8 Rheumatology
Osteoarthritis (OA)
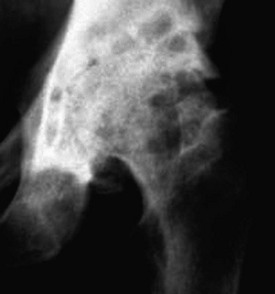
Describe the main radiological features of OA of the hip
The radiograph shows joint space narrowing, periarticular sclerosis, cyst formation and osteophytes. These are the four classic features of osteoarthritis (Fig. 8.1).
How would you assess this patient?
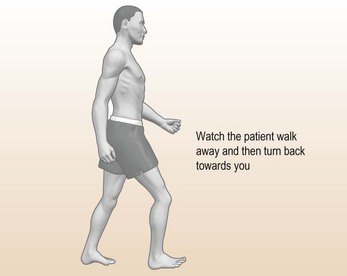
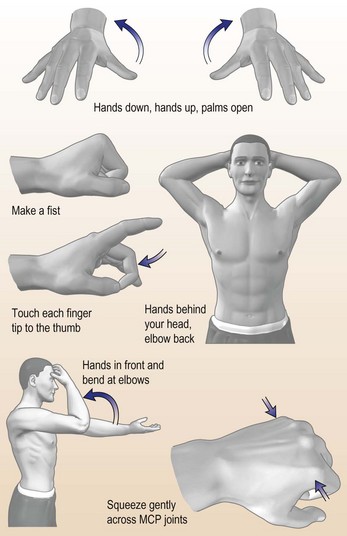
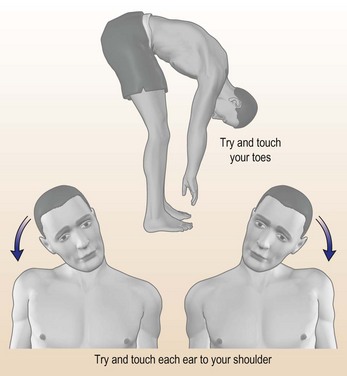
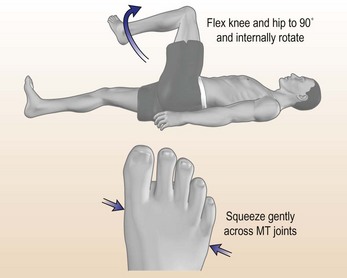
A full musculoskeletal examination is needed. The GALS (Gait, Arms, Leg, Spine) is a useful screen (Doherty et al., 1992) (Fig. 8.2).
Diagnostic clues
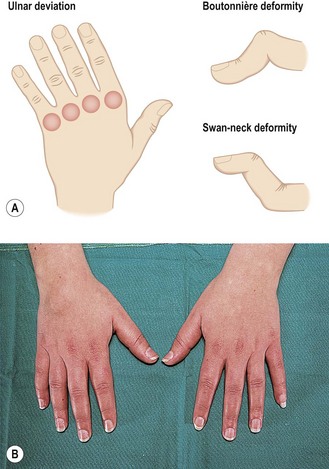
Look for Heberden’s (distal interphalangeal joints)/Bouchard’s (proximal) nodes, ‘square’ hands, painful thumb, carpometacarpal joints that indicate primary nodal OA. Figure 8.3 shows the distributions of generalised OA and pyrophosphate arthropathy.
Examine
Initial treatment
• Analgesia: simple or compound analgesia as first-line therapy, e.g. paracetamol up to 4 g/day. If this fails, a short course of an NSAID, e.g. Diclofenac usually helps the pain. There is a high risk of GI toxicity with long-term NSAID use in her age group. A gastro-cytoprotective agent, e.g. omeprazole, should be co-prescribed. Opiates should be avoided unless other analgesia has not worked because of sedation/confusion and constipation.
Later management
Refer to rheumatologist or medicine for the elderly consultant. In the meantime, organise:
There should be detailed planning before discharge, including liaison with the doctor and a home visit.
Rheumatoid arthritis (RA)
What other conditions could give a similar clinical picture?
In the first two differential diagnoses there are often other features. In SLE photosensitive rashes, hair loss, serositis and oral ulceration are seen. Erythrovirus B19 nearly always presents with flu-like symptoms and a widespread rash.
How would you manage this patient?
A full history and general medical examination is essential. Specific points:
• Look for nodules or vasculitis: uncommon at first presentation.
• A full musculoskeletal examination noting the symmetry of the joint involvement.
• Look for persistent inflammatory symmetrical arthritis (PISA). The most common cause of this is rheumatoid arthritis.
The most commonly involved joints at onset in rheumatoid arthritis are: wrists, MCPs, PIPs and MTP joints.
Admission is necessary if the patient is very unwell systemically and to exclude other pathology.
Initial management
• A short period of bed rest, ice packs if only a few joints involved.
• NSAIDS: ibuprofen is the safest; other NSAIDs have a higher risk of GI toxicity, although this patient is young.
• Disease-modifying anti-rheumatic drugs (DMARDs): these should be given at the earliest opportunity because RA is a systemic disease that leads rapidly to joint damage and disability. It is no longer acceptable to treat RA with NSAIDs alone. There is accumulating evidence to show that early DMARD use delays joint damage and functional disability.
Initial DMARDs commonly used include sulfasalazine, methotrexate or azathioprine. Others, such as IM gold and D-penicillamine, are less commonly used but still effective. Hydroxychloroquine and auranofin are the least effective but can be used in combination regimens. Combination therapies are showing good results.
SLE and vasculitis
Discuss the differential diagnosis, investigation and management
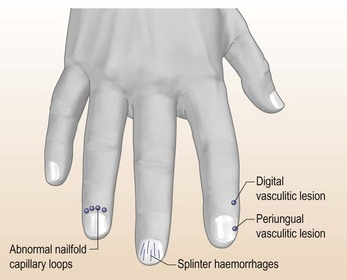
The differential diagnosis includes an inflammatory autoimmune rheumatic disease such as systemic lupus erythematosus (SLE), which has developed after delivery of her baby. The lesions on her hands (Fig. 8.6) and feet are strongly suggestive of vasculitis, which is a serious prognostic factor that requires immediate therapy.
Investigations (Table 8.1) are performed to look for the possibility of major organ involvement, which might be vasculitic. Her urine must be tested immediately for blood and protein and sent for urine cytology looking for fragmented red cells and/or casts. The presence of an ‘active’ urine sediment with fragmented or dysmorphic red cells and granular casts has a > 90% specificity for glomerulonephritis.
Table 8.1 Investigations for SLE and vasculitis
| Investigation | Typical finding |
|---|---|
| FBC | Immune cytopenias, especially neutropenia and thrombocytopenia, are common in SLE |
| There may be anaemia of chronic disease or haemolytic anaemia – check Coombs’ test. | |
| ESR and CRP | The pattern of a high ESR but normal CRP is characteristic of SLE |
| Renal function | U&E, 24-h urine protein/eGFR |
| Liver biochemistry | Hypoalbuminaemia is common |
| Lupus serology | |
| ANA | Present in 95% of SLE patients |
| dsDNA | Specific marker for SLE. A negative dsDNA, however, does not exclude SLE |
| ENA | Ro/La photosensitivity/Sjogren’s RNP/Sm often seen in severe SLE |
| Complement | Low values indicate activation of complement or rarely congenital deficiency |
| ANCA | A marker of vasculitis: a systemic vasculitis is an alternative to SLE |