S
Salivation, decreased
[Xerostomia]
Typically a common but minor complaint, diminished production or excretion of saliva (dry mouth) usually results from mouth breathing. However, this symptom can also result from salivary duct obstruction, Sjögren’s syndrome, the use of an anticholinergic other drug, and the effects of radiation. It can even result from vigorous exercise or autonomic stimulation—for example, as the result of fear.
HISTORY AND PHYSICAL EXAMINATION
Evaluate the patient’s complaint of dry mouth by asking pertinent history questions: When did he first notice the symptom? Was he exercising at the time? Is he currently taking any medications? Is his sensation of dry mouth intermittent or continuous? Is it related to or relieved by a particular activity? Ask about related symptoms, such as burning or itching eyes, or changes sense of smell in or taste.
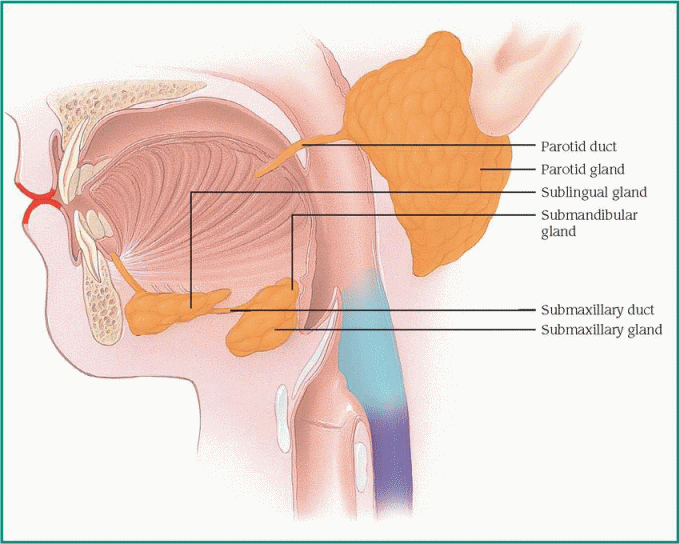
Next, inspect the patient’s mouth, including the mucous membranes, for any abnormalities. Observe his eyes for conjunctival irritation, matted lids, and corneal epithelial thickening. Perform simple tests of smell and taste to detect impairment of these senses. Check for enlarged parotid and submaxillary glands. (See Examining salivary glands and ductal openings, page 610.) Palpate for tender or enlarged areas along the neck, too.
MEDICAL CAUSES
♦ Dehydration. Decreased saliva production causes dry oral mucous membranes. Skin turgor is also decreased, and urine output may be low.
♦ Facial nerve paralysis. A diminished saliva production occurs along with decreased sense of taste and facial muscle movement.
♦ Salivary duct obstruction. Usually associated with a salivary stone, this obstruction causes reduced salivation and local pain and swelling.
♦ Sjögren’s syndrome. Diminished secretions from the lacrimal, parotid, and submaxillary glands produce the hallmarks of this disorder: decreased or absent salivation and dry eyes with a persistent burning, gritty sensation. The patient may also experience dryness that involves the nose, respiratory tract, vagina, and skin.
Related oral signs and symptoms include difficulty chewing, talking, and swallowing as well as ulcers and soreness of the lips and mucosa. The parotid and submaxillary glands may be enlarged. Nasal crusting, epistaxis, fatigue, lethargy, nonproductive cough, abdominal discomfort, and polyuria may be present. These signs and symptoms may occur alone or with rheumatoid arthritis or another connective tissue disorder.
OTHER CAUSES
♦ Drugs. Anticholinergics, antihistamines, tricyclic antidepressants, phenothiazines, clonidine, and opioid analgesics can cause decreased salivation, which disappears after discontinuation of therapy.
When a patient reports decreased salivation, assess the parotid and submaxillary glands for enlargement and the ductal openings for salivary flow.
To detect an enlarged parotid gland, ask the patient to clench his teeth, thereby tensing the masseter muscle. Then palpate the parotid duct (about 2″ [5 cm] long); you should be able to feel it against the tensed muscle, on the cheek just below the zygomatic arch. Next, check the ductal orifice, opposite the second molar. Using a gloved finger, palpate the orifice for enlargement, and observe for drainage.
Palpate the submaxillary gland. About the size of a walnut, this gland is located under the mandible, anterior to the angle of the jaw. Using a gloved finger, palpate the floor of the mouth for enlargement of the submaxillary ductal orifice.
Finally, test both ductal openings for salivary flow. Place cotton under the patient’s tongue, have him sip pure lemon juice, and then remove the cotton and observe salivary flow from each opening. Document your findings.
 |
♦ Radiation. Excessive irradiation of the mouth or face from chemotherapeutic treatments or dental X-rays may cause transient decreased salivation due to salivary gland atrophy, which can lead to difficulty swallowing, discomfort, and gum disease.
SPECIAL CONSIDERATIONS
If markedly reduced salivation interferes with speaking, eating, or swallowing, allow the patient extra time for these activities.
PEDIATRIC POINTERS
Mouth breathing and anticholinergic therapy are the primary causes of decreased salivation in children.
PATIENT COUNSELING
To relieve dry mouth, encourage the patient to increase his fluid intake during meals and to chew gum or tart sugarless mints between meals. To reduce the risk of cavities, advise him to brush his teeth, floss, use mouthwash, and avoid sugary desserts, candies, and drinks. Routine dental visits and fluoride treatments may also be beneficial.
Pilocarpine hydrochloride (5 to 10 mg orally three times daily) can relieve symptoms of dry mouth, but it must be used regularly.
Salivation, increased
[Polysialia, ptyalism]
Increased salivation is an uncommon symptom that can result from a GI disorder, especially of the mouth. It also accompanies certain systemic disorders and may result from the use of certain drugs or from exposure to toxins. Saliva may also accumulate because of difficulty swallowing. (See “Dysphagia,” page 235.)
HISTORY AND PHYSICAL EXAMINATION
A patient who complains of increased salivation may have overproductive salivary glands or difficulty swallowing. To distinguish these, first test for a gag reflex and observe the patient’s ability to swallow and chew. Is he drooling? Is his chewing uncoordinated? An impaired gag reflex, drooling, and chewing incoordination suggest difficulty swallowing. Does he have related signs and symptoms, such as fatigue, fever, headache, or a sore throat? Ask about exposure to industrial toxins, such as mercury. Is the patient taking any medications? Note especially use of iodides, cholinergics, and miotics.
Inspect the mouth and mucous membranes for lesions. If present, are they painful? Put on gloves and palpate the lesions, which may be suppurative or infectious. Describe them in your notes. Next, inspect the uvula, gingivae, and pharynx. Palpate the lymph nodes, and determine if the parotid glands are swollen or sore.
MEDICAL CAUSES
♦ Bell’s palsy. Paralysis of the facial nerve causes an inability to control salivation or close the eye on the affected side.
♦ Pregnancy. In the early months of pregnancy, many women experience increased salivation, nausea, and breast tenderness.
♦ Stomatitis. Mucosal ulcers may be accompanied by moderately increased salivation, mouth pain, fever, and erythema. Spontaneous healing usually occurs in 7 to 10 days, but scarring and recurrence are possible.
♦ Syphilis. With secondary syphilis, mucosal ulcers cause increased salivation that may persist up to a year. Related findings include fever, malaise, headache, anorexia, weight loss, nausea, vomiting, sore throat, and generalized lymphadenopathy. A bilaterally symmetrical rash appears on the arms, trunk, palms, soles, face, and scalp. Condylomata develop in the genital and perianal areas.
♦ Tuberculosis. Certain forms of tuberculosis may produce solitary, irregularly shaped mouth or tongue ulcers, covered with exudate, that cause increased salivation. Other findings include weight loss, anorexia, fever, fatigue, malaise, dyspnea, cough, night sweats (a common sign), and hemoptysis.
OTHER CAUSES
♦ Arsenic poisoning. Common effects of arsenic poisoning are diarrhea, diffuse skin hyperpigmentation, and edema of the eyelids, face, and ankles; increased salivation occurs infrequently. The patient may also exhibit garlicky breath odor, pruritus, alopecia, irritated mucous membranes, headache, drowsiness, and confusion. He may also develop muscle aching, weakness, seizures, and paresthesia in a stocking-glove distribution pattern.
♦ Drugs. Increased salivation may occur with iodide toxicity, but the earliest symptoms are a brassy taste and a burning sensation in the mouth and throat. Associated findings include sneezing, irritated eyelids, and (commonly) pain in the frontal sinus.
Pilocarpine and other miotics used to treat glaucoma may be absorbed systemically, increasing salivation. Cholinergics, such as bethanechol, may also cause this symptom.
♦ Mercury poisoning. Stomatitis, characterized by increased salivation and a metallic taste, commonly occurs in those with mercury poisoning. The patient’s teeth may be loose and his gums are painful, swollen, and prone to bleeding. A blue line appears on the gingivae. The patient may also experience personality changes, memory loss, abdominal cramps, diarrhea, paresthesia, and tremors of the eyelids, lips, tongue, and fingers.
SPECIAL CONSIDERATIONS
Though annoying to the patient, increased salivation doesn’t require treatments beyond those needed to correct the underlying disorder.
PEDIATRIC POINTERS
Besides stemming from conditions that affect adults, increased salivation in children may also stem from congenital esophageal atresia. With this disorder, the infant is unable to swallow seemingly excessive saliva and frothy mucus.
GERIATRIC POINTERS
Drooling is common in elderly people with Parkinson’s disease. It’s caused by a reduction in automatic or conscious swallowing rather than by excessive salivation.
Salt craving
Craving salty foods is a compensatory response to the body’s failure to adequately conserve sodium. Normally, the renal tubules reabsorb almost all sodium, allowing less than 1% of it to be excreted in the urine. This reabsorption is regulated by aldosterone, a hormone synthesized in the adrenal gland. However, adrenal dysfunction can reduce aldosterone levels, thereby impairing reabsorption and increasing excretion of sodium.
 Sudden or rapidly worsening salt craving may indicate adrenal crisis. Adrenal crisis produces profound weakness, fatigue, nausea, vomiting, hypotension, dehydration and, occasionally, high fever. If untreated, this condition can ultimately lead to vascular collapse, renal shutdown, coma, and death. It requires prompt I.V. bolus administration of hydrocortisone. Later, doses may be given I.M. or may be diluted with dextrose in saline solution and given I.V. until the patient’s condition stabilizes.
Sudden or rapidly worsening salt craving may indicate adrenal crisis. Adrenal crisis produces profound weakness, fatigue, nausea, vomiting, hypotension, dehydration and, occasionally, high fever. If untreated, this condition can ultimately lead to vascular collapse, renal shutdown, coma, and death. It requires prompt I.V. bolus administration of hydrocortisone. Later, doses may be given I.M. or may be diluted with dextrose in saline solution and given I.V. until the patient’s condition stabilizes.HISTORY AND PHYSICAL EXAMINATION
Because normal salt intake varies widely, depending on dietary preferences and cultural differences, find out how much salt the patient typically uses. Has he increased this amount recently? Has he also experienced weakness, fatigue, anorexia, or weight loss? Has he fainted or felt dizzy? Check for a history of adrenal insufficiency or diabetes mellitus and for recent onset of polydipsia or polyuria. Inspect the patient’s skin for hyperpigmentation or hypopigmentation. Take his vital signs, too, noting orthostatic hypotension.
MEDICAL CAUSES
♦ Adrenal insufficiency (primary). Commonly called Addison’s disease, this disorder reduces aldosterone secretion. As a result, the patient may exhibit an intense craving for salty food. He may display diffuse brown, tan, or bronze-toblack hyperpigmentation of exposed areas (such as the face, knees, and knuckles) and of nonexposed areas (such as the tongue, buccal mucosa, or palmar creases) as well as darkening of normally pigmented areas, moles, and scars. Related findings include weakness, anorexia, nausea, irritability, vomiting, decreased cold tolerance, dizziness, low blood pressure, weight loss, abdominal pain, and slowly progressive fatigue.
SPECIAL CONSIDERATIONS
Prepare the patient for laboratory tests, such as plasma renin activity and serum aldosterone, serum electrolyte, plasma cortisol and glucose, urine 17-ketogenic steroids and 17-hydroxycorticosteroid, and corticotropin levels. Special provocative studies may include the metyrapone test and the rapid corticotropin test. Collect a urine specimen, and use a reagent strip to test for glucose and acetone.
To check for volume depletion, monitor and record the patient’s blood pressure, weight, intake and output, and skin turgor. Encourage the patient to drink plenty of fluids, and arrange for a diet that helps maintain adequate sodium and potassium levels. Be alert for signs of hyponatremia, such as hypotension, muscle twitching and weakness, and abdominal cramps. Look for signs and symptoms of hyperkalemia, such as muscle weakness, tachycardia, nausea, vomiting, and characteristic ECG changes, including tented and elevated T waves, widened QRS complex, prolonged PR interval, flattened or absent P waves, and depressed ST segment.
If diagnostic tests confirm primary adrenal insufficiency, emphasize the importance of complying with lifelong steroid (glucocorticoid or mineralocorticoid) therapy.
PEDIATRIC POINTERS
Salt craving in children may stem from decompensated congenital adrenal hyperplasia; although this disorder usually responds adequately to steroid replacement. Adrenal insufficiency can also develop with surgery or acute illness. Salt craving may signal a change in condition requiring increased steroid dosage.
PATIENT COUNSELING
If the patient will be taking a steroid (usually hydrocortisone), explain why he needs to take the
drug. Explain to him the adverse effects of the drug and the signs and symptoms of steroid toxicity and underdosage. Instruct the patient not to decrease the dose or discontinue the drug without a physician’s order. Explain that his dosage may need to be increased during times of stress (infection, injury, even profuse sweating) to prevent adrenal crisis. Tell him that he’ll need lifelong medical supervision to monitor the steroid therapy.
drug. Explain to him the adverse effects of the drug and the signs and symptoms of steroid toxicity and underdosage. Instruct the patient not to decrease the dose or discontinue the drug without a physician’s order. Explain that his dosage may need to be increased during times of stress (infection, injury, even profuse sweating) to prevent adrenal crisis. Tell him that he’ll need lifelong medical supervision to monitor the steroid therapy.
Instruct the patient to wear a medical identification bracelet at all times, indicating his condition and the name and dosage of the drug he takes. Teach him how to self-administer the drug parenterally in emergency situations such as traveling in remote areas away from medical help. Urge him to keep a prepared syringe of the drug available for emergency use.
Scotoma
A scotoma is an area of partial or complete blindness within an otherwise normal or slightly impaired visual field. Usually located within the central 30-degree area, the defect ranges from absolute blindness to a barely detectable loss of visual acuity. Typically, the patient can pinpoint the scotoma’s location in the visual field. (See Locating scotomas, page 614.)
A scotoma can result from a retinal, choroid, or optic nerve disorder. It can be classified as absolute, relative, or scintillating. An absolute scotoma refers to the total inability to see all sizes of test objects used in mapping the visual field. A relative scotoma, in contrast, refers to the ability to see only large test objects. A scintillating scotoma refers to the flashes or bursts of light commonly seen during a migraine headache.
HISTORY AND PHYSICAL EXAMINATION
First, identify and characterize the scotoma, using such visual field tests as the tangent screen examination, the Goldmann perimeter test, and the automated perimetry test. Two other visual field tests—confrontation testing and the Amsler grid—may also help in identifying a scotoma.
Next, test the patient’s visual acuity and inspect his pupils for size, equality, and reaction to light. An ophthalmoscopic examination and measurement of intraocular pressure (IOP) are necessary.
Explore the patient’s medical history, noting especially any eye disorders, vision problems, or chronic systemic disorders. Find out if he takes medications or uses eyedrops.
MEDICAL CAUSES
♦ Chorioretinitis. Inflammation of the choroid and retina produces a paracentral scotoma. Ophthalmoscopic examination reveals clouding and cells in the vitreous, subretinal hemorrhage, and neovascularization. The patient may have photophobia along with blurred vision.
♦ Glaucoma. Prolonged elevation of IOP can cause an arcuate scotoma. Poorly controlled glaucoma can also cause cupping of the optic disk, loss of peripheral vision, and reduced visual acuity. The patient may also see rainbow-colored halos around lights.
♦ Macular degeneration. Any degenerative process or disorder affecting the fovea centralis results in a central scotoma. Ophthalmoscopic examination reveals changes in the macular area. The patient may notice subtle changes in visual acuity, in color perception, and in the size and shape of objects.
♦ Migraine headache. Transient scintillating scotomas, usually bilateral and often homonymous, can occur during a classic migraine aura. Besides pain, characteristic associated symptoms include paresthesia of the lips, face, or hands; slight confusion; dizziness; and photophobia.
♦ Optic neuritis. Inflammation, degeneration, or demyelination of the optic nerve produces a central, circular, or centrocecal scotoma. The scotoma may be unilateral with involvement of one nerve, or bilateral with involvement of both nerves. It can vary in size, density, and symmetry. The patient may report severe visual loss or blurring, lasting up to 3 weeks, and pain—especially with eye movement. Common ophthalmoscopic findings include hyperemia of the optic disk, retinal vein distention, blurred disk margins, and filling of the physiologic cup.
♦ Retinal pigmentary degenerations. These disorders cause premature retinal cell changes leading to cell death. One disorder, retinitis pigmentosa, initially involves loss of peripheral rods; the resulting annular scotoma progresses concentrically until only a central field of vision (tunnel vision) remains. The earliest symptom—impaired night vision—appears during adolescence. Associated signs include narrowing of the retinal blood vessels and pallor of the optic disk. Eventually, with invasion of the macula, blindness may occur.
Locating scotomas
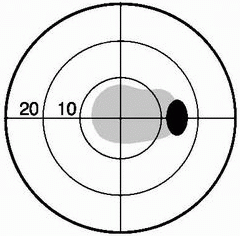
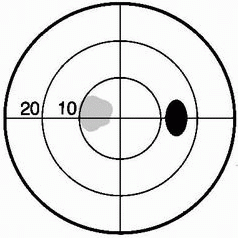
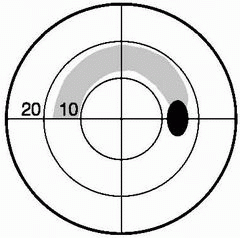
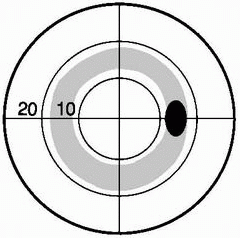
Scotomas, or “blind spots,” are classified according to the affected area of the visual field. The normal scotoma—shown in the temporal region of the right eye—appears in black in all the illustrations.
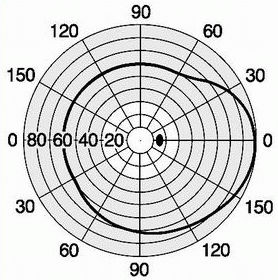 |
The normally present scotoma represents the position of the optic nerve head in the visual field. It appears between 10 and 20 degrees on this chart of the normal visual field.
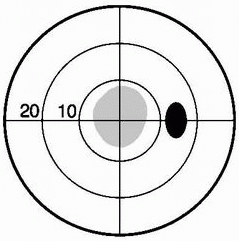 |
A paracentral scotoma affects an area of the visual field that is nasal or temporal to the point of central fixation.
 |
A central scotoma involves the point of central fixation. It’s always associated with decreased visual acuity.
 |
An arcuate scotoma arches around the fixation point, usually ending on the nasal side of the visual field.
 |
A centrocecal scotoma involves the point of central fixation and the area between the blind spot and the fixation point.
 |
An annular scotoma forms a circular defect around the fixation point. It’s common with retinal pigmentary degeneration.
SPECIAL CONSIDERATIONS
For the patient with an arcuate scotoma associated with glaucoma, emphasize regular testing of IOP and visual fields. For the patient with a disorder involving the fovea centralis (or the area surrounding it), teach him to periodically use the Amsler grid to detect progression of macular degeneration.
PEDIATRIC POINTERS
In young children, visual field testing is difficult and requires patience. Confrontation testing is the method of choice.
Scrotal swelling
Scrotal swelling occurs when a condition affecting the testicles, epididymis, or scrotal skin produces edema or a mass; the penis may be involved. Scrotal swelling can affect males of any age. It can be unilateral or bilateral and painful or painless.
The sudden onset of painful scrotal swelling suggests torsion of a testicle or testicular appendages, especially in a prepubescent male. This emergency requires immediate surgery to
untwist and stabilize the spermatic cord or to remove the appendage.
untwist and stabilize the spermatic cord or to remove the appendage.
 If severe pain accompanies scrotal swelling, ask when the swelling began. Using a Doppler stethoscope, evaluate blood flow to the testicle. If it’s decreased or absent, suspect testicular torsion and prepare the patient for surgery. Withhold food and fluids, insert an I.V. catheter, and apply an ice pack to the scrotum to reduce pain and swelling. An attempt may be made to untwist the cord manually, but even if this is successful, the patient may still require surgery for stabilization.
If severe pain accompanies scrotal swelling, ask when the swelling began. Using a Doppler stethoscope, evaluate blood flow to the testicle. If it’s decreased or absent, suspect testicular torsion and prepare the patient for surgery. Withhold food and fluids, insert an I.V. catheter, and apply an ice pack to the scrotum to reduce pain and swelling. An attempt may be made to untwist the cord manually, but even if this is successful, the patient may still require surgery for stabilization.HISTORY AND PHYSICAL EXAMINATION
If the patient isn’t in distress, proceed with the history. Ask about injury to the scrotum, urethral discharge, cloudy urine, increased urinary frequency, and dysuria. Is the patient sexually active? When was his last sexual contact? Does he have a history of sexually transmitted disease? Find out about recent illnesses, particularly mumps. Does he have a history of prostate surgery or prolonged catheterization? Does changing his body position or level of activity affect the swelling?
Take the patient’s vital signs, especially noting fever, and palpate his abdomen for tenderness. Then examine the entire genital area. Assess the scrotum with the patient in supine and standing positions. Note its size and color. Is the swelling unilateral or bilateral? Do you see signs of trauma or bruising? Are there rashes or lesions present? Gently palpate the scrotum for a cyst or a lump. Note especially tenderness or increased firmness. Check the testicles’ position in the scrotum. Finally, transilluminate the scrotum to distinguish a fluid-filled cyst from a solid mass. (A solid mass can’t be transilluminated.)
MEDICAL CAUSES
♦ Elephantiasis of the scrotum. With this disorder (common in some tropical countries), infection by a filaria worm obstructs lymphatic drainage, causing chronic gross scrotal edema and pain. Associated findings include other areas of pitting and, eventually, brawny edema (especially the legs), thickened subcutaneous tissue, hyperkeratosis, and skin fissures.
♦ Epididymal cysts. Located in the head of the epididymis, these cysts produce painless scrotal swelling.
♦ Epididymal tuberculosis. This disorder produces an enlarged scrotal mass separated from the testicle. Other findings include palpable beading along the vas deferens, induration of the prostate or seminal vesicles, and pus or tubercle bacilli in the urine.
♦ Epididymitis. Key features of inflammation are pain, extreme tenderness, and swelling in the groin and scrotum. The patient waddles to avoid pressure on the groin and scrotum during walking. He may have high fever, malaise, urethral discharge and cloudy urine, and lower abdominal pain on the affected side. His scrotal skin may be hot, red, dry, flaky, and thin.
♦ Gumma. This rare, painless nodule—usually associated with benign tertiary syphilis—can affect any bone or organ. If it affects the testicle, it causes edema.
♦ Hernia. Herniation of bowel into the scrotum can cause swelling and a soft or unusually firm scrotum. Occasionally, bowel sounds can be auscultated in the scrotum.
♦ Hydrocele. Fluid accumulation produces gradual scrotal swelling that’s usually painless. The scrotum may be soft and cystic or firm and tense. Palpation reveals a round, nontender scrotal mass.
♦ Idiopathic scrotal edema. Swelling occurs quickly with this disorder and usually disappears within 24 hours. The affected testicle is pink.
♦ Orchitis (acute). Mumps, syphilis, or tuberculosis may precipitate this disorder, which causes sudden painful swelling of one or, at times, both testicles. Related findings include a hot, reddened scrotum; fever of up to 104° F (40° C); chills; lower abdominal pain; nausea; vomiting; and extreme weakness. Urinary signs are usually absent.
♦ Scrotal burns. Burns cause swelling within 24 hours of injury. Depending on the burn’s severity, associated findings may include severe pain, erythema, chafing, tissue sloughing, and maceration with a weeping exudate.
♦ Scrotal trauma. Blunt trauma causes scrotal swelling with bruising and severe pain. The scrotum may appear dark or bluish.
♦ Spermatocele. This usually painless cystic mass lies above and behind the testicle and contains opaque fluid and sperm. Its onset may be acute or gradual. Less than 1 cm in diameter, it’s movable and may be transilluminated.
♦ Testicular torsion. Most common before puberty, this urologic emergency causes scrotal swelling; sudden, severe pain; and, possibly,
elevation of the affected testicle within the scrotum. It may also cause nausea and vomiting.
elevation of the affected testicle within the scrotum. It may also cause nausea and vomiting.
♦ Testicular tumor. Typically painless, smooth, and firm, a testicular tumor produces swelling and a sensation of excessive weight in the scrotum.
♦ Torsion of a hydatid of Morgagni. Torsion of this small, pea-sized cyst severs its blood supply, causing a hard, painful swelling on the testicle’s upper pole.
OTHER CAUSES
♦ Surgery. An effusion of blood from surgery can produce a hematocele, leading to scrotal swelling.
SPECIAL CONSIDERATIONS
Keep the patient on bed rest and administer an antibiotic. Provide adequate fluids, fiber, and stool softeners. Place a rolled towel between the patient’s legs and under the scrotum to help reduce severe swelling. If the patient has mild or moderate swelling, advise him to wear a loose-fitting athletic supporter lined with a soft cotton dressing. For several days, administer an analgesic to relieve his pain. Encourage sitz baths, and apply heat or ice packs to decrease inflammation.
Prepare the patient for needle aspiration of fluid-filled cysts and other diagnostic tests, such as lung tomography and computed tomography scan of the abdomen, to rule out malignant tumors.
PEDIATRIC POINTERS
A thorough physical assessment is especially important for children with scrotal swelling, who may be unable to provide history data. In children up to age 1, a hernia or hydrocele of the spermatic cord may stem from abnormal fetal development. In infants, scrotal swelling may stem from ammonia-related dermatitis, if diapers aren’t changed often enough. In prepubescent males, it usually results from torsion of the spermatic cord.
Other disorders that can produce scrotal swelling in children include epididymitis (rare before age 10), traumatic orchitis from contact sports, and mumps, which usually occurs after puberty.
PATIENT COUNSELING
Encourage the patient to perform testicular selfexaminations at home. (See How to examine your testicles.)
Seizures, absence
Absence seizures are benign, generalized seizures thought to originate subcortically. These brief episodes of unconsciousness usually last 3 to 20 seconds and can occur 100 or more times a day, causing periods of inattention. Absence seizures usually begin between ages 4 and 12. Their first sign may be deteriorating school work and behavior. The cause of these seizures is unknown.
Absence seizures occur without warning. The patient suddenly stops all purposeful activity and stares blankly ahead, as if he were daydreaming. Absence seizures may produce automatisms, such as repetitive lip smacking, or mild clonic or myoclonic movements, including mild jerking of the eyelids. The patient may drop an object that he’s holding, and muscle relaxation may cause him to drop his head or arms or to slump. After the attack, the patient resumes activity, typically unaware of the episode.
Absence status, a rare form of absence seizure, occurs as a prolonged absence seizure or as repeated episodes of these seizures. Usually not life-threatening, it occurs most commonly in patients who have previously experienced absence seizures.
HISTORY AND PHYSICAL EXAMINATION
If you suspect a patient is having an absence seizure, evaluate its occurrence and duration by reciting a series of numbers and then asking him to repeat them after the attack ends. If the patient has had an absence seizure, he’ll be unable to do this. Alternatively, if the seizures are occurring within minutes of each other, ask the patient to count for about 5 minutes. He’ll stop counting during a seizure and resume when it’s over. Look for accompanying automatisms. Find out if the family has noticed a change in behavior or deteriorating schoolwork.
MEDICAL CAUSES
♦ Idiopathic epilepsy. Some forms of absence seizure are accompanied by learning disabilities.
PATIENT COUNSELING
Explain the purpose of any diagnostic tests, such as computed tomography scans, magnetic resonance imaging, and EEGs. Teach the patient and his family about these seizures and how to recognize their onset, pattern, and
duration. Include the child’s teacher and school nurse in the teaching process, if possible. If the seizures are being controlled with drug therapy, emphasize the importance of strict compliance.
duration. Include the child’s teacher and school nurse in the teaching process, if possible. If the seizures are being controlled with drug therapy, emphasize the importance of strict compliance.
Dear Patient:
To help detect abnormalities early, you should examine your testicles once a month. (Perform this examination on the same date every month.) The best time to examine your testicles is during or after a hot bath or shower. The heat causes the testicles to descend and relaxes the scrotum; this makes finding abnormalities easier.
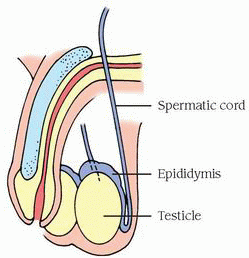 |
Follow these simple instructions for performing a self-examination, using the illustration (upper right) to locate anatomic landmarks.
Check the scrotum
With one hand, lift your penis and check your scrotum (the pouch of skin containing the testicles and parts of the spermatic cords) for any change in shape or size and for reddened, distended veins. Expect the scrotum’s left side to hang slightly lower than the right.
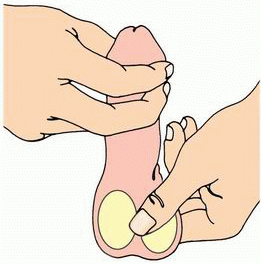 |
Check each testicle
Place your left thumb on the front of your left testicle and your index and middle fingers behind it (as shown middle right). Gently but firmly roll the testicle between your thumb and fingers. Then use your right hand to examine your right testicle in the same manner. Your testicles should feel smooth, rubbery, slightly tender, and movable within the scrotum.
If you notice any lumps, masses, or other changes, notify your physician.
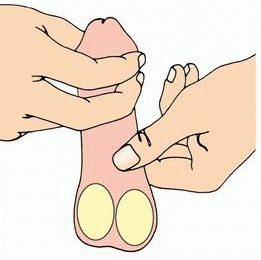 |
Check each spermatic cord
Locate the epididymis, the cordlike structure at the back of your testicles. Then locate the spermatic cord extending upward from it (as shown bottom right).
Gently squeeze the spermatic cord above your left testicle between your thumb and the first two fingers of your left hand. Then repeat on the right side, using your right hand. Check for lumps and masses along the entire length of the cords.
This patient-teaching aid may be reproduced by office copier for distribution to patients. © 2011, Lippincott Williams & Wilkins.
Seizures, complex partial
A complex partial seizure occurs when a focal seizure begins in the temporal lobe and causes a partial alteration of consciousness—usually confusion. Psychomotor seizures can occur at any age, but incidence usually increases during adolescence and adulthood. Two-thirds of patients also have generalized seizures.
An aura—usually a complex hallucination, illusion, or sensation—typically precedes a psychomotor seizure. The hallucination may be audiovisual (images with sounds), auditory (abnormal or normal sounds or voices from the patient’s past), or olfactory (unpleasant smells, such as rotten eggs or burning materials). Other types of auras include sensations of déjà vu, unfamiliarity with surroundings, or depersonalization. Some patients become fearful or anxious, experience lip smacking, or have an unpleasant feeling in the epigastric region that rises toward the chest and throat. The patient usually recognizes the aura and lies down before losing consciousness.
A period of unresponsiveness follows the aura. The patient may experience automatisms, appear dazed and wander aimlessly, perform inappropriate acts (such as undressing in public), be unresponsive, utter incoherent phrases, or (rarely) go into a rage or tantrum. After the seizure, the patient is confused, drowsy, and doesn’t remember the seizure. Behavioral automatisms rarely last longer than 5 minutes, but postseizure confusion, agitation, and amnesia may persist.
Between attacks, the patient may exhibit slow and rigid thinking, outbursts of anger and aggressiveness, tedious conversation, a preoccupation with naive philosophical ideas, diminished libido, mood swings, and paranoid tendencies.
HISTORY AND PHYSICAL EXAMINATION
If you witness a complex partial seizure, never attempt to restrain the patient. Instead, lead him gently to a safe area. (Exception: Don’t approach him if he’s angry or violent.) Calmly encourage him to sit down, and remain with him until he’s fully alert. After the seizure, ask him if he experienced an aura. Record all observations and findings.
MEDICAL CAUSES
♦ Brain abscess. If the brain abscess is in the temporal lobe, complex partial seizures commonly occur after the abscess disappears. Related problems may include headache, nausea, vomiting, generalized seizures, and a decreased level of consciousness (LOC). The patient may also develop central facial weakness, auditory receptive aphasia, hemiparesis, and ocular disturbances.
♦ Head trauma. Severe trauma to the temporal lobe (especially from a penetrating injury) can produce complex partial seizures months or years later. The seizures may decrease in frequency and eventually stop. Head trauma also causes generalized seizures and behavior and personality changes.
♦ Herpes simplex encephalitis. The herpes simplex virus commonly attacks the temporal lobe, resulting in complex partial seizures. Other features include fever, headache, coma, and generalized seizures.
♦ Temporal lobe tumor. Complex partial seizures may be the first sign of this disorder. Other signs and symptoms include headache, pupillary changes, and mental dullness. Increased intracranial pressure may cause a decreased LOC, vomiting and, possibly, papilledema.
SPECIAL CONSIDERATIONS
After the seizure, remain with the patient to reorient him to his surroundings and to protect him from injury. Keep him in bed until he’s fully alert, and remove harmful objects from the area. Offer emotional support to the patient and his family, and teach them how to cope with seizures.
Prepare the patient for diagnostic tests, such as EEG, computed tomography scans, or magnetic resonance imaging.
PEDIATRIC POINTERS
Complex partial seizures in children may resemble absence seizures. They can result from birth injury, abuse, infection, or cancer. In about one-third of patients, their cause is unknown.
Repeated complex partial seizures commonly lead to generalized seizures. The child may experience a slight aura, which is rarely as clearly defined as that seen with generalized tonicclonic seizures.
Seizures, generalized tonic-clonic
Like other types of seizures, generalized tonicclonic seizures are caused by the paroxysmal, uncontrolled discharge of central nervous system (CNS) neurons, leading to neurologic dysfunction. Unlike most other types of seizures, however, this cerebral hyperactivity isn’t confined to the original focus or to a localized area but extends to the entire brain.
A generalized tonic-clonic seizure may begin with or without an aura. As seizure activity spreads to the subcortical structures, the patient loses consciousness, falls to the ground, and may utter a loud cry that’s precipitated by air rushing from the lungs through the vocal cords. His body stiffens (tonic phase), then undergoes rapid, synchronous muscle jerking and hyperventilation (clonic phase). Tongue biting, incontinence, diaphoresis, profuse salivation, and signs of respiratory distress may also occur. The seizure usually stops after 2 to 5 minutes. The patient then regains consciousness but displays confusion. He may complain of headache, fatigue, muscle soreness, and arm and leg weakness.
Generalized tonic-clonic seizures usually occur singly. The patient may be asleep or awake and active. (See What happens during a generalized tonic-clonic seizure, page 620.) Possible complications include respiratory arrest due to airway obstruction from secretions, status epilepticus (occurring in 5% to 8% of patients), head or spinal injuries and bruises, Todd’s paralysis and, rarely, cardiac arrest. Lifethreatening status epilepticus is marked by prolonged seizure activity or by rapidly recurring seizures with no intervening periods of recovery. It’s most commonly triggered by abrupt discontinuation of anticonvulsant therapy.
Generalized seizures may be caused by a brain tumor, vascular disorder, head trauma, infection, metabolic defect, drug or alcohol withdrawal syndrome, exposure to toxins, or a genetic defect. Generalized seizures may also result from a focal seizure. With recurring seizures, or epilepsy, the cause may be unknown.
 If you witness the beginning of the seizure, first check the patient’s airway, breathing, and circulation, and ensure that the cause isn’t asystole or a blocked airway. Stay with the patient and ensure a patent airway. Focus your care on observing the seizure and protecting the patient. Place a towel under his head to prevent injury, loosen his clothing, and move any sharp or hard objects out of his way. Never try to restrain the patient or force a hard object into his mouth; you might chip his teeth or fracture his jaw. Only at the start of the ictal phase can you safely insert a soft object into his mouth.
If you witness the beginning of the seizure, first check the patient’s airway, breathing, and circulation, and ensure that the cause isn’t asystole or a blocked airway. Stay with the patient and ensure a patent airway. Focus your care on observing the seizure and protecting the patient. Place a towel under his head to prevent injury, loosen his clothing, and move any sharp or hard objects out of his way. Never try to restrain the patient or force a hard object into his mouth; you might chip his teeth or fracture his jaw. Only at the start of the ictal phase can you safely insert a soft object into his mouth.If possible, turn the patient to one side during the seizure to allow secretions to drain and to prevent aspiration. Otherwise, do this at the end of the clonic phase when respirations return. (If they fail to return, check for airway obstruction and suction the patient if necessary. Cardiopulmonary resuscitation, intubation, and mechanical ventilation may be needed.)
Protect the patient after the seizure by providing a safe area in which he can rest. As he awakens, reassure and reorient him. Check his vital signs and neurologic status. Be sure to carefully record these data and your observations during the seizure.
If the seizure lasts longer than 4 minutes or if a second seizure occurs before full recovery from the first, suspect status epilepticus. Establish an airway, insert an I.V. catheter, give supplemental oxygen, and begin cardiac monitoring. Draw blood for appropriate studies. Turn the patient on his side, with his head in a semi-dependent position, to drain secretions and prevent aspiration. Periodically turn him to the opposite side, check his arterial blood gas levels for hypoxemia, and administer oxygen by mask, increasing the flow rate if necessary. Administer diazepam or lorazepam by slow I.V. push, repeated two or three times at 10- to 20-minute intervals, to stop the seizures. If the patient isn’t known to have epilepsy, an I.V. bolus of dextrose 50% (50 ml) with thiamine (100 mg) may be ordered. Dextrose may stop the seizures if the patient has hypoglycemia. If his thiamine level is low, also give thiamine to guard against further damage.
If the patient is intubated, expect to insert a nasogastric (NG) tube to prevent vomiting and aspiration. Be aware that if the patient hasn’t been intubated, the NG tube itself can trigger the gag reflex and cause vomiting. Be sure to record your observations and the intervals between seizures.
HISTORY AND PHYSICAL EXAMINATION
If you didn’t witness the seizure, obtain a description from the patient’s companion. Ask when the seizure started and how long it lasted. Did the patient report any unusual sensations before the seizure began? Did the seizure start
in one area of the body and spread, or did it affect the entire body right away? Did the patient fall on a hard surface? Did his eyes or head turn? Did he turn blue? Did he lose bladder control? Did he have any other seizures before recovering?
in one area of the body and spread, or did it affect the entire body right away? Did the patient fall on a hard surface? Did his eyes or head turn? Did he turn blue? Did he lose bladder control? Did he have any other seizures before recovering?
What happens during a generalized tonic-clonic seizure
Before the seizure
Prodromal signs and symptoms, such as myoclonic jerks, throbbing headache, and mood changes, may occur over several hours or days. The patient may have premonitions of the seizure. For example, he may report an aura, such as seeing a flashing light or smelling a characteristic odor.
During the seizure
If a generalized seizure begins with an aura, this indicates that irritability in a specific area of the brain quickly became widespread. Common auras include palpitations, epigastric distress rapidly rising to the throat, head or eye turning, and sensory hallucinations.
Next, loss of consciousness occurs as a sudden discharge of intense electrical activity overwhelms the brain’s subcortical center. The patient falls and experiences brief, bilateral myoclonic contractures. Air forced through spasmodic vocal cords may produce a birdlike, piercing cry.
During the tonic phase, skeletal muscles contract for 10 to 20 seconds. The patient’s eyelids are drawn up, his arms are flexed, and his legs are extended. His mouth opens wide, then snaps shut; he may bite his tongue. His respirations cease because of respiratory muscle spasm, and initial pallor of the skin and mucous membranes (the result of impaired venous return) changes to cyanosis secondary to apnea. The patient arches his back and slowly lowers his arms (as shown below). Other effects include dilated, nonreactive pupils; greatly increased heart rate and blood pressure; increased salivation and tracheobronchial secretions; and profuse diaphoresis.
 |
During the clonic phase, lasting about 60 seconds, mild trembling progresses to violent contractures or jerks. Other motor activity includes facial grimaces (with possible tongue biting) and violent expiration of bloody, foamy saliva from clonic contractures of thoracic cage muscles. Clonic jerks slowly decrease in intensity and frequency. The patient is still apneic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


