205 Retinal vein thrombosis
Salient features
History
• Age: central retinal vein occlusions arise in 0·1–0·4% and branch retinal vein occlusions in 0·6–1·1% of adults aged ≥40 years
• Branched retinal vein occlusion: decreased vision, floaters suggest vitreal haemorrhage
• Central retinal vein occlusion: loss or decreased vision, headache (associated increase in intraocular pressure), floaters
• History of hypertension, diabetes, glaucoma, multiple myeloma or macroglobulinaemia.
Examination
Patient 1
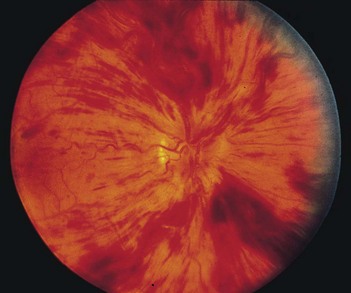
Central retinal vein occlusion (Fig. 205.1), the occlusion is behind the cribriform plate:
• Multiple retinal and preretinal haemorrhages surround the optic nerve head. there is marked dilatation and tortuosity of the veins, hyperaemia or oedema of the nerve head and soft exudates: ‘blood and thunder’ appearance
Patient 2
• Branch vein occlusion (Fig. 205.2), the occlusion is in front of the cribriform plate:
• Occlusion occurs just distal to the arteriovenous crossing and haemorrhages can be seen surrounding the occluded vein; the superior temporal vein is most commonly involved
For both patients, proceed as follows: