Safe Medication Administration
Introduction
Safe medication administration involves more than accurate dose measurement and calculations. Prior to calculation, the nurse must be able to interpret the medication-related documents that will be encountered. This interpretation includes knowledge of medical terminology, hospital forms and abbreviations used in medication orders, drug forms, drug label contents, medication-related patient records, and current drug references. Attention to detail and patient rights are necessary elements for the protection of each patient.
Patient Rights
There are many patient rights related to safe medication administration. As you read through these seven rights, think about the implications should one of these rights be violated.
Right Patient
The patient for whom the medication is ordered must be the patient who receives the medication. Similar names and lack of attention to patient identification when the medication is in hand can result in a medication being administered to the wrong patient. There are strict agency and The Joint Commission procedures for safe patient identification. They include using two separate written identifiers, such as the patient name and medical record number or birth date.
Right Drug
The nurse must be able to interpret orders for the drug, identify and clarify incomplete or unclear orders by conferring with the prescriber, and compare supplied drugs by matching them exactly to the order. Drugs may have a trade name in addition to a generic and chemical name. The nurse needs to become familiar with these alternative names. There are many similar-sounding drugs on the market, and they must be distinguished from each other.
Right Dose
Knowledge of abbreviations and measurement systems commonly used in the preparation and administration of medications is essential. The nurse must ascertain that it is a safe dose for the intended patient and must calculate and measure the precise dose ordered. Attention to decimals and zeros is vital for the prevention of errors.
Right Time
If a medication is omitted, delayed, or given too early, there can be serious consequences. A nurse must be able to interpret the 24-hour clock as well as read traditional time. Prioritizing emergency and stat drugs and identifying drugs that have to be given before, with, or after a meal are abilities that must be acquired through clinical practice and supervision. Knowledge of each drug’s purpose and action is required. It is important to ask for help if the workload is too heavy to allow for perfect attention to detail.
 CLINICAL ALERT
CLINICAL ALERT
Always document the medication promptly after it is administered. Never document before a medication is administered. Doing so may lead to double dosing a medication.
Right Route
The nurse must prepare the medication so it can be administered via the route ordered. Abbreviations are usually used for medication routes. Many medications are available in solid and liquid forms for oral, intramuscular, or intravenous routes of administration. If the patient refuses or is unable to tolerate the route ordered, the nurse must obtain an order for change from the prescriber.
Right Documentation
Accurate and timely reporting and documentation in the patient medical records is an essential protection for the patient and the nurse.
Right to Refuse a Medication
Patients are entitled to refuse medications (and treatments). The reason should be ascertained, reported, and documented in a timely fashion so that corrective action can be taken if necessary. Include a comment on mental status when reporting and recording refusals.
Medication Errors
Several studies have shown that many medications are given in error; the rate ranges from 2% to well over 10% when underreporting and wrong time of administration are considered.
Errors may occur in the prescriber’s order, in the interpretation of the order by the pharmacy or the nurse, in the copying of the order into a computer or onto a record, on the label or with the medication supplied by the pharmacy, or during the preparation and administration of the medication. Check agency policies pertaining to reporting medication errors.
There are many Internet references well worth reading that pertain to medication errors. The following is a sampling of on-line sources:
www.nlm.nih.gov/medlineplus/drugsafety.html
www.nlm.nih.gov/medlineplus/drugsafety.html
www.fda.gov/cder/drug/MedErrors
www.jointcommission.org/PatientSafety/DoNotUseList
www.nccmerp.org/aboutMedErrors.html
Note: It is recommended that you subscribe to the ISMP free medication safety newsletter: www.ismp.org/newsletters/nursing/default.asp
 CLINICAL ALERT
CLINICAL ALERT
The nurse who prepares and administers the medication offers the last protection to the patient.
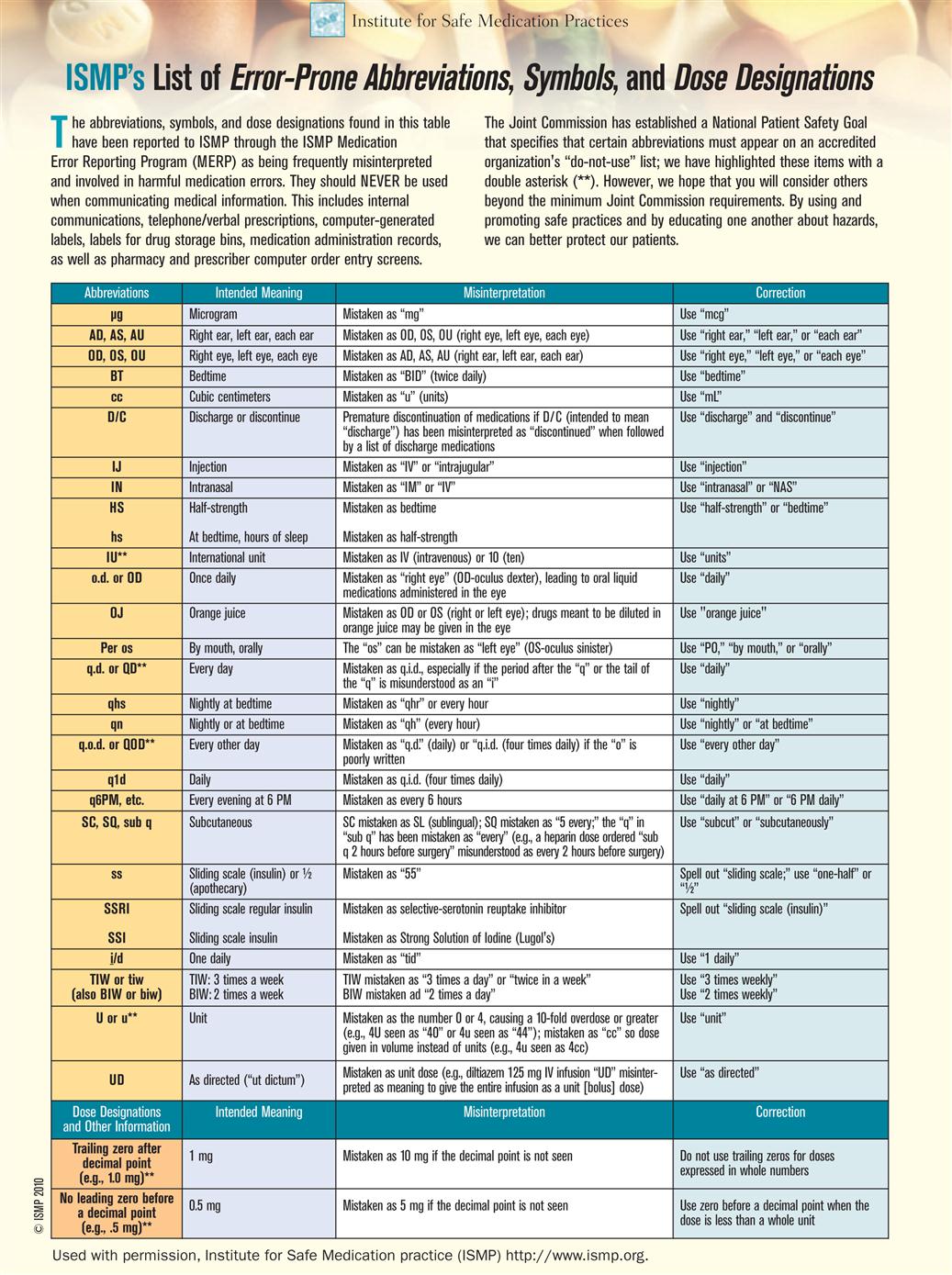
Abbreviations
In order to interpret prescriber orders, drug literature, and drug labels, the nurse must learn treatment-related and medication-related abbreviations; they are listed on the inside front cover. The nurse must also avoid writing the abbreviations that are on The Joint Commission’s Do Not Use list (Table 3-1). These abbreviations have been misinterpreted and have led to medication errors. Only approved abbreviations may be used, and they must be written precisely. You will have to review them several times in order to memorize them. Use these worksheets to help yourself remember them. Abbreviations for drugs have led to errors and are best avoided. The trend is to reduce the number of approved abbreviations.
