Arthritis and tendinitis can easily be distinguished on physical examination. Tendinitis is painful on active movement but not on passive manipulation of the joint. Arthritis, on the other hand, is painful on both active and passive movement.
It is important to distinguish tendinitis from actual joint involvement.
Osteoarthritis (Degenerative Joint Disease [DJD])
The most common rheumatologic disease is osteoarthritis, also called DJD. Although not an exciting disease entity it is a major cause of disability.
 Osteoarthritis may be thought of as delayed payment for many years of joint abuse resulting in cartilage breakdown and loss of the normal mechanical relationships that underlie smooth joint function.
Osteoarthritis may be thought of as delayed payment for many years of joint abuse resulting in cartilage breakdown and loss of the normal mechanical relationships that underlie smooth joint function.
Knees and hips are common sites of involvement but no joint is immune. There is clearly a genetic component as well.
 Heberden’s and Bouchard’s nodes are common forms of osteoarthritis that present as deformed, nodular, bony swelling of the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints respectively.
Heberden’s and Bouchard’s nodes are common forms of osteoarthritis that present as deformed, nodular, bony swelling of the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints respectively.
Most common in elderly women, these nodes are not usually painful but may cause some loss of mobility.
 Baker’s cyst may complicate osteoarthritis of the knee.
Baker’s cyst may complicate osteoarthritis of the knee.
Almost any type of arthritis or injury to the knee may be associated with a Baker’s cyst.
The cyst, which is located in the popliteal fossa and communicates with the joint space, may rupture resulting in painful inflammation of the calf. Swelling, pain, and tenderness with difficulty bearing weight are common consequences.
 A ruptured Baker’s cyst may be erroneously confused with thrombophlebitis.
A ruptured Baker’s cyst may be erroneously confused with thrombophlebitis.
Ultrasound establishes the diagnosis of a ruptured Baker’s cyst.
 Charcot joint, a particularly destructive variant of osteoarthritis, refers to extensive joint damage due to loss of proprioceptive innervation secondary to underlying neurologic disease.
Charcot joint, a particularly destructive variant of osteoarthritis, refers to extensive joint damage due to loss of proprioceptive innervation secondary to underlying neurologic disease.
Loss of proprioception subjects the joint to unusual stress which results, ultimately, in total joint destruction. The location of the damaged joint depends upon the underlying neurologic disease.
 The most common cause of Charcot joint at the ankle is diabetes; at the knee, syphilis (tabes dorsalis); at the shoulder or the elbow, syringomyelia; at the wrist Hansen’s disease (leprosy, neuritic form).
The most common cause of Charcot joint at the ankle is diabetes; at the knee, syphilis (tabes dorsalis); at the shoulder or the elbow, syringomyelia; at the wrist Hansen’s disease (leprosy, neuritic form).
Olecranon Bursitis
Olecranon bursitis, inflammation of the olecranon bursa accompanied by fluid accumulation, swelling, and often redness, is usually the result of acute or chronic traumatic injury.
 Olecranon bursitis can be distinguished from arthritis of the elbow on physical examination: pronation and supination at the elbow joint cause pain if the elbow joint is involved; flexion and extension cause pain with both olecranon bursitis and elbow arthritis.
Olecranon bursitis can be distinguished from arthritis of the elbow on physical examination: pronation and supination at the elbow joint cause pain if the elbow joint is involved; flexion and extension cause pain with both olecranon bursitis and elbow arthritis.
 Olecranon bursitis may complicate rheumatoid arthritis (RA), often in relation to a subcutaneous nodule located over the bursa. Similarly, an overlying tophus in patients with gout may be associated with olecranon bursitis.
Olecranon bursitis may complicate rheumatoid arthritis (RA), often in relation to a subcutaneous nodule located over the bursa. Similarly, an overlying tophus in patients with gout may be associated with olecranon bursitis.
Olecranon bursitis may also be seen in alcoholics (elbows leaning on the bar!).
 Infection may complicate olecranon bursitis if the skin splits; Staphylococcus aureus is the usual organism.
Infection may complicate olecranon bursitis if the skin splits; Staphylococcus aureus is the usual organism.
Rheumatoid Arthritis (RA)
RA is a systemic disease principally involving the synovia and the joints. The cause is unknown, but heredity, autoimmunity, infectious agents, and environmental (smoking) factors may play a role. The disease is more common in women especially in younger patients. HLA-DR4 is a common histocompatibility antigen in RA patients.
 Rheumatoid factor (RF), an IgM antibody directed against gamma globulin, is useful diagnostically although the sensitivity and specificity depend on the prior probability of the disease.
Rheumatoid factor (RF), an IgM antibody directed against gamma globulin, is useful diagnostically although the sensitivity and specificity depend on the prior probability of the disease.
RF has been a biomarker for RA for over half a century. Recently, anticyclic citrullinated antibodies (anti-CCP) have been utilized as a diagnostic test. In patients with inflammatory arthritis the sensitivity of RF is about 70% and the specificity about 85%. The higher the titer the greater is the specificity of RF for RA. Anti-CCP antibodies appear to have a similar sensitivity and slightly greater specificity.
 RF is also positive in other collagen vascular diseases and in some chronic infectious diseases.
RF is also positive in other collagen vascular diseases and in some chronic infectious diseases.
Thus, Sjögren’s syndrome, Lupus, and subacute bacterial endocarditis are not infrequently RF positive.
 Approximately 50% of patients with RA are RF negative at the time of presentation.
Approximately 50% of patients with RA are RF negative at the time of presentation.
RF positivity subsequently develops in many patients as the disease progresses. The role of RF in the pathogenesis of RA, if any, is unknown.
 High-titer RF is associated with long-standing disease, aggressive joint destruction, subcutaneous nodules, vasculitis, and other extra-articular manifestations.
High-titer RF is associated with long-standing disease, aggressive joint destruction, subcutaneous nodules, vasculitis, and other extra-articular manifestations.
 The small joints of the hands, wrists, feet, and ankles are the most common sites of involvement in RA, although involvement of larger joints (knees, hips, elbows, and spine) also occurs.
The small joints of the hands, wrists, feet, and ankles are the most common sites of involvement in RA, although involvement of larger joints (knees, hips, elbows, and spine) also occurs.
 At the ankle the subtalar joints are most prominently involved affecting inversion and eversion more than flexion and extension.
At the ankle the subtalar joints are most prominently involved affecting inversion and eversion more than flexion and extension.
Characteristic deformities of the hands (ulna deviation, swan neck deformities), bilateral wrist involvement, and bony erosions on x-ray help establish the diagnosis.
 Morning stiffness, although not specific for RA, is characteristic.
Morning stiffness, although not specific for RA, is characteristic.
The stiffness is not fleeting; it lasts at least 1 hour.
 Although RA is most common in middle-aged women, extra-articular manifestations are more common in older men.
Although RA is most common in middle-aged women, extra-articular manifestations are more common in older men.
 Extra-articular manifestations are associated with severe articular disease, subcutaneous nodules, and high-titer rheumatoid factor (Table 3-1).
Extra-articular manifestations are associated with severe articular disease, subcutaneous nodules, and high-titer rheumatoid factor (Table 3-1).
Subcutaneous nodules occur most frequently on extensor surfaces around the hands and elbow, but histologically, similar rheumatoid nodules may occur in viscera as well, including the heart and lungs.
 Cardiac rheumatoid nodules, if strategically located around the conducting system, may cause heart block. Rheumatoid nodules may also, uncommonly, occur in the lung.
Cardiac rheumatoid nodules, if strategically located around the conducting system, may cause heart block. Rheumatoid nodules may also, uncommonly, occur in the lung.
 Rheumatoid pleural effusion is exudative and characterized by an extremely low glucose level, a low complement level, and a low pH.
Rheumatoid pleural effusion is exudative and characterized by an extremely low glucose level, a low complement level, and a low pH.
RF in the pleural fluid may be positive as well. The pH may be very low and may require repeated thoracentesis to avoid the development of a fibrothorax.
 Bi-basilar pulmonary fibrosis is the most common form of pulmonary involvement in RA.
Bi-basilar pulmonary fibrosis is the most common form of pulmonary involvement in RA.
It predisposes to pneumonia which may require a long course of treatment. This is particularly true in the face of immunosuppressive treatment or when neutropenia is present (Felty’s syndrome).
TABLE 3.1 Extra-articular Manifestations of RA
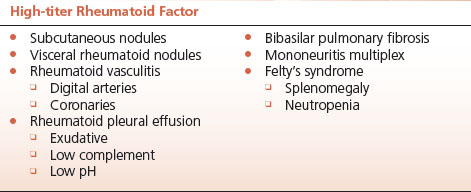
 Rheumatoid vasculitis occurs in the course of aggressive disease with high-titer rheumatoid factor, and is often associated with characteristic linear ulcerations around the digital arteries of the terminal phalanges of the hands.
Rheumatoid vasculitis occurs in the course of aggressive disease with high-titer rheumatoid factor, and is often associated with characteristic linear ulcerations around the digital arteries of the terminal phalanges of the hands.
 Rheumatoid vasculitis of the coronary arteries may cause myocardial ischemia and infarction, and vasculitis of the vasa vasorum of major motor nerves may cause nerve infarction and the corresponding syndrome of mononeuritis multiplex.
Rheumatoid vasculitis of the coronary arteries may cause myocardial ischemia and infarction, and vasculitis of the vasa vasorum of major motor nerves may cause nerve infarction and the corresponding syndrome of mononeuritis multiplex.
Rheumatoid vasculitis involving the kidneys is vanishingly rare.
 Felty’s syndrome, a triad including RA, splenomegaly, and neutropenia, occurs most commonly in long-standing RA with high-titer rheumatoid factor and other extra-articular manifestations.
Felty’s syndrome, a triad including RA, splenomegaly, and neutropenia, occurs most commonly in long-standing RA with high-titer rheumatoid factor and other extra-articular manifestations.
Antineutrophil antibodies and splenic sequestration explain the neutropenia.
 The possibility of septic arthritis masquerading as an RA flare should be considered, particularly in febrile patients with acute joint symptoms.
The possibility of septic arthritis masquerading as an RA flare should be considered, particularly in febrile patients with acute joint symptoms.
Since RA patients are often on an immunosuppressive regimen, joint infections that mimic a flare in the underlying disease may occur. These infections are usually caused by S. aureus, are associated with S. aureus bacteremia, and usually involve large joints such as hip or knee.
 Consider palindromic rheumatism in the differential diagnosis of RA in patients who have recurrent bouts of acute arthritis, are RF negative, and have no joint deformities.
Consider palindromic rheumatism in the differential diagnosis of RA in patients who have recurrent bouts of acute arthritis, are RF negative, and have no joint deformities.
Palindromic rheumatism is an acute inflammatory arthritis that is evanescent, recurs at variable intervals, and does not result in chronic joint deformity. The cause is unknown.
Adult Still’s Disease (Juvenile Rheumatoid Arthritis)
 Previously known as juvenile rheumatoid arthritis (JRA), Adult Still’s disease is a prominent cause of undiagnosed febrile illness in young adults.
Previously known as juvenile rheumatoid arthritis (JRA), Adult Still’s disease is a prominent cause of undiagnosed febrile illness in young adults.
 Diagnosis is purely clinical and supported by a distinctive fever pattern of two spikes per day and by the recognition of an evanescent pale erythematous maculopapular eruption, most commonly noted on the trunk, particularly in areas subject to pressure, such as the back.
Diagnosis is purely clinical and supported by a distinctive fever pattern of two spikes per day and by the recognition of an evanescent pale erythematous maculopapular eruption, most commonly noted on the trunk, particularly in areas subject to pressure, such as the back.
Other clues to the diagnosis include pharyngitis early in the course, arthralgias (and occasionally, arthritis), and very high levels of inflammatory indices including, importantly, very high ferritin levels. The latter are usually elevated out of proportion to other indices of inflammation. RF is negative.
Psoriatic Arthritis
 An asymmetric RF-negative, spondyloarthropathy, psoriatic arthritis affects principally the distal phalangeal joints and is associated with pitting of the finger nails and onycholysis.
An asymmetric RF-negative, spondyloarthropathy, psoriatic arthritis affects principally the distal phalangeal joints and is associated with pitting of the finger nails and onycholysis.
Although it is associated with psoriasis, in a small minority of patients, the joint disease may antedate the skin disease. It is commonly associated with HLA-B27 tissue type and sacroiliitis is a common accompaniment.
Reactive Arthritis
 Reactive arthritis (formerly known as Reiter’s syndrome) is an inflammatory response to an infection involving the bowel or urogenital tract.
Reactive arthritis (formerly known as Reiter’s syndrome) is an inflammatory response to an infection involving the bowel or urogenital tract.
The inciting infections include those caused by Chlamydia, Campylobacter, Shigella, Yersinia, and Salmonella species.
 The arthritis, which usually favors the large joints of the lower extremities, is mono- or oligoarticular and asymmetric; it is variable in severity, and occurs principally, but not exclusively, in patients positive for HLA-B27.
The arthritis, which usually favors the large joints of the lower extremities, is mono- or oligoarticular and asymmetric; it is variable in severity, and occurs principally, but not exclusively, in patients positive for HLA-B27.
The sacroiliac joints and the spine may be involved. The infection frequently precedes the arthritis by 1 to several weeks. Reactive arthritis following genitourinary infections has a marked male predominance (10 to 1 or greater), but the syndrome following enteric infections affects women equally.
 In addition to arthritis, the skin, the eyes, and the mucous membranes may be involved.
In addition to arthritis, the skin, the eyes, and the mucous membranes may be involved.
The triad of urethritis, arthritis, and conjunctivitis was previously known as Reiter’s syndrome.
 The characteristic skin lesions often associated with Reiter’s syndrome go by the colorful name keratoderma blenorrhagica; they are papulosquamous lesions with a serpiginous border classically located on the soles and palms.
The characteristic skin lesions often associated with Reiter’s syndrome go by the colorful name keratoderma blenorrhagica; they are papulosquamous lesions with a serpiginous border classically located on the soles and palms.
The eye inflammation involves the anterior chamber and may vary between mild conjunctivitis and severe anterior uveitis.
 Shallow erosions on the penis are known as circinate balanitis.
Shallow erosions on the penis are known as circinate balanitis.
In circumcised men lesions on the shaft of the penis resemble the keratoderma described above.
Crystal Deposition Arthridities: Uric Acid and Calcium Pyrophosphate
 Gout is a severe monoarticular arthritis, characteristically involving the metatarsophalangeal joint of the big toe (podagra).
Gout is a severe monoarticular arthritis, characteristically involving the metatarsophalangeal joint of the big toe (podagra).
The inflammation is so intense that even the bed sheets on the affected joint cannot be tolerated. The knee, the dorsum of the foot, the ankle joint (mortise and tenon portion affecting flexion and extension) and the instep are sites of involvement as well.
 The cause of gout is the precipitation of monosodium urate crystals in the synovial fluid of the involved joint. The needle shaped, negatively birefringent crystals (under polarized light) are phagocytized by neutrophils, initiating an inflammatory cascade within the joint space.
The cause of gout is the precipitation of monosodium urate crystals in the synovial fluid of the involved joint. The needle shaped, negatively birefringent crystals (under polarized light) are phagocytized by neutrophils, initiating an inflammatory cascade within the joint space.
Hyperuricemia is the underlying cause, but during an acute attack the serum uric acid level need not be elevated. Demonstration of phagocytized crystals in the joint fluid secures the diagnosis.
 Acute gouty attacks are frequently precipitated by unrelated hospitalization, surgery, and generous alcohol intake.
Acute gouty attacks are frequently precipitated by unrelated hospitalization, surgery, and generous alcohol intake.
It is not unusual for the first attack to occur when the patient wakes from anesthesia after surgery for an unrelated problem.
Ethanol increases plasma lactate which inhibits the tubular excretion of urate, a change that may precipitate an acute attack of gout.
The initiation of uricosuric therapy, or the inhibition of urate synthesis with allopurinol, mobilizes urate from tissue stores in tophi and may induce an acute attack. Prophylactic administration of colchicine or nonsteroidal anti-inflammatory agents is indicated when treatment to lower uric acid levels is initiated.
 Tophi, the precipitation of monosodium urate in soft tissues, develop after years of hyperuricemia; they occur most commonly adjacent to joints and in the skin of the ear lobe over the auricular cartilage.
Tophi, the precipitation of monosodium urate in soft tissues, develop after years of hyperuricemia; they occur most commonly adjacent to joints and in the skin of the ear lobe over the auricular cartilage.
Chronic tophaceous gout refers to polyarticular arthritis that occurs in relation to tophaceous deposits around joints which may result in destructive changes. In distinction to acute gout joint involvement with tophi may cause a chronic arthritis in multiple joints reminiscent of osteoarthritis.
 Gout is a disease of men and to a lesser extent of postmenopausal women. It is associated with obesity, hypertension, and diabetes mellitus.
Gout is a disease of men and to a lesser extent of postmenopausal women. It is associated with obesity, hypertension, and diabetes mellitus.
High-serum uric acid is a risk factor for cardiovascular disease, for reasons that remain obscure.
 Pseudogout is an acute arthritis usually involving the knee or wrist caused by the precipitation of calcium pyrophosphate dihydrate in the synovial space.
Pseudogout is an acute arthritis usually involving the knee or wrist caused by the precipitation of calcium pyrophosphate dihydrate in the synovial space.
It is a disease of the elderly, and men and women are equally affected. There is an association with hyperparathyroidism, hemochromatosis, and osteoarthritis. Decreased levels of phosphatases in the articular cartilage with aging may contribute.
 Acute inflammation is caused by the phagocytosis of rhomboid-shaped positively birefringent calcium pyrophosphate crystals (under polarized light).
Acute inflammation is caused by the phagocytosis of rhomboid-shaped positively birefringent calcium pyrophosphate crystals (under polarized light).
The disease is frequently chronic and may involve multiple joints. Treatment of the acute attack is similar to that of gout.
 Chondrocalcinosis, a linear deposition of calcium in the articular cartilage of the involved joint, helps confirm the diagnosis of pseudogout; chondrocalcinosis, however, is common in the elderly, frequently asymptomatic, and often occurs without pseudogout.
Chondrocalcinosis, a linear deposition of calcium in the articular cartilage of the involved joint, helps confirm the diagnosis of pseudogout; chondrocalcinosis, however, is common in the elderly, frequently asymptomatic, and often occurs without pseudogout.
ANCA-ASSOCIATED VASCULITIDES
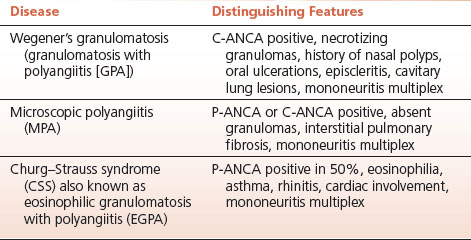
 Wegener’s granulomatosis (granulomatosis with polyangiitis [GPA]), microscopic polyangiitis (MPA), and Churg–Strauss syndrome (CSS) are the major vasculitides associated with positive antineutrophil cytoplasmic antibodies (Table 3-2).
Wegener’s granulomatosis (granulomatosis with polyangiitis [GPA]), microscopic polyangiitis (MPA), and Churg–Strauss syndrome (CSS) are the major vasculitides associated with positive antineutrophil cytoplasmic antibodies (Table 3-2).
Antineutrophil cytoplasmic antibodies (ANCAs), IgG autoantibodies directed against proteinase 3 (c-ANCA, cytoplasmic immunostaining), or myeloperoxidase (p-ANCA, perinuclear immunostaining), are present in the blood of many patients with systemic vasculitis. They are useful diagnostically even if their specific role in the pathogenesis of vasculitis is uncertain.
 c-ANCA is highly associated with Wegener’s granulomatosis; p-ANCA is less specific but associated more with MPA; the CSS may be associated with either.
c-ANCA is highly associated with Wegener’s granulomatosis; p-ANCA is less specific but associated more with MPA; the CSS may be associated with either.
TABLE 3.2 ANCA-associated Vasculitides
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


