Source: Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990; 47:543–9.
The concept of pharmaceutical care struck a responsive chord with many practitioners. It was termed pharmacy’s mission for the 1990s, and pharmaceutical care and the quality of care to patients were linked.9
Pharmaceutical Care Sprouts in Community Pharmacies
Over the years, the contributions that pharmacists can make to improving drug therapy have been recognized in federal laws. In 1974 and again in 1987, the federal government ruled that consultant pharmacists must check the medication regimens of nursing home residents each month and ask the physician to address any problems detected during these reviews.
In 1990, the US Congress passed a law that pharmacists must offer counsel to ambulatory Medicaid patients about their medications. This requirement was extended to all patients by many state boards of pharmacy (see Chapter 3, Pharmacy Law and Regulation). The federal government thus recognized that (1) drugs are not always used properly, even when physicians order them, and (2) pharmacists have the knowledge and expertise to help both the physician and the consumer make sure medications are used properly.
In 1995, an important article in the Archives of Internal Medicine confirmed and quantified the extent of problems related to suboptimal medication use.10 Johnson and Bootman showed that medications were a serious and substantial cause of problems among Americans, a finding that was later supported by reports from the respected Institute of Medicine. In fact, Johnson and Bootman calculated, for every dollar spent on medications for ambulatory Americans (those using the medications outside hospitals and nursing homes), another dollar was spent for medication-related problems, including deaths, hospitalizations, physician office visits, and other medications and treatments.10,11 This calculation was updated in the Journal of the American Pharmaceutical Association by Ernst and Grizzle in 2001, and it had more than doubled, from $76 billion in the 1995 study to $177 billion.12
The Institute of Medicine’s 2006 report cited a study that found that each preventable adverse drug event in a hospital adds $8,750 (in 2006 dollars) to the cost of a hospital stay. The report estimated the total costs for these events, conservatively, at $3.5 billion.13 One of the solutions to this problem, the report said, is increased communication with patients by pharmacists and other allied health care providers.
In the late 1990s, recognition of these problems led innovative practitioners and the APhA Foundation to implement several community-based pharmaceutical care projects.14–17 One of the more important efforts began in 1997 when the city of Asheville, N.C., began contracting with local pharmacists to provide pharmaceutical care services to employees and their dependents with diabetes. Joined later by the Mission St. Joseph’s Health System in that city, the Asheville Project demonstrated that pharmacists could reduce the overall cost of health care and improve the lives and work productivity of people with diabetes.
The APhA Foundation expanded the demonstration of pharmacists’ services with a series of Project ImPACT (Improving Persistence And Compliance with Therapy) and Patient Self-Management Project studies in the late 1990s and early years of the 21st century.18 Pharmacists—acting as pharmacotherapy experts, educators, and coaches to patients with chronic diseases such as diabetes, hyperlipidemia, asthma, hypertension, coronary artery disease, and depression—helped people make therapeutic lifestyle changes (getting more exercise, stopping smoking, reducing alcohol intake, and losing weight), take their medications as prescribed, avoid or minimize disease, and in general have a better quality of life.
Medication Therapy Management
In December 2003, the US Congress passed the Medicare Prescription Drug, Improvement, and Modernization Act (MMA), creating Part D of the Medicare program (see Chapter 3). As a result of the recognition of medication-related problems and the important roles pharmacists could play in preventing and resolving them, this law created a medication therapy management (MTM)19 services benefit for patients who have several chronic diseases, take multiple medications for those diseases, and have expected annual drug costs above a level that is adjusted annually. By recognizing pharmacists as providers under Medicare and establishing a revenue stream, MTM services have opened doors to change a number of pharmacy practice settings into the health and wellness centers that many pharmacists have dreamed of. While the uptake on MTM services was initially slow and limited to community pharmacies, many believe that such patient-centered services—rather than the traditional focus on drug preparation—will define the future roles of pharmacists in many practice settings. If true, technicians will need to be proficient in drug-distribution tasks so that pharmacists will be able to spend time with patients without the many interruptions that often characterize the drug-preparation and distribution process.
Core Elements of an MTM Services Model in Pharmacy Practice
Pharmacy is now working to incorporate MTM services into everyday practice in a broad variety of settings. Soon after passage of MMA, APhA convened meetings of key pharmacy associations to develop a consensus-wide definition of MTM services. The result is the language shown in Table 6-2.