Table 3-1
The Joint Commission’s Official “Do Not Use” List
| Official “Do Not Use” List1 | ||
| Do Not Use | Potential Problem | Use Instead |
| U (unit) | Mistaken for “0” (zero), the number “4” (four) or “cc” | Write “unit” |
| IU (International Unit) | Mistaken for IV (intravenous) or the number 10 (ten) | Write “International Unit” |
| Trailing zero (X.O mg)* Lack of leading zero (.X mg) | Decimal point is missed | Write × mg Write O.X mg |
| Additional Abbreviations, Acronyms and Symbols (For possible future inclusion in the Official “Do Not Use” List) | ||
| Do Not Use | Potential Problem | Use Instead |
| > (greater than) < (less than) | Misinterpreted as the number “7” (seven) or the letter “L” Confused for one another | Write “greater than” Write “less than” |
| Abbreviations for drug names | Misinterpreted due to similar abbreviations for multiple drugs | Write drug names in full |
| Apothecary units | Use metric units | |
| @ | Mistaken for the number “2” (two) | Write “at” |
| cc | Mistaken for U (units) when poorly written | |
| μg | Write “meg” or “micrograms” | |
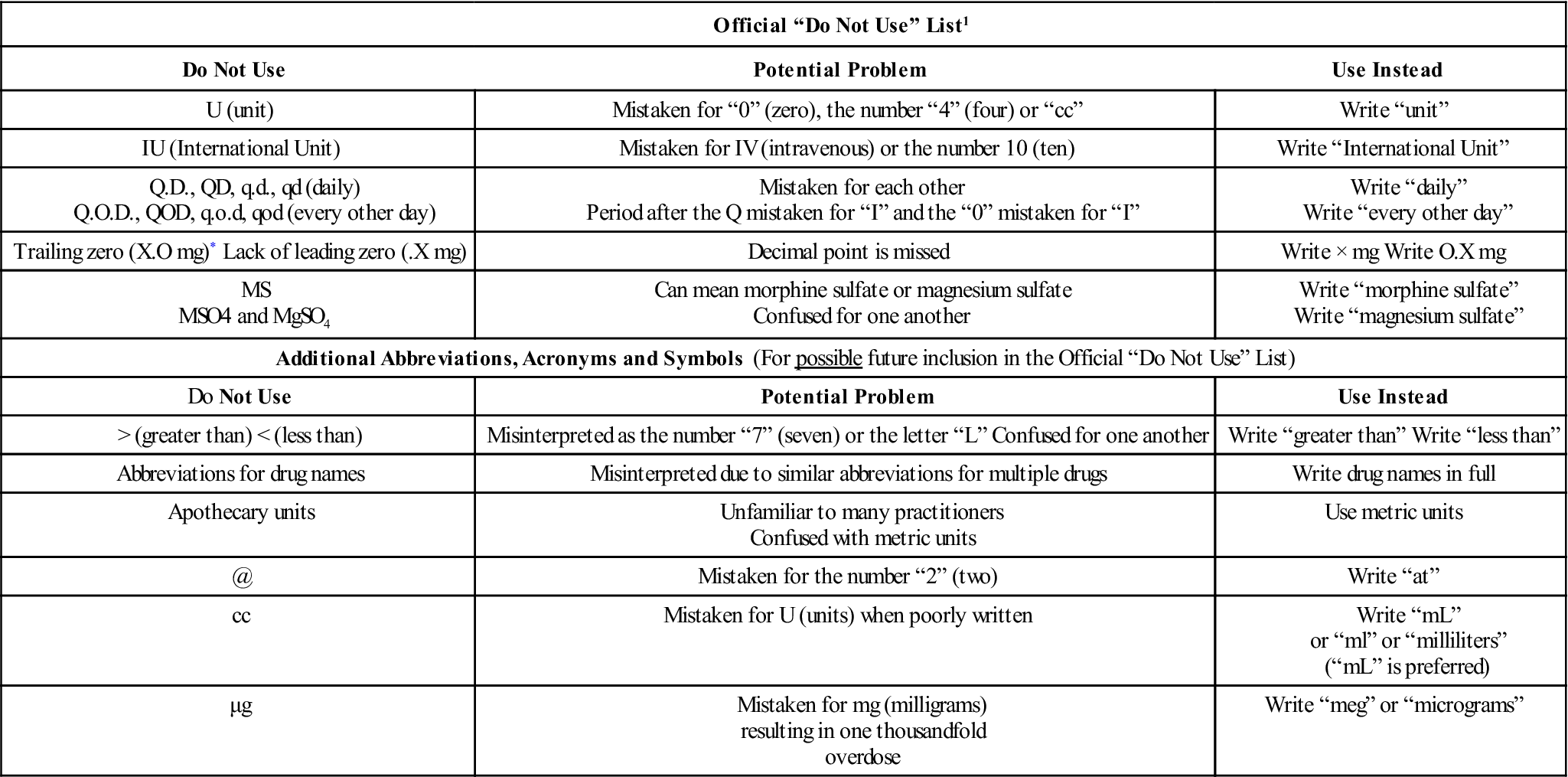
*Exception: A “trailing zero” may be used only where required to demonstrate the level of precision of the value being reported, such as for laboratory results, imaging studies that report size of lesions, or catheter/tube sizes. It may not be used in medication orders or other medication-related documentation.
© The Joint Commission, 2010 Reprinted with permission.
Study the approved and recommended abbreviations and their patterns of similarities and differences as well as The Joint Commission’s Do Not Use list in Table 3-1 and the Institute for Safe Medication Practices (Table 3-2). Then enter the approved or recommended abbreviation in the space provided.
Worksheet 3A
Abbreviations for Time and Route Table
| Time | Abbreviation (if Applicable) | Time | Abbreviation (if Applicable) |
| before | after | ||
| before meals | after meals | ||
| daily | Write out daily | three times a day | |
| twice a day | every other day | Write out every other day | |
| every day | Write out every day | every 6 hours | |
| every 4 hours | every 12 hours | ||
| whenever necessary | as desired, freely | ||
| immediately, at once | bedtime | Write out bedtime | |
| with | without | ||
| by mouth | nothing by mouth | ||
| intravenous | intramuscular | ||
| sublingual | subcutaneous | ||
| intradermal | suppository* | ||
| left eye | Write out left eye | right ear | Write out right ear |
| nasogastric | per gastrostomy tube |
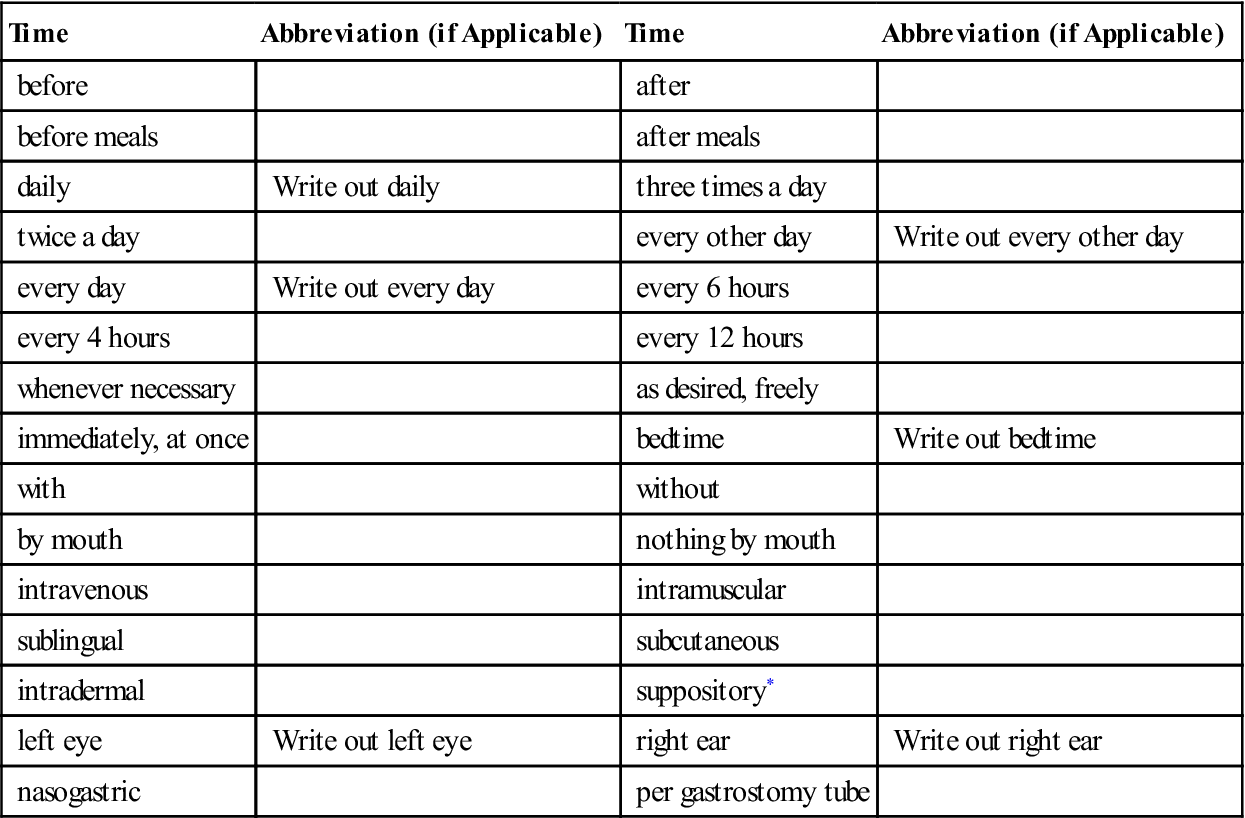
*Orders for suppositories require further route identification per vagina, per rectum, or per urethra.
Measurement Abbreviations
Metric abbreviations are commonly used for medication orders.
Metric measurement abbreviations are not pluralized. Two kilograms would be written as 2 kg, not 2 kgs; 2 grams would be written as 2 g, not 2 gs. Insert a space between the number and the metric unit: 10 g (not 10 g).
Study the abbreviations on the inside front cover. Pay attention to upper and lower case letters when learning the abbreviations. There are only a few instances when upper case is employed. Then provide the approved abbreviations for the measurements.
| Metric Measurement Term* | Abbreviation (if Applicable) |
| microgram(s) | |
| milligram(s) | |
| gram(s) | |
| kilogram(s) | |
| milliliter(s) | |
| milliequivalent(s) | |
| unit | Write out unit |
| international unit | Write out international unit |
| liter | |
| square meter | |
| Other Measurement Term | Abbreviation (if Applicable) |
| one half | Write out one half |
| teaspoon | |
| tablespoon | |
| pound |
*The metric abbreviations are the same for singular and plural measurements.
 CLINICAL ALERT
CLINICAL ALERT
mcg, micrograms, may also be encountered written as mg. Write mcg for micrograms because mg has been misread as mg (milligrams) when poorly written; that is a thousandfold error.
cc is sometimes written interchangeably with mL (milliliters). It means cubic centimeters and has been mistaken for aa (of each) and u (units). Write mL instead. Do not write cc. Do not make up your own abbreviations for metric terms.
Study the abbreviations on the inside front cover. Then provide the abbreviations in the spaces provided.
| Term | Recommended Abbreviation |
| capsule* | |
| tablet | |
| fluid | |
| solution | |
| suspension | |
| elixir | |
| teaspoon | |
| tablespoon | |
| liquid | |
| ounce | |
| double-strength | |
| extended release* | |
| long acting* | |
| sustained release* | |
| controlled release* |
 CLINICAL ALERT
CLINICAL ALERT
Study examples of abbreviations that have caused errors and are best written out. Refer to Tables 3-1 and 3-2.
Medication Delivery
Many hospital pharmacies stock supply and resupply computerized medication carts as shown in Figure 3-1. Computerized carts with bar scanners are thought to provide greater security and reduce the chances of medication errors by providing unit dose (single-serving) medications for one to three shifts at a time and one bottle of multidose liquid medications (Figure 3-2). The bar scanner is used to compare the bar code on the medication with the patient ID at the bedside (Figure 3-3).
Drug Forms: Solids and Liquids
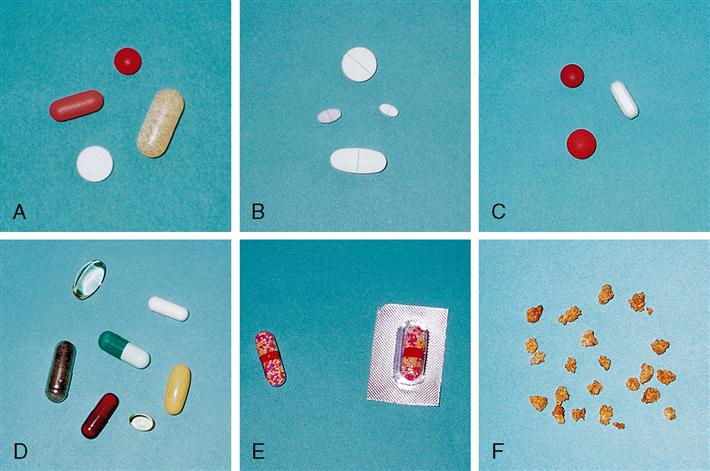
As can be seen in the list and figures that follow, drugs can be provided in a variety of forms for both oral and other routes—tablets, capsules, suspensions, suppositories, and so forth. It is very important to distinguish among the forms and to ascertain the precise form intended by the prescriber. The form affects the rate of absorption of the drug and the route of administration.
Solids
• Plain tablets (Figure 3-4, A): compressed powdered drugs.
• Scored tablets (Figure 3-4, B): tablets with indentation; the only kind of tablet that may be broken. Use a pill cutting device for an accurate cut. (Figure 4-2)
• Enteric-coated tablets (Figure 3-4, C): tablets with coating for delayed dissolution.
• Capsules (caps) (Figure 3-4, D): soluble case, usually gelatin, that holds liquid or dry particles of drug.
• Extended-release capsules (S-R, slow-release) (Figure 3-4, E): capsules that contain beaded particles of drug for delayed absorption.
• Powders/granules (Figure 3-4, F): loose or molded drug substance; usually to be dissolved in liquid or food.
Liquids
• Elixirs: sweetened alcohol and water solutions
• Emulsions: fats or oils suspended in liquid by an emulsifier
• Extracts: syrups or derived forms of active drugs
• Fluid extracts: concentrated alcoholic liquid extracts of plants or vegetables
 CLINICAL ALERT
CLINICAL ALERT
Some tablets may be crushed if needed, and mixed with a liquid. Check current drug reference (Fig 3-5).
Reminder: Never cut unscored tablets. Never crush enteric-coated, E-R, S-R, XR, or gel-coated medications. Do not crush capsules. Check with prescriber if it is deemed necessary to alter the ordered form of medication, for example, when the patient develops difficulty swallowing.
Oral liquids are supplied in individual prepacked unit dose cups, bottles, calibrated plastic spoons, oral syringes, and so forth. Medicine cups with metric measurements are commonly used.
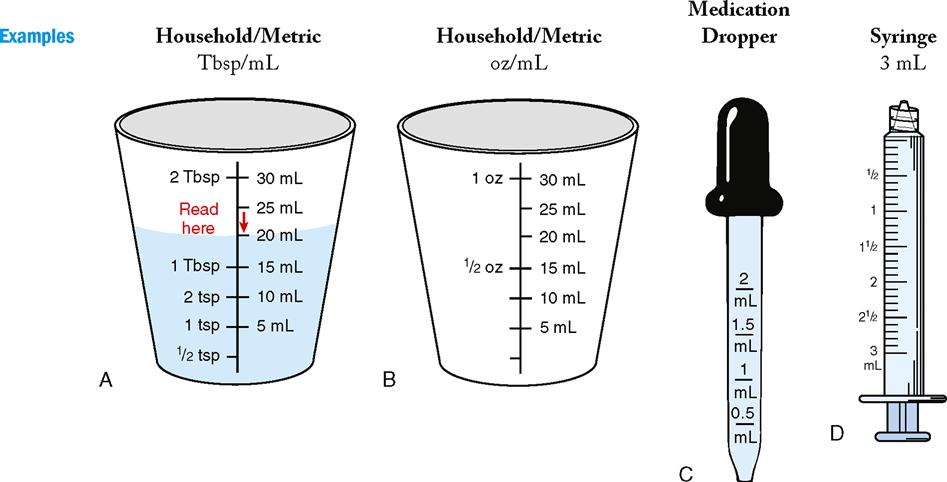
Medicine dropper. (From Clayton BD, Stock YN, Cooper S: Basic pharmacology for nurses, ed 15, St Louis, 2010, Mosby. Courtesy of Chuck Dresner.)
3 mL syringe. (From Perry AG, Potter PA: Clinical nursing skills and techniques, ed 7, St Louis, 2010, Mosby.)
 CLINICAL ALERT
CLINICAL ALERT
Do not substitute the ordered form of a drug for another form. Do not substitute household utensils, such as spoons, cups, and droppers, when measuring medications. Medication utensils are calibrated for exact doses according to the metric system of measurement.
Liquid Injectables
Liquids may also be supplied in injectable (also known as parenteral ) forms in ampules, vials, and prefilled syringes these are covered in Chapter 5.
Medication Labels
It is helpful to study the information provided on medication labels so as to facilitate your interpretation of prescriber orders and of medication administration records. Some of the label information is already familiar because of personal experience with medication prescriptions and over-the-counter (OTC) products. The label must be read carefully to ensure that the medication is precisely what the prescriber ordered.
Interpreting Medication Labels
Medication labels can be confusing because of the vast amount of information they contain and the small print. Some labels are prepared in-house by pharmacists or pharmacy technicians. The most important information is as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree