Sarcoidosis
Key Facts
Etiology/Pathogenesis
Etiology unknown, but evidence suggests it may represent exaggerated cellular immune response to an unidentified antigen
Clinical Issues
Most commonly affected sites include lungs (95% of patients) and lymphatic organs
May be asymptomatic and discovered incidentally on chest x-rays
Symptomatic patients may present with insidious chronic disease or an acute presentation
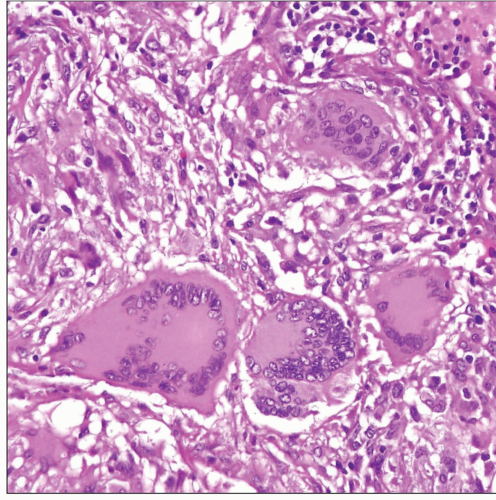
Microscopic Pathology
Multiple small, nonnecrotizing interstitial epithelioid granulomas distributed along bronchovascular bundles and interlobular septa
Nodular sarcoidosis shows confluence of granulomas with large tumor nodule formation
Granulomas are frequently distributed along bronchial submucosa, accounting for high yield in bronchoscopic biopsies
Interstitial inflammation is absent or inconspicuous
Vasculitis and foci of necrosis may sometimes accompany the granulomas
Granulomas are composed of aggregates of epithelioid histiocytes ± multinucleated giant cells
Diagnostic Checklist
Sarcoidosis is a diagnosis of exclusion made by clinician rather than pathologist
Special stains for organisms (AFB, PAS, GMS) should always be done to rule out infection
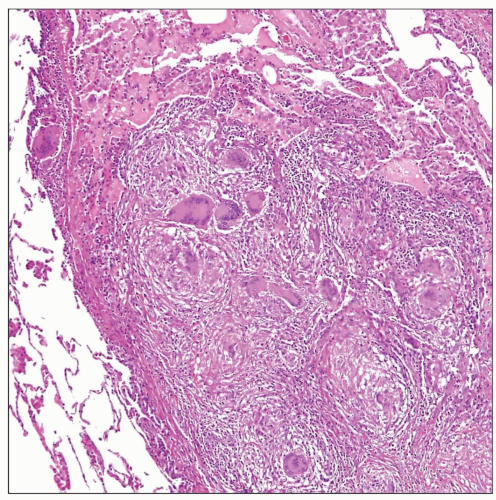 Pulmonary sarcoidosis shows well-circumscribed collections of histiocytes without evidence of necrosis and abundant multinucleated giant cells. |
TERMINOLOGY
Definitions
Multiorgan disease characterized by nonnecrotizing epithelioid granulomas
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Etiology is unknown, but evidence suggests it may represent exaggerated cellular immune response to an unidentified antigen
Genetic Predisposition
Marked familial clustering of cases
CLINICAL ISSUES
Epidemiology
Incidence
About 10 per 100,000 people per year
Age
Young adults (from 20-40 years of age)
Gender
Slight female predominance
Ethnicity
Increased incidence in African Americans
Site
Most commonly affected sites include lungs (95% of patients) and lymphatic organs
Other organs involved include liver, spleen, skin, heart, and eyes; central nervous system (CNS) may also be involved
Presentation
Fatigue
Anorexia
Weight loss
Fever
Triad of erythema nodosum, bilateral hilar lymphadenopathy, and polyarthralgia (Löfgren syndrome) seen in 20-50% of patients
Laboratory Tests
Hyperglobulinemia due to nonspecific polyclonal activation of B cells by helper T cells
Elevation of serum levels of angiotensin-converting enzyme
Natural History
May be asymptomatic and discovered incidentally on chest x-rays
Symptomatic patients may present with insidious chronic disease or an acute presentation
Spontaneous resolution is commonly the rule
Progressive and disabling organ failure may occur in up to 10% of patients
Treatment
Drugs
Corticosteroids (prednisone)
Immunosuppressive or cytotoxic drugs
Prognosis
Most cases involute spontaneously
Mortality may occur in a small percentage of patients (1-5%) due to progressive lung, heart, or CNS involvement