Sinonasal Melanoma
Lester D. R. Thompson, MD
Key Facts
Terminology
Neural crest-derived neoplasms originating from melanocytes and demonstrating melanocytic differentiation
Clinical Issues
Anterior nasal septum > maxillary sinus
Overall prognosis is poor
Macroscopic Features
Most are polypoid
Microscopic Pathology
Protean histology, mimic of many other primary tumor types
Junctional activity and epidermal migration (pagetoid spread) help to confirm primary tumor
Many patterns of growth
Variety of cell types can be seen
Prominent, irregular, brightly eosinophilic, enlarged nucleoli
Intranuclear cytoplasmic inclusions usually present
Melanin-containing tumor cells can be seen
Ancillary Tests
Positive: S100, HMB-45, MART-1/Melan-A, microphthalmia transcription factor, tyrosinase, vimentin
Top Differential Diagnoses
Olfactory neuroblastoma
Sinonasal undifferentiated carcinoma
Melanotic neuroectodermal tumor of infancy
Rhabdomyosarcoma
Metastatic melanoma
TERMINOLOGY
Synonyms
Mucosal malignant melanoma (MMM)
Sinonasal tract mucosal malignant melanoma (STMMM)
Definitions
Neural crest-derived neoplasms originating from melanocytes and demonstrating melanocytic differentiation
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Formalin
Possibly radiation
UV exposure
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Represents < 1% of all melanomas
< 5% of all sinonasal tract neoplasms
15-33% of all skin melanomas occur in head and neck
STMMM represent < 4% of all head and neck melanomas
Age
Wide age range, usually in 5th-8th decades
Gender
Equal gender distribution
Ethnicity
Increased incidence in Japanese patients
Site
About 15-20% of melanomas arise in head and neck
80% are cutaneous in origin
Ocular origin account for majority of remaining MMM
Sinonasal tract and oral cavity are next most common sites
Anterior nasal septum > maxillary sinus
Presentation
Nasal obstruction
Epistaxis or nasal discharge
Melanorrhea: Black-flecked (melanin) discharge
Polyp
Pain is uncommon
Treatment
Options, risks, complications
Metastatic melanoma to sinonasal tract can develop but is vanishingly rare
Breslow thickness and Clark level are not used in sinonasal tract
Surgical approaches
Wide local excision is treatment of choice
Radiation
Radiation can be used after surgery
In most cases, it is palliative
Prognosis
Overall prognosis is poor
5-year survival: 17-47%
Recurrences are common
Poor prognosis associated with
Obstruction as presenting symptom
Nasopharynx or “mixed site” of involvement
Tumor ≥ 3 cm
Undifferentiated histology
High mitotic count
Recurrence
Stage of tumor
Matrix metalloproteinases (MMPs: Proteolytic enzymes required for extracellular matrix degradation) expression may be associated with patient outcome
Decreased MMP2 expression associated with greater overall survival
Positive MMP14 expression associated with poor survival
IMAGE FINDINGS
Radiographic Findings
Usually identifies extent of tumor and bone invasion
Positron emission tomography (PET) tends to show posterior nasal cavity and sinus tumors better than anterior nasal tumors
Locoregional and metastatic disease can be detected
MACROSCOPIC FEATURES
General Features
Most are polypoid
White to gray, brown, or black
Surface ulceration/erosion is common
Size
Range up to 6 cm
Mean: 2-3 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Protean histology, mimic of many other primary tumor types
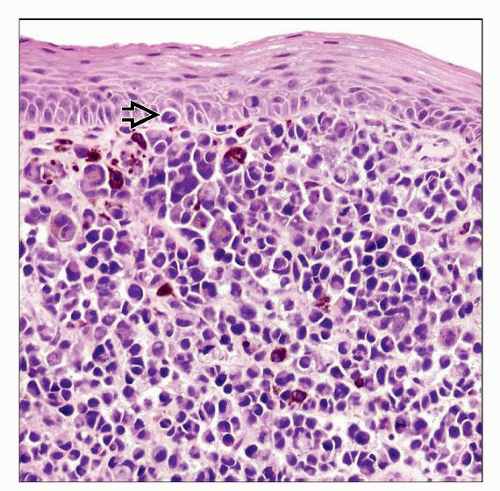
Junctional activity and intraepidermal migration (Pagetoid spread) help to confirm primary tumor
Surface ulceration is common, obscuring “in situ” component
Bone or soft tissue invasion is common
Many patterns of growth
Nests
Solid
Organoid
Sheets
Fascicles and interlacing bundles
Storiform
Meningothelial
Papillary
Hemangiopericytoma-like
Peritheliomatous: Distinctive and unique for STMMM
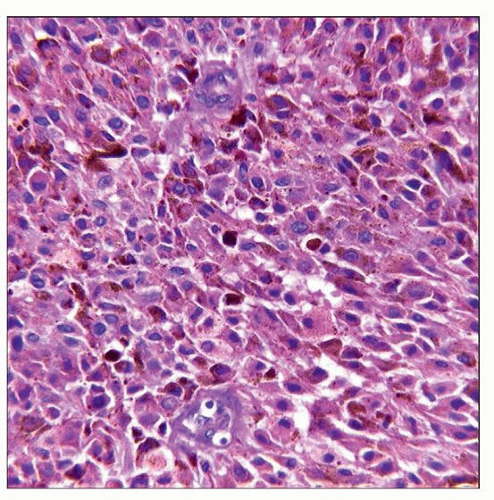
Variety of cell types can be seen
Undifferentiated
Epithelioid, polygonal
Small cell
Plasmacytoid
Rhabdoid
Giant cell
Vesicular nuclei, although sometimes hyperchromatic
Prominent, irregular, brightly eosinophilic, enlarged nucleoli
Intranuclear cytoplasmic inclusions usually present
Melanin-containing tumor cells can be seen
Tumor cell necrosis is common
Mitotic figures, including atypical forms, usually easily found
Inflammation may be present, but not of consequence
Desmoplastic type fibrosis can be seen, but is not common
Perineural invasion, when present, is poor prognostic indicator
Tumor depth of invasion (Clark) impossible to accurately assess
Tumor thickness (Breslow) not meaningful in sinonasal tract
Lymphatic/Vascular Invasion
Usually present but difficult to assess
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree