28 Sex hormones
male
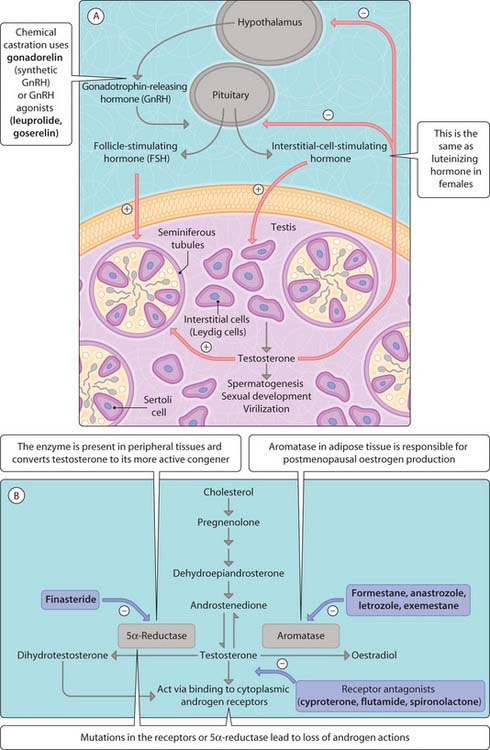
Androgens (e.g. testosterone) control spermatogenesis, sexual development, puberty and male virilization. The secretion of luteinizing hormone (referred to as interstitial cell-stimulating hormone (ICSH) in the male) and follicle-stimulating hormone (FSH) from the anterior pituitary by gonadotrophin-releasing hormone (GnRH) (Fig. 3.28.1) regulates spermatogenesis. ICSH stimulates the synthesis of testosterone by Leydig cells of the testis while FSH stimulates Sertoli cells to stimulate spermatogenesis. Testosterone acts locally to stimulate sperm production and peripherally on cells carrying testosterone receptors (steroid receptor family). The release of ICSH and FSH is regulated by testosterone, although this negative feedback mechanism becomes impaired during puberty. Testosterone is converted to its more active metabolite dihydrotestosterone by 5α-reductase, of which there are two isoforms with tissue-specific expression:
Testosterone has a variety of cellular effects within the developing male embryo (e.g. transformation of the wolffian ducts of epididymis, seminal vesicles and deferent ducts) and after puberty determines muscle mass, spermatogenesis, sexual potency, behaviour and coarsening of the voice. Dihydrotestosterone is responsible for the pubertal changes in the male and prostatic growth (Fig. 3.28.1B) and plays a role in controlling the growth of body hair (alopecia in men, hirsutism in women), enlargement of the prostate gland and acne. Both testosterone and dihydrotestosterone bind to intracellular androgen receptors, which translocate to the nucleus and alter the rate of gene transcription in Leydig cells, skeletal muscle, prostate gland, skin, sebaceous glands and brain. Mutations in the androgen receptor or in 5α-reductase result in loss of function, lack of virilization of the male embryo and pseudohermaphroditism.
< div class='tao-gold-member'>