Steven Shoptaw, PhD, and Matthew Brensilver, PhD
40
DEFINITIONS
Current boundaries that define pathologic (and illegal) sexual behavior for an individual are easiest to set when the boundaries involve sexual partners who are children and sexual partners who are subjected to aggression by the individual. Outside legal sanctions against behaviors that involve pedophilia, rape, or sexual abuse, there are no agreed-upon cut points that distinguish “normal” from “pathologic” sexual behaviors.
Sexual compulsivity shares many stigmata of other addictive disorders defined by excessive consumption. Individuals affected by compulsive sexual behaviors commonly describe symptoms that parallel addiction to nicotine, alcohol, and illicit drugs. The parallels include repetitive, compulsive behaviors that impact on neurobiology, social environments, and the health of the individual. Similarly, the concept of sexual addiction includes clinically significant distress due to negative consequences of compulsive and impulsive sexual behaviors. By contrast, there are few measurable and reliable definitions of sexual addiction.
DIAGNOSIS
In trying to define the limits of pathologic sexual behaviors, two traditions dominate the nomenclature: psychiatry and addiction. Psychiatry has a long tradition of defining pathologic sexual behaviors (including a history of pathologizing homosexuality) and relies on terms like erotomania and paraphilia. The newer tradition is from addiction and relies on terms like sexual addiction, compulsive sexual behavior, and sexual impulsivity and emphasizes recovery and a neurobiologic basis of the disorder. Further complicating definitions, behaviors that may reflect sexual addiction can cross groups and engender different social reactions and censure.
An element defining significant clinical distress for nonparaphilic sexual disorders involves the large amounts of time to plan or engage in sexual behaviors, either alone or with partners. In this sense, sexual addictions have much in common with substance use disorders. Individuals complain of sexual behaviors that are repetitive, persistent, compulsive, and out of control, and when not engaged in the behaviors, individuals report obsessive thoughts about sex. Obsessive sexual thoughts in such individuals contributed to development of one heuristic model defining the disorder as a variant of obsessive–compulsive disorder. Negative self-evaluations are also part of the definition, including feeling abnormal or sick; feeling degraded, guilty, or ashamed; feeling regret, depression, or discomfort; or feeling numb, hollow, or empty.
As expected, problems in defining the disorder complicate efforts to determine the prevalence of the disorder. One notable attempt to achieve a prevalence estimate used a statistical cutoff as a proxy for sexually compulsive behavior by defining hypersexuality—among men—as persistence of seven or more orgasms per week for a minimum duration of 6 months or more after age 15. This definition characterizes between 3% and 8% of responses in nationally representative surveys of male sexual behavior in the United States. Research on women is largely lacking; important definitional differences across gender may exist.
ETIOLOGY
The quality of evidence supporting the etiology of sexual addiction is poor, with much of the literature based exclusively on theory. There are no indications in adolescence that clearly predict individuals who go on to develop sexual addiction in adulthood. There are, however, better data documenting trauma in the histories of individuals, especially women, who develop sexual addiction. It is plausible that sexual addiction is related to a broad externalizing behavior propensity, which may explain similarities to antisocial behavior and substance use disorders.
Some have examined whether genetics may explain high numbers of sexual partners. One group found that variation in the gene coding for dopamine transporter level, which impacts synaptic levels of dopamine, was associated with the number of sexual partners among men but not among women. Several studies found significant associations between genes regulating dopamine expression and sexual behaviors (mostly number of sexual partners), though with no clear pattern of findings. Links between dopamine availability and sexual behaviors are rational, but the available genetic data that might signal efforts to identify paraphilias or other sexual disorders are premature.
NEUROBIOLOGY OF SEXUAL ADDICTION
There exists a small literature on the neurobiology of sexual behavior, primarily among healthy males. Some of the neuroadaptations seen in substance dependence may exist in hypersexuality. Imaging studies have experimentally manipulated presentation of erotic and neutral stimuli among young adult male heterosexual subjects under positron emission tomography or functional magnetic resonance imaging. Erotic visual stimuli activate brain regions that include the right insula and claustrum (somatosensory processing and penile erection), the hypothalamus and striatum (areas of dopamine neurotransmission), and the anterior cingulate gyrus (shifting attention, repetitive behavior, endocrine and gonadal secretions), in addition to activation in the occipital cortex (visual processing). Oei et al. probed the role of dopaminergic tone in sexual response by randomizing healthy males to haloperidol, levodopa, or placebo. Levodopa enhanced activation in the nucleus accumbens and the dorsal anterior cingulate when participants were exposed to subconscious sexual stimuli, while haloperidol decreased activations in these areas. The role of dopamine in normal and aberrant sexual behavior has been suggested by high prevalence of impulse control disorders emerging in response to dopamine agonist treatment among those with Parkinson’s disease.