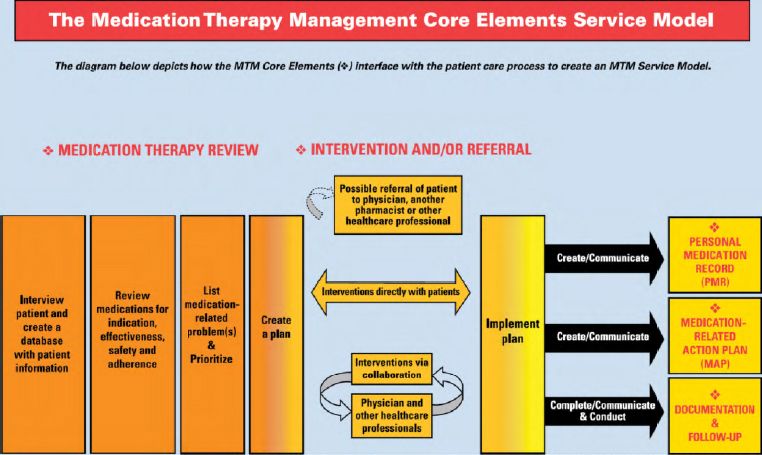
To fulfill these MTM tasks, the pharmacy profession also developed a framework for delivering MTM services, referred to as the MTM Core Elements, which was published in the Journal of the American Pharmacists Association in 2008.20 This framework includes the following components:
- Medication therapy review (MTR)
- Personal medication record (PMR)
- Medication-related action plan (MAP)
- Intervention and/or referral
- Documentation and follow-up
Figure 6-1 shows how the MTM Core Elements fit into the patient-care process to build the MTM service model. Pharmacists often rely on technicians to participate in these foundational components of MTM services, whether in spearheading the drug-preparation phase of the dispensing process, participating in medication histories and patient scheduling, or facilitating patient communication. It will be helpful in your practice to understand each of the core elements of MTM services.
Medication Therapy Management is a distinct service or group of services that optimize therapeutic outcomes for individual patients. Medication Therapy Management services are independent of, but can occur in conjunction with, the provision of a medication product.
Medication Therapy Management encompasses a broad range of professional activities and responsibilities within the licensed pharmacist’s, or other qualified health care provider’s, scope of practice. These services include but are not limited to the following, according to the individual needs of the patient:
a. Performing or obtaining necessary assessments of the patient’s health status
b. Formulating a medication treatment plan
c. Selecting, initiating, modifying, or administering medication therapy
d. Monitoring and evaluating the patient’s response to therapy, including safety and effectiveness
e. Performing a comprehensive medication review to identify, resolve, and prevent medication-related problems, including adverse drug events
f. Documenting the care delivered and communicating essential information to the patient’s other primary care providers
g. Providing verbal education and training designed to enhance patient understanding and appropriate use of his/her medications
h. Providing information, support services, and resources designed to enhance patient adherence with his/her therapeutic regimens
i. Coordinating and integrating medication therapy management services within the broader health care management services being provided to the patient
A program that provides coverage for Medication Therapy Management services shall include:
a. Patient-specific and individualized services or sets of services provided directly by a pharmacist to the patient.a These services are distinct from formulary development and use, generalized patient ducation and information activities, and other population-focused quality assurance measures for medication use.
b. Face-to-face interaction between the patienta and the pharmacist as the preferred method of delivery. When patient-specific barriers to face-to-face communication exist, patients shall have equal access to appropriate alternative delivery methods. Medication Therapy Management programs shall include structures supporting the establishment and maintenance of the patient-pharmacist relationship.
c. Opportunities for pharmacists and other qualified health care providers to identify patients who should receive Medication Therapy Management services.
d. Payment for Medication Therapy Management services consistent with contemporary provider payment rates that are based on the time, clinical intensity, and resources required to provide services (e.g., Medicare Part A and/or Part B for Current Procedural Terminology [CPT] and Resource-Based Relative Value Scale [RBRVS]).
e. Processes to improve continuity of care, outcomes, and outcome measures.
— Approved July 27, 2004, by the Academy of Managed Care Pharmacy, the American Association of Colleges of Pharmacy, the American College of Apothecaries, the American College of Clinical Pharmacy, the American Society of Consultant Pharmacists, the American Pharmacists Association, the American Society of Health-System Pharmacists, the National Association of Boards of Pharmacy,b the National Association of Chain Drug Stores, the National Community Pharmacists Association, and the National Council of State Pharmacy Association Executives.
aIn some situations, Medication Therapy Management services may be provided to the caregiver or other persons involved in the care of the patient.
bOrganization policy does not allow the National Association of Boards of Pharmacy to take a position on payment issues.
Source: Bluml BM. Definition of medication therapy management: development of professionwide consensus. J Am Pharm Assoc. 2005;45:566–72.
Source: American Pharmacists Association and the National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0). J Am Pharm Assoc. 2008;48:341–53.
Medication Therapy Review
According to the MTM Core Elements, an MTR is defined as “a systematic process of collecting patient-specific information, assessing medication therapies to identify medication-related problems, developing a prioritized list of medication-related problems, and creating a plan to resolve them.”20 In this step of the framework, the patient presents all of his or her medications to the pharmacist, who assesses each agent and the way the patient is taking it—with the goal of identifying problems and potential solutions for the patient. In a traditional MTM service model, patients at risk for adverse events should receive a comprehensive MTR of all their medications at least once each year, with targeted MTRs—as needed throughout the year—focusing on individual medications.
Personal Medication Record
In the PMR step, a record is created of all of the patient’s medications, including prescription and nonprescription drugs, herbal products, and dietary supplements (Figure 6-2). The PMR is a written record developed in collaboration with the individual and his or her other health care providers; patients can use the PMR to help keep track of and manage their medications at home.



