Segmental Resection for Diverticulitis
Janice F. Rafferty
Introduction
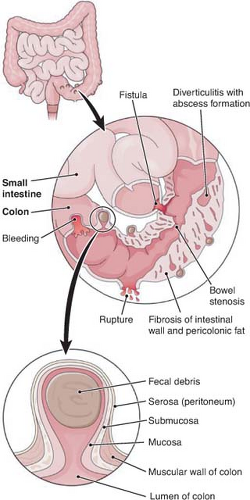
Acquired colonic diverticular disease affects the sigmoid colon in 95% of cases, and is a disease of the aging population. In fact 30% of U.S. adults will have diverticulosis evident on colonoscopy by the age of 60, while almost 60% of Americans who reach the age of 80 will have diverticulosis. Although diverticular change is most often found in a patient’s sigmoid colon, up to 35% will have diverticuli of the proximal colon as well. Diverticuli are rare both below the pelvic peritoneal reflection and beyond the splaying of the taenia coli onto the anterior wall of the rectum. This is due to the fact that the partial thickness herniations of mucosa and submucosa, or pseudodiverticuli, occur at the site where vasa recta traverse the colonic wall at or near the fibrous taenia coli (Fig. 1). True diverticuli are composed of all layers of the wall of the colon, and are thought to be congenital instead of acquired.
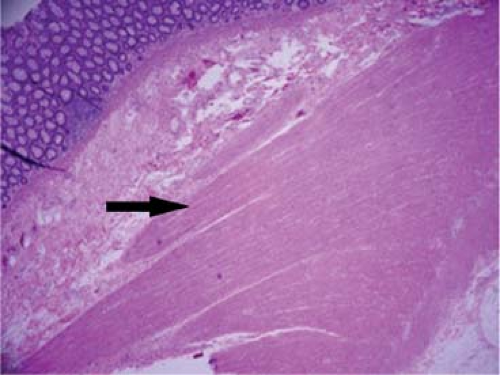
The etiology of diverticulosis is thought to be related to a chronic deficiency of dietary fiber, with resultant desiccated compact stool. High intracolonic pressures are required to propel dry stool forward, and areas of segmentation, combined with decreased tensile strength of collagen and muscle fibers related to aging, result in herniations through the bowel wall. These may be more prevalent in patients with connective tissue disorders such as Marfan’s and Ehlers-Danlos syndrome. A chronic increase in intraluminal pressure results in hypertrophy of the muscular wall of the colon; this is palpable at the time of operation and guides the extent of surgical resection (Fig. 2).
Only 10% to 25% of people with diverticulosis become patients with diverticulitis. Perforation of a diverticulum results in extravasation of fecal flora and infection of the paracolic tissues. Some microperforations are contained by the mesentery, or adhesion of the omentum and surrounding structures. Those not contained, which leak into the peritoneal cavity, often cause life-threatening peritonitis and require immediate attention of a surgeon. Whether a patient has acute life-threatening perforated diverticulitis, or chronic recurrent symptoms related to diverticular inflammation, segmental resection may be indicated. This chapter examines the clear indications as well as changing paradigms for surgical intervention in the treatment of diverticulitis.
While the management of lower gastrointestinal (GI) bleeding and algorithm for localization and resection will not be covered in depth, it is interesting to consider the pathogenesis of diverticular bleeding.
Colonic diverticuli protrude through the muscular layers of the wall of the colon in intimate contact with the nutritional artery. Over time, the artery undergoes pathologic changes characterized by eccentric muscular thickening and intimal thinning. Occasionally, this affected artery will bleed into the diverticulum and then into the colonic lumen; the arterial bleeding can be massive in volume and yet difficult to localize. Although the affected artery is associated with the diverticulum that protrudes to the serosal surface of the colon, the bleeding is virtually always into the colonic lumen. It is extremely rare that an artery associated with a diverticulum will bleed into the peritoneal cavity.
Colonic diverticuli protrude through the muscular layers of the wall of the colon in intimate contact with the nutritional artery. Over time, the artery undergoes pathologic changes characterized by eccentric muscular thickening and intimal thinning. Occasionally, this affected artery will bleed into the diverticulum and then into the colonic lumen; the arterial bleeding can be massive in volume and yet difficult to localize. Although the affected artery is associated with the diverticulum that protrudes to the serosal surface of the colon, the bleeding is virtually always into the colonic lumen. It is extremely rare that an artery associated with a diverticulum will bleed into the peritoneal cavity.
Pathogenesis
De Quervain recognized that the condition we commonly call diverticulitis would more properly be called “peridiverticulitis.” It is an infection of the paracolic tissues caused by a perforation of a diverticulum. The perforation results in extravasation of feces through the colonic wall, either micro- or macroscopically. Since most diverticula are located on the mesenteric side of the colon, the perforation is often contained within the mesentery. Unfortunately, not all diverticular perforations are immediately confined by the mesentery, adjacent structures, or omentum. A free perforation into the peritoneal cavity may cause life-threatening peritonitis; similarly, a contained abscess cavity may rupture into the free peritoneal cavity or into adjacent organs and cause peritonitis or create a fistula. The clinical scenario and appropriate treatment plan is obviously different for each stage of this disease. The overall treatment goal for any case of diverticulitis is to control the infection, assess the likelihood of persistent or recurrent disease, and formulate a treatment plan that will control the infection and minimize the chance of recurrence.
A thorough history and physical examination is the basis for the accurate diagnosis of diverticulitis. A patient with contained peridiverticular inflammation involving the sigmoid colon most often complains of left lower quadrant or suprapubic pain, accompanied by fever and malaise; symptoms are often worsened when the bladder empties, or the colon propels stool forward during defecation. The typical patient is sedentary, overweight, and
oftentimes a smoker. On physical examination, left lower quadrant guarding, tenderness, and occasionally a mass may be felt. In patients with a redundant, tortuous sigmoid colon symptoms may be most acute on the right side, and can potentially mimic appendicitis by presenting with right lower quadrant abdominal pain and tenderness. Leukocytosis is common, and significant infection can be associated with ileus or small-bowel obstruction secondary to involvement of adjacent loops of intestine by the inflammatory process. A patient with a free perforation into the abdominal cavity will have a much more dramatic presentation, with signs and symptoms of generalized peritonitis and hemodynamic changes.
oftentimes a smoker. On physical examination, left lower quadrant guarding, tenderness, and occasionally a mass may be felt. In patients with a redundant, tortuous sigmoid colon symptoms may be most acute on the right side, and can potentially mimic appendicitis by presenting with right lower quadrant abdominal pain and tenderness. Leukocytosis is common, and significant infection can be associated with ileus or small-bowel obstruction secondary to involvement of adjacent loops of intestine by the inflammatory process. A patient with a free perforation into the abdominal cavity will have a much more dramatic presentation, with signs and symptoms of generalized peritonitis and hemodynamic changes.
Table 1 Differential Diagnosis of Acute Left Lower Quadrant Pain | |
|---|---|
|
Table 2 CT Severity Staging of Diverticulitis | |||
|---|---|---|---|
|
The list of differential diagnoses is long, and includes irritable bowel syndrome, gastroenteritis, bowel obstruction, inflammatory bowel disease, ischemic colitis, colorectal cancer, urinary tract infection, kidney stone, and gynecologic disorders (Table 1). Obviously, the treatment of each of these problems differs significantly, so accuracy in diagnosis is of utmost importance. The preferred test to confirm the suspected diagnosis of diverticulitis is a computer-assisted tomography (CAT) scan with both oral and IV contrast. This test is both highly sensitive and specific, with a high positive predictive value. While axial imaging is always acquired, multiplanar reconstructions in the coronal or sagittal planes can improve specificity. CAT scan is particularly useful in detecting the presence and location of a complication associated with diverticulitis, like an abscess, and can alter the treatment algorithm in certain patients. It also allows severity staging, which has emerged as a tool for predicting success of nonsurgical therapy in both the acute and the chronic setting (Table 2). The severity of acute diverticulitis is statistically predictive of the need for surgical treatment of the first episode of acute diverticulitis; it is also useful to predict a future complicated episode after successful conservative treatment of the acute phase. Patients who present with severe diverticulitis, as graded by CAT scan, have a >50% chance of future complication if their diverticulitis is not treated surgically (either in the acute or staged setting). While young age (<40 years) was initially thought to be related to poor outcome, severity staging on computed tomography (CT) has been shown to be more accurately predictive. When CAT scanning is not available, gentle contrast enema is an option for diagnosis, but is inferior to CAT scan in both sensitivity and detection of severe infection, especially when an abscess is present. Hinchey et al. initially used a classification system to guide surgical therapy in the acute setting; this remains useful today (Table 3), even though the limits of conservative management are being stretched. Stages I and II, according to Hinchey, were initially categorized as diverticular complications that could be surgically managed without a stoma, in selected patients. Stages III and IV, on the other hand, have historically mandated emergent surgical intervention with resection and stoma construction. Today, it has become apparent that certain patients with purulent peritonitis (Hinchey stage III) can be managed without colostomy construction, and in highly select cases, without laparotomy and resection during the acute phase of disease.
Treatment of diverticulitis depends on the severity of the infection, as determined by careful physical examination, and imaging studies. When diverticulitis is present, the CAT scan typically shows a thickened colonic wall in the area of the perforation, with contiguous inflammatory changes of the paracolic soft tissues and stranding of the mesentery (Fig. 3). This would be graded as mild or moderate severity, according to Ambrosetti. Diverticulitis complicated by abscess or extraluminal air can readily be seen on appropriate imaging as well (Fig. 4), and would qualify for a grade of severe disease.
Table 3 Hinchey Classification | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
Outpatient management may be appropriate for a limited patient population with uncomplicated diverticulitis, especially in the absence of fever, excessive vomiting, or marked peritonitis. Nonoperative treatment typically includes dietary modification and oral or intravenous antibiotics. This is successful in 70% to 100% of patients, but they must be compliant patients with ample opportunity for follow-up. The patient should be able to take liquids and oral antibiotics, and should be reexamined every few days to assess for change in their clinical appearance. Any deterioration in physical examination, or decrease in ability to take a diet or antibiotics, mandates hospital admission and if possible repeat CT scan to investigate the possibility of a complication associated with diverticulitis.
Patients with severe infection, as indicated by significant tenderness, nausea, emesis, fever, and leukocytosis should be admitted to the hospital for intravenous hydration and antibiotics, as well as close and careful clinical examination. A CAT scan should be obtained on admission, if available, to grade severity and look for complications associated with diverticulitis. Up to 15% of patients will have a pelvic or mesenteric abscess at presentation. Extraluminal air in the absence of generalized peritonitis is not in itself an indication for emergent surgery; if peritoneal irritation is focal, nonoperative management may be feasible in an otherwise healthy, hemodynamically stable patient. Most patients experiencing an attack of diverticulitis will respond favorably to nonoperative treatment. Treatment varies depending upon the severity of the disease and specific circumstances, ranging from oral antibiotics to bowel rest, nasogastric decompression, intravenous antibiotics, and percutaneous drainage of contained intra-abdominal or pelvic abscesses. Diverticulitis that responds readily to antibiotics is considered to be uncomplicated. A single uncomplicated attack of diverticulitis that responds to antibiotic treatment is likely to recur in about 20% of patients, with patients under the age of 50 years being more likely to suffer recurrences than older patients (27% vs. 17%). However, the risk of a subsequent attack requiring emergency surgery and a colostomy is <6%.
 Fig. 3. Moderately severe diverticulitis as seen on CT scan.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|