, Kyu Eun Lee1 and June Young Choi1
(1)
Department of Surgery, Seoul National University Hospital, Seoul, Korea, Republic of (South Korea)
Abstract
The operating theater for robotic thyroidectomy is similar to those of open and endoscopic thyroidectomy. However, the robot system requires more space than that of endoscopic thyroidectomy; the room is usually larger than the ordinary operating theater.
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-642-37262-9_4) contains supplementary material, which is available to authorized users.
4.1 Basic Equipment and Instruments of Robotic Thyroidectomy
4.1.1 The Operation Theater
The operating theater for robotic thyroidectomy is similar to those of open and endoscopic thyroidectomy. However, the robot system requires more space than that of endoscopic thyroidectomy; the room is usually larger than the ordinary operating theater.
The room is also a clean and sterile space to perform the operation in aseptic manners.
4.1.2 da Vinci Si HD Surgical System (Intuitive, Sunnyvale, CA)

Fig. 4.1
The da Vinci system. (a) Robot system, (b) console, (c) da Vinci system before use
4.1.3 Instruments
4.1.3.1 Endoscope

Fig. 4.2
(a) Φ10–mm, 30° endoscope, (b) endoscope before use
4.1.3.2 Thyroid Pillow (Emtas, Korea)

Fig. 4.3
Thyroid pillow
4.1.3.3 EndoWrist Instruments
1 Maryland bipolar forceps, Φ8 mm
1 PrograspTM forceps, Φ8 mm
1 cautery hook, Φ8 mm
1 large needle driver, Φ8 mm
1 Harmonic®, Φ8 mm
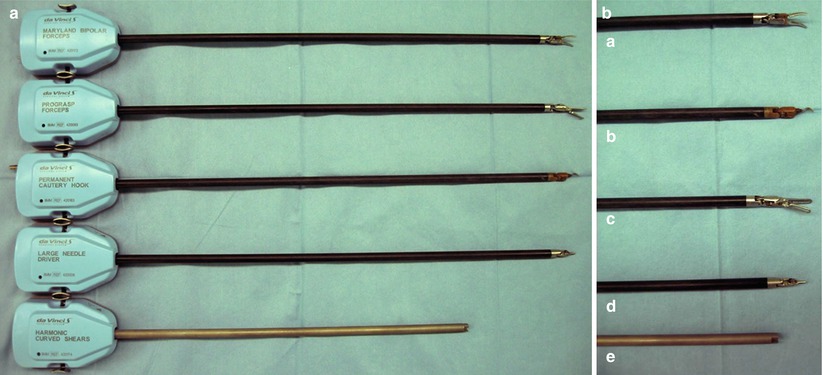
Fig. 4.4