PSYCHIATRIC COMORBIDITY
Reports consistently implicate impulsivity, obsessions, and compulsivity as central issues in the expression of sexual addiction. Several psychiatric conditions share one or more of these features. In men with paraphilia and paraphilia-related disorders, psychiatric comorbidity is highly prevalent. In one sample (n = 88) of clinic-referred males diagnosed with paraphilias, 86% met criteria for any mood disorder, 46% met criteria for any anxiety disorder, and 49% met criteria for any substance abuse disorder. High prevalence of psychiatric comorbidities is also observed in community samples of individuals who defined their behavior as sexually compulsive. In one study (n = 36), 39% met criteria for lifetime mood disorders and 64% for lifetime substance abuse disorders. In another (n = 24), all subjects met lifetime criteria for any Axis I disorder (mood disorders, 71%; anxiety disorders, 96%). Fully 88% met criteria for any current Axis I disorders (mood disorders, 33%; anxiety disorders, 42%), with 29% and 71% who met criteria for any substance use disorder current and lifetime, respectively, and 46% met criteria for any personality disorder, predominantly cluster C. Among men who have sex with men, depression symptoms significantly correlate with reports of sexual compulsivity. Presence of anxiety symptoms also appears to be somewhat higher in individuals with behaviors consistent with sexual addiction as compared to controls. Some retrospective reports suggest associations between attention-deficit/hyperactivity disorder (ADHD) during childhood and presence of sexual addiction.
ASSESSMENT
Individuals who present to a clinician need careful evaluation to define the presenting problem and understand factors precipitating initiation of treatment. Individuals presenting for treatment of sexual addiction often have limited motivation for treatment themselves and rely on spouses, partners, or judges, who may place conditional demands on the individual. Thus, determining and enhancing intrinsic motivation often is an important element of treatment. After seeking a thorough understanding of the chief complaint, it is important to establish whether or not there is victimization in the history. Some forms of sexual compulsion (sexual contact with children) are legally reportable activities; others expose the patient to risk of arrest (sexual assault, public exhibitionism). Still others increase individual risks for viral infection or physical violence. Careful review of ways in which the sexual addiction impacted areas of functioning is crucial. Assessment of comorbid conditions is important, as is determining if the sexual behavior is better explained by another psychiatric condition.
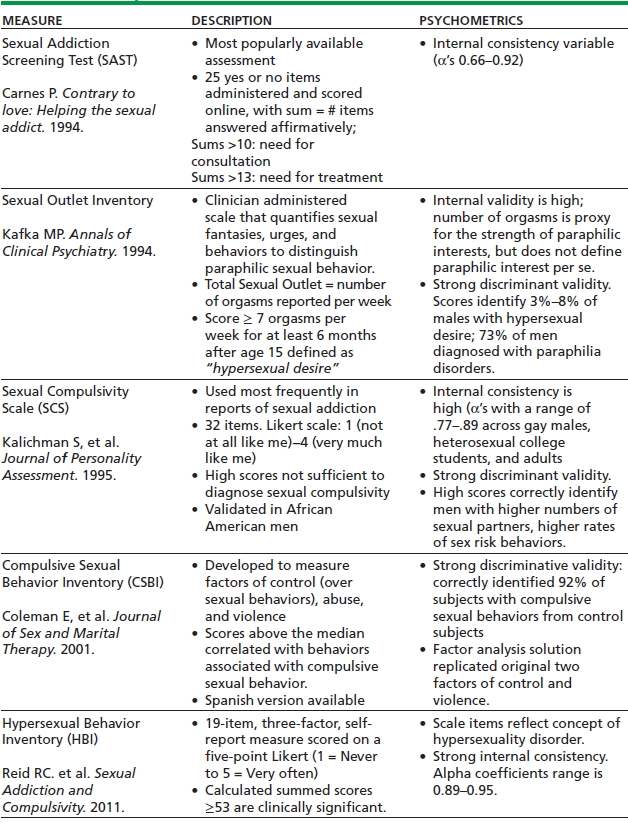
Over the past 20 years, several measures have been developed, and psychometric properties are established for their use in measuring various aspects of sexually compulsive behaviors. Hook et al. provide a comprehensive review 17 self-report and clinician-administered instruments assessing sexual addiction of most published instruments. Table 40-1 provides an overview of five of the most commonly used assessment measures of symptoms of sexual addictions used in the literature and provides their psychometric properties.
TABLE 40-1. FREQUENTLY USED MEASURES OF SEXUAL BEHAVIOR
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


