Respiratory Physiology
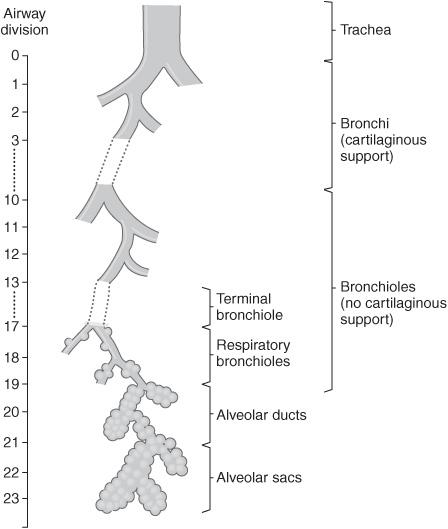
Figure 4.1 Branches of the respiratory tree. (Reproduced, with permission, from Kibble JD, Halsey CR: Medical Physiology: The Big Picture. New York, NY: McGraw-Hill; 2009.)
RESPIRATORY ANATOMY
What is the purpose of the branching pattern shown above?
To allow for dramatic increase in cross-sectional area.
What is the approximate cross-sectional area of the trachea?
2.5 cm2
How many alveoli are there present in a normal adult?
About 300 million
How many branches are there in the respiratory tree?
23
How many generations until alveoli are present; that is, how many branch generations in the conducting zone?
16 (trachea to the terminal bronchioles)
What type of epithelium lines the conducting zone?
Ciliated, pseudostratified columnar (also known as respiratory epithelium)
At what point in the respiratory tree does gas exchange begin?
Respiratory bronchioles (branch point 17)
What is the surface area of alveolar-capillary interface available for gas exchange?
50 to 100 m2; approximately the size of a tennis court
What are the barriers to gas exchange at the alveolar-capillary interface?
Surfactant
Alveolar epithelium
Interstitial space
Capillary endothelium
What types of cells compose the alveolar surface?
Type I pneumocytes: thin cells that constitute 90% of the surface area, even though less abundant than type II cells in numbers
Type II pneumocytes: most abundant, but only constitute 10% of surface, and produce surfactant
Phagocytic alveolar macrophages: ingests and clears foreign, inhaled particles
What are the two types of dead space?
- Anatomic dead space (respiratory tree with no alveoli present)
- Alveolar dead space (alveoli with no perfusion)
How is anatomic dead space approximated?
Ideal body weight in pounds is roughly equivalent to anatomic dead space in milliliters.
What is the function of anatomic dead space?
Warm and humidity inspired air Removal of foreign particles
In which locations and by what mechanisms is air filtered?
- In vibrissae (aka nasal hairs)
- By mucus in bronchi and bronchioles
- Alveolar macrophages remove particles that make it to alveoli
What is the mucociliary escalator?
As foreign particles are trapped in the mucus that lines the epithelium of the respiratory tract, the cilia on the epithelium beat upwards, away from alveoli and lower respiratory structures.
What common inhalant inhibits the mucociliary escalator?
Cigarette smoke
Why do particles in venous blood not reach the arterial circulation?
They are filtered out by the pulmonary circulation (these particles can vary, but can be clots, agglutinated red blood cells, gas bubbles, etc).
What does this “filter” prevent?
Thrombotic or occlusive events on the left side of circulation (such as stroke, MI, etc)
LUNG VOLUMES AND CAPACITIES
Define the following lung volumes:
Tidal volume (VT)
Volume of a normal breath at rest (average 500 mL)
Inspiratory reserve volume (IRV)
Additional volume of gas that can be inspired above the VT (average 3 L)
Expiratory reserve volume (ERV)
Volume of gas that can be forcefully expired after a normal passive expiration (average 1.3 L)
Residual volume (RV)
Volume of gas that remains after maximal expiration (average 1.5 L)
How are lung volumes and capacities related?
A capacity is the sum of two or more volumes
Define the following lung capacities:
Total lung capacity (TLC)
Volume of gas present after a maximal inspiration (average 6 L)
Vital capacity (VC)
Maximal volume that can be expelled after a maximal inspiration (average 4.5 L). This is the maximal volume that can be exchanged in a single breath
Functional residual capacity (FRC)
Volume remaining at the end of a normal breath at rest (average 3 L)
Identify the labeled lung volumes on the spirogram below.
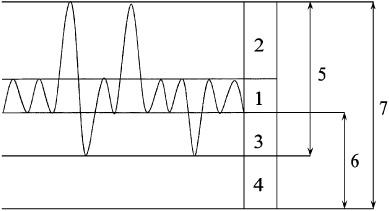