EndoWrist instruments. (a) Maryland bipolar forceps, (b) PrograspTM forceps, (c) cautery hook, (d) large needle driver, (e) Harmonic®
4.1.3.4 Harmonic® (Ethicon Endo-surgery, Cincinnati, Ohio, USA)
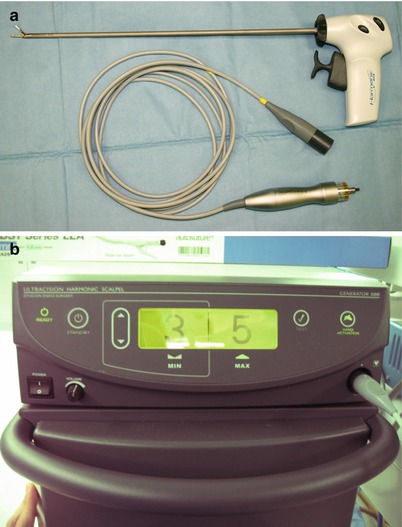
Fig. 4.5
Harmonic®. (a) hand piece, (b) generator
4.1.3.5 Vascular Tunneler (Gore-Tex)

Fig. 4.6
Vascular tunneler
4.1.3.6 Trocars
3 trocars, Ф8 mm
1 obturator
1 trocar, Ф12 mm
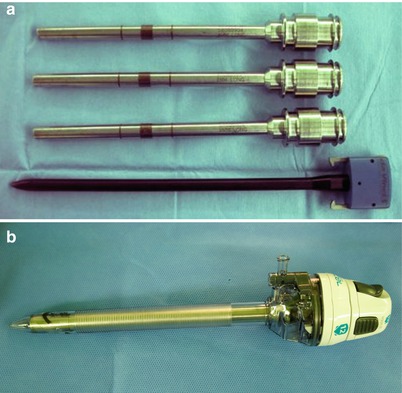
Fig. 4.7
Trocars. (a) Ф8-mm trocars and obturator, (b) Ф12-mm trocar
4.1.3.7 Endobag, 10 mm
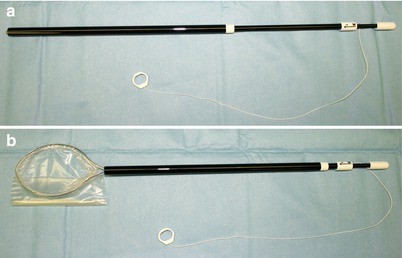
Fig. 4.8
Endobag. (a) closed, (b) open
4.1.3.8 Suction-Irrigator for Robotic Surgery
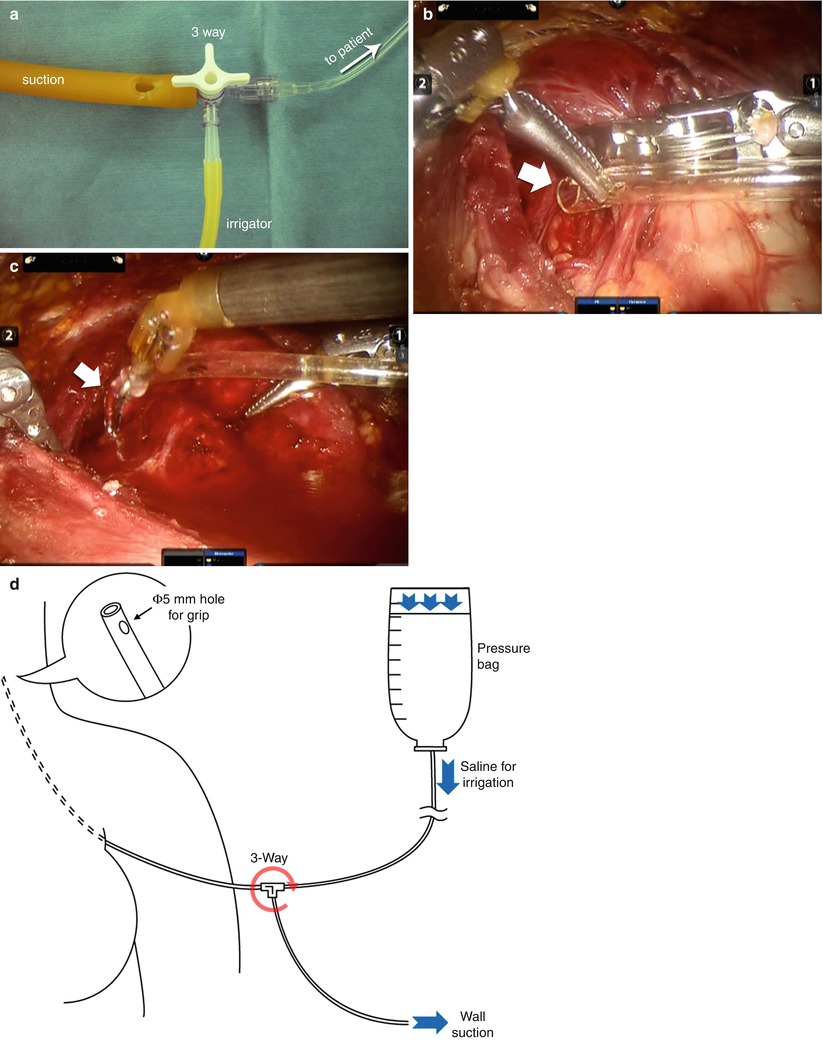
Fig. 4.9
Suction-irrigator. (a) Each part of suction-irrigator, (b) suction, (c) irrigation, (d) concept of suction-irrigator
4.1.3.9 Other Instruments
1 Thermos
1 CO2 line
1 alignment target
2 camera arm sterile adapter
1 camera sterile adapter

Fig. 4.10
Other instruments
4.2 Advantages and Disadvantages of Robotic Surgery
Unlike endoscopic instruments which are rigid and provide finite degrees of movement so that central and lateral node dissection poses a challenge, robotic system has advantages as follows: (1) the high-definition and three-dimensional magnified vision that can allow to identify the major structure and to operate easier and (2) the EndoWrist function of the instruments that can overcome limited access of confined operative field. With these reasons, robotic system is intuitive and easy to handle, and thus the learning curve is relatively short even in the beginner group.
However, there are some disadvantages of robotic surgery as follows: (1) lack of tactile sensation which can cause severe harm to the patient, (2) unawareness of severe complications since the operator is far from the patient, (3) impossibility of immediate reaction against unexpected events, and (4) very high cost even in developed countries. For the first disadvantage of lack of tactile sensation, robotic arms should not be moved out of surgeon’s view.
4.3 Patient Selection: Indications and Contraindications
Indications for robotic thyroidectomy are as follows: (1) cytologic diagnosed well-differentiated thyroid carcinoma such as papillary thyroid carcinoma and follicular thyroid carcinoma (the size of the cancer less than 2–3 cm is recommended), (2) the patient with Graves’ disease, (3) male patient with thyroid nodules that are needed to be excised, and (4) large size of the thyroid nodule more than 5 cm.
Absolute contraindications for robotic thyroidectomy are the patient with previous open neck surgery, thyroid malignancy which expected to be recurred easily (i.e., medullary thyroid cancer, advanced papillary thyroid cancer, and poorly differentiated thyroid cancer), with deep-lying carcinoma which is very close to the recurrent laryngeal nerve(Fig.4.11), and with overt breast malignancy.
Relatively not recommended patients for robotic thyroidectomy are with large size thyroid nodules over 8 cm in diameter, with thyroid malignancy with suspicious for lateral neck lymph node metastases and goiter with substernal portion. Previous breast operation due to breast carcinoma or breast augmentation is not to be considered as contraindication, and we experienced scores of patients with breast augmentation. Moreover, with BABA robotic thyroidectomy, lateral neck dissection can be effectively performed and patients suspicious for lateral neck metastases are not considered as relative contraindication recently.
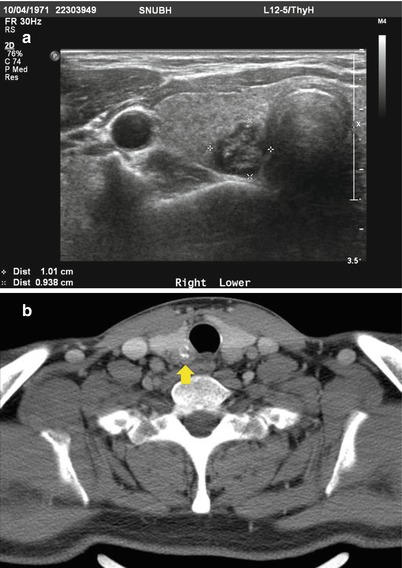
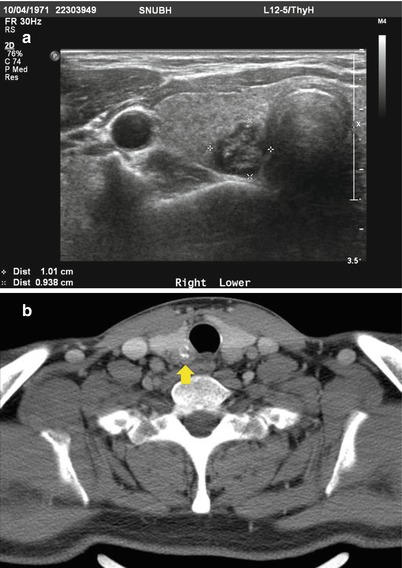
Fig. 4.11
(a) USG of deep-lying carcinoma, (b) CT scan of deep-lying carcinoma
4.4 Procedures of Bilateral Axillo-Breast Approach (BABA) Robotic Thyroidectomy
4.4.1 Positioning
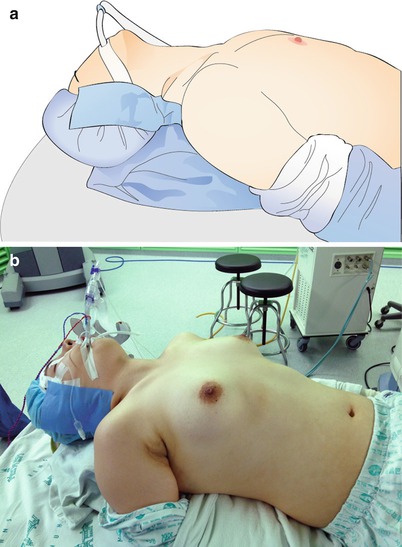
Fig. 4.12
Position of patient (a) illustration, (b) photo
The patient should be placed in the supine position on the operating table with the arms tucked close to the side.
A folded sheet or a pillow (Q-pillow) is placed vertically under the patient’s shoulders to extend the head and neck.
This neck extension should be performed with great caution and with the assistance of the anesthesiologists to ensure endotracheal tube is secured and avoid overextending the neck.
The patient’s head may be covered with a mesh cap to avoid contamination of the field. An adhesive tape may be applied to cover up both ears.
4.4.2 Skin Preparation and Draping

Fig. 4.13
Skin preparation
The operative field is then prepared with a routine surgical maneuver.
The anterior cervical region is prepared bilaterally from the angles of the mandible, posteriorly to the anterior borders of the trapezius, and inferiorly to the xiphoid process of sternum.
Axillae and proximal regions of arms are also prepared with antiseptic solution.
When the surgical prep solution is completely dry, an aseptic draping is applied using a universal draping package so that the anterior neck, bilateral axilla, and bilateral breast area are exposed.
We cover the patient’s head and face with a transparent plastic sheet in order to maintain the visual field of the patient’s face and the endotracheal tube. And a large sterile drape is covered over the patient’s shoulder, anterior chest wall, and the lower body to complete the draping.
4.4.3 Operating Room Setup
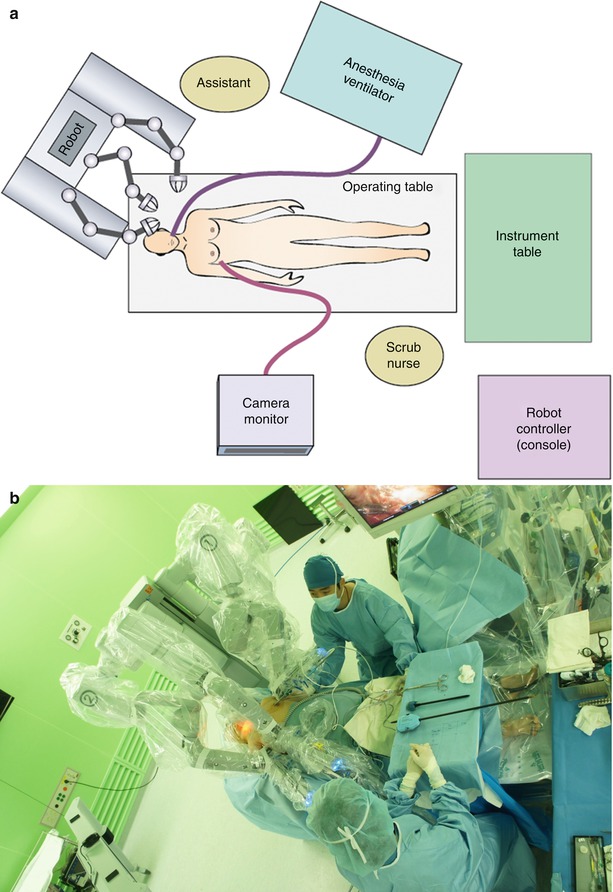

Fig. 4.14
(a) Schematic depiction and (b, c) the aerial view of the operating room setting for robotic thyroidectomy
4.4.4 Drawing Guidelines on the Body
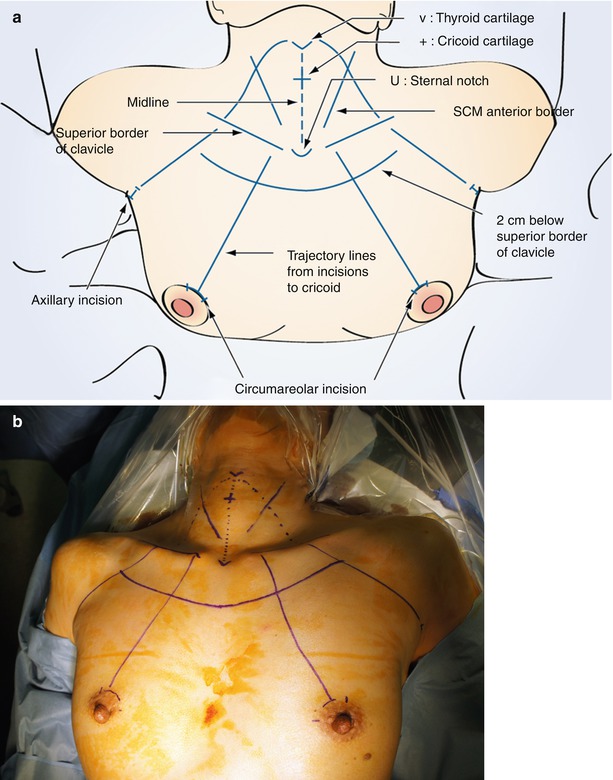
Fig. 4.15
Guidelines of BABA robotic thyroidectomy. (a) illustration, (b) photo
Guidelines are drawn along the landmarks of the chest and the neck (midline, thyroid cartilage (V), cricoid cartilage (+), anterior border of the SCM muscle, superior border of the clavicle, suprasternal notch (U), incisions, trajectory lines from the port site to the thyroid gland, and the working spaces).
4.4.5 Saline Injection

Fig. 4.16
(a) Epinephrine-saline injection and (b) 1:200,000 epinephrine-saline
Diluted epinephrine solution (1:200,000) is injected in the working area under the platysma in the neck and subcutaneously in the anterior chest. In the neck area, a “pinch and raise” maneuver of the skin facilitates the injection of saline into the subplatysmal area. This “hydrodissection” technique results in the formation of a saline pocket in the subplatysmal layer, which decreases the bleeding in the flap area and makes the subsequent dissection easier.
Inadvertent intravenous injection can be avoided by drawing the plunger backward slightly before making the injection.
4.4.6 Skin Incision and Blunt Dissection
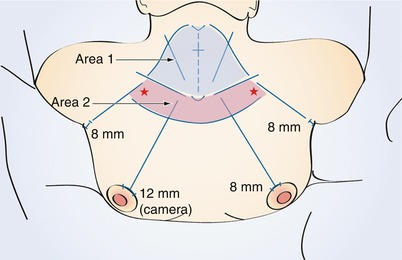
Fig. 4.17
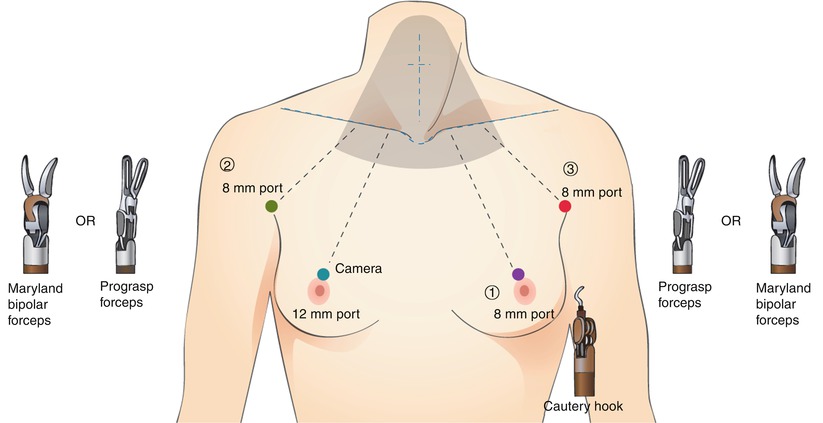
Port (incision) size of BABA robotic thyroidectomy
Circumareolar incisions are made bilaterally along the superomedial margin of each areola. Each incision is further deepened by electrocautery.
Blunt dissections are held with a straight mosquito hemostat, a long Kelly clamp, and a vascular tunneler to elevate the flap. When performing the blunt dissection near the sternal notch, one should try to avoid using excessive force. Dissection should start “area 2” (marked by ★) and elongate to “area 1”.
4.4.7 Port Insertion
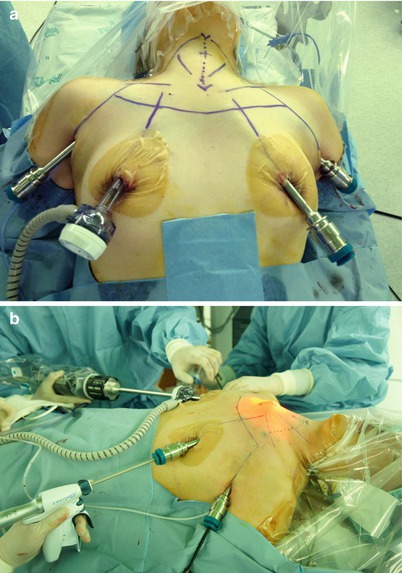
Fig. 4.18
(a) Port insertion and (b) sharp dissection with Harmonic®
After elevating the flap from the incision sites to the cricoid cartilage, the ports are inserted through the incisions. A 12-mm port is inserted through the right breast incision and an 8-mm port through the left breast incision. The camera is put through the 12 mm port to visually transmit the intracorporeal working space. And the ultrasonic shears are put through the 8-mm port. The working space is insufflated with CO2 gas at the pressure of 5–6 mmHg via a 12-mm port.
DuoDERM® is applied to the incision sites of the breasts in order to protect the nipples after making the port insertion.
When the ultrasonic shears come into the view, make a cut in the connective tissues (or trabeculae).
After making the working space on the anterior chest, two 8-mm axillary incisions are made.
Two 8-mm ports are inserted through the axillary incisions.
4.4.8 The Patient Cart Positioning

Fig. 4.19
Robot docking
The patient is positioned in the reverse Trendelenburg position at 30° angle.
The patient’s head is positioned towards the cart. Align the center column of the cart and the camera arm in a straight line with the camera port. Position the arms of patient cart as high as possible to clear patient’s head and operation table.
Note: All overhead lights, booms, and equipments should be temporarily placed aside to avoid contamination of the fields and robotic arms.
Patient cart is rolled into position on the patient’s left with the center column in line with the camera port, slightly angled to the operation table and patient’s head.
Robot docking: The camera arm is docked first. The camera port is, then, aligned to the target anatomy (i.e., thyroid gland) and the center column of the patient’s cart.
The instrumental arms are docked one by one. They should be kept in the center range of motion. The da Vinci instrumental ports are directed towards the center of the target anatomy (or cricoid cartilage) using setup joint release or port-clutch button.
da Vinci camera port: 12 mm (blue) camera port |
da Vinci instrument arm ① port: 8 mm (purple) instrumental port |
da Vinci instrument arm ② port: 8 mm (green) instrumental port |
da Vinci instrument arm ③ port: 8 mm (red) instrumental port |