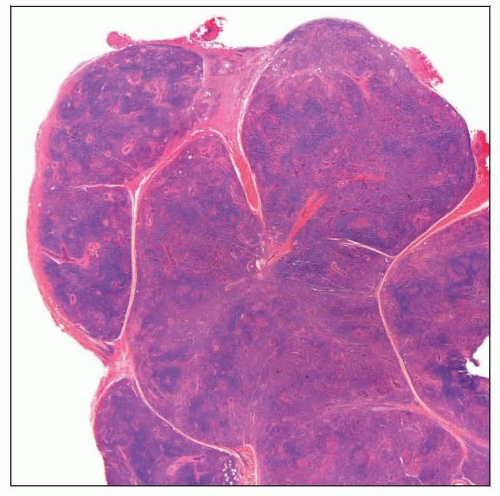
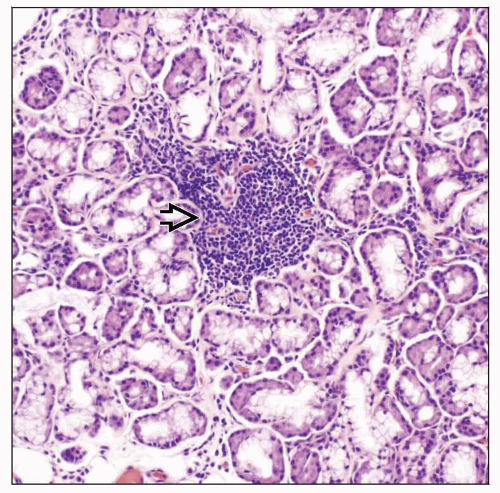
Minor salivary glands with lymphocytic and plasma cell infiltrate
Lymphoid aggregate = ≥ 50 lymphocytes
Lymphocytic infiltration, acinar atrophy, and formation of epimyoepithelial islands
TERMINOLOGY
Abbreviations
Sjögren syndrome (SS)
Synonyms
Mikulicz disease, Sicca syndrome
Definitions
Primary SS: Chronic, systemic autoimmune disease primarily affecting parotid and lacrimal excretory glands, leading to xerostomia and xerophthalmia, respectively
Secondary SS: Above in association with another autoimmune, connective tissue disorder
Typically rheumatoid arthritis or systemic lupus erythematosus
ETIOLOGY/PATHOGENESIS
Primary SjöGren Syndrome
Etiology unknown, yet likely multifactorial and complex
Endocrine: Systemic and local androgen deficiencies
Genetics
1° SS associated with HLA-B8 and HLA-Dw3
2° SS associated with HLA-DRw4
Viral infection: EBV, Coxsackievirus, and HTLV-1
Autonomic nervous system
Blockage of receptor sites by antimuscarinic antibodies (anti-M3R)
Upregulation of INFα and β-cell activating factor
CLINICAL ISSUES
Epidemiology
Incidence
0.5-3% of population
May be undiagnosed in nearly half of affected patients
Age
Mean: 5th-7th decades
Peaks at menarche and menopause
Gender
Female > > > Male (9:1)
Males may be more common in juvenile presentation
Ethnicity
No racial predilection
Site
Lacrimal and parotid glands most severely affected
Commonly bilateral
Submandibular, sublingual, and minor salivary glands affected to lesser degree
Upper respiratory tract
Sinonasal mucosa, eustachian tube, and larynx
Multiple other organ systems possibly affected
Presentation
Xerostomia (dry mouth)
Typically noted after saliva production falls below 50% of normal
Taste alterations
Difficulties in speech and mastication
Possible burning sensation
Less frequently associated with
Dental caries
Dry, cracked lips, angular cheilitis
Fissured or depapillated tongue
Chronic candidiasis
Oral ulcerations
Xerophthalmia (dry eyes, keratoconjunctivitis sicca)
Pain and foreign body sensation
Photosensitivity, ocular fatigue
Redness, loss of visual acuity, filamentary keratitis
Parotid gland
Recurrent, firm, diffuse parotid enlargement lasting weeks to months, with occasional remission
Enlargement correlated with increased disease severity
Persistent swelling may indicate transformation into low-grade lymphoma
Possible discomfort/pain, which may increase with eating
Potential retrograde infections with suppuration from Stensen duct
Lacrimal gland
Typically painless, bilateral swellings of lateral orbital margin
Associated with chronic dacryoadenitis
Associated with infection (especially viral), sarcoidosis, Graves disease, and orbital inflammatory syndrome
Other presentations based upon affected system
Many patients have other connective tissue, autoimmune, or rheumatologic disorders
Diabetes, sarcoidosis, malnutrition, infection, alcoholism, bulimia
Medications can be related to disorder development
Laboratory Tests
Diagnosis based upon results of multiple tests
Ocular
Schirmer test: Decreased tear secretion
Rose bengal and lissamine green: Dyes used to examine eye surface for dry spots
Salivary flow tests (sialometry)
Serology
Positive anti-SS-A (RO) &/or anti-SS-B (LA)
Also autoantibodies for muscarinic receptor M3, IFI16, KLHL12, or KLHL7
Rheumatoid factor positive in up to 95%
Anti-nuclear antibody (ANA) positive in up to 80%
Erythrocyte sedimentation rate (ESR) usually elevated
Immunoglobulins: Usually elevated in SS patients
Treatment
Treatment mostly supportive
Xerostomia: Adequate hydration and stimulation of salivary flow
Topical stimulation: Sugar-free gum, candies, or lozenges
Systemic stimulation: Pilocarpine, cevimeline, bromhexine, tibolone
Xerophthalmia
Topical: Artificial tears, including eye drops or ointments
Systemic: Androgens (methyl-testosterone) or cyclosporine
Oral hygiene instruction, topical fluoride, and chlorhexidine rinses
Antifungal therapy for chronic candidiasis
Prognosis
Slowly progressive, evolving over decades
May wax and wane over time
Most serious complication is lymphoma development
44x increased risk of developing lymphoma
Approximately 4-10% of SS patients
Typically low grade
Extranodal marginal zone B-cell lymphoma (EMZBCL) of mucosa-associated lymphoid tissue (MALT) is most common
Represents approximately 85% of lymphomas in SS patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree