Chapter 12 Right Upper Quadrant Pain in a 44-Year-Old Female (Case 2)
Editor’s note: Given the overlap of Cases 2 and 3 (Chapters 12 and 13), we suggest reading them as a single unit.
PATIENT CARE
Clinical Thinking
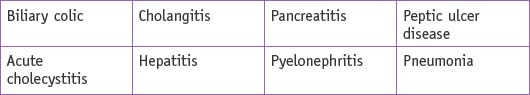
• Keep in mind conditions that can result in clinical deterioration or potential progression to sepsis without appropriate tx. These would include acute cholecystitis, ascending cholangitis, pyelonephritis, and a perforated ulcer.
• In a patient with jaundice, consider the possibility of a primary hepatic process, intrahepatic cholestasis, or obstruction of the biliary tree.
History
• As with all abdominal pain histories, focus on the location, character, duration, frequency, timing, and alleviating/aggravating factors. A hx of intermittent, postprandial, RUQ pain, radiating to the right subscapular regions is characteristic of biliary colic. Patients with acute cholecystitis may have had a hx of biliary colic, but now present with progressive, unrelenting pain and may have fever. Patients with pancreatitis have more persistent pain that often is centered more toward the epigastrium with radiation toward the back. Pain related to pyelonephritis is sensed more in the flank, and you should ask about associated dysuria and urinary frequency.
• Jaundice or other symptoms of hyperbilirubinemia, such as pale stools, dark urine, or pruritis can be seen in hepatitis and cholangitis and are also present in patients with an obstruction of the common bile duct due to a stone (choledocholithiasis) or mass (periampullary neoplasm).
• A careful social hx is important. Risk factors for hepatitis should be elicited, including IV drug use, recent personal or sexual contacts, medications, transfusions, alcohol use, or food exposures. Hepatitis is often accompanied by other prodromal constitutional symptoms such as fatigue, malaise, nausea, anorexia, and fever.
Physical Examination
• VS: Fever suggests an inflammatory process. Tachycardia and hypotension suggest sepsis or acute hemorrhage.
• Observation: Begin by getting a general sense of whether the patient appears acutely ill. Look for scleral icterus and jaundice. Patients with colicky pain often cannot find a position of comfort, whereas those with peritonitis tend to lie still.
• Auscultation: Decreased bowel sounds are associated more with a GI inflammatory process than a GU process.
• Palpation: A sharp, tender liver edge suggests hepatitis or hepatic congestion. Local peritoneal signs are common with acute cholecystitis, as is a Murphy’s sign. Patients with biliary colic generally have minimal to no tenderness on physical examination. Tenderness associated with jaundice and fever is indicative of cholangitis, while costovertebral angle (CVA) tenderness is prominent in pyelonephritis. A tender and palpable gallbladder is consistent with acute cholecystitis, whereas a non-tender, palpable gallbladder associated with jaundice may suggest bile duct obstruction due to pancreatic cancer (Courvoisier’s gallbladder). A pelvic examination is indicated in younger women to exclude pelvic inflammatory disease (PID) with associated secondary perihepatic inflammation (Fitz-Hugh-Curtis syndrome).
Tests for Consideration
| $35 | |
| $75 | |
| $45 | |
| $75 | |
| $80 | |
| $135 | |
| $38 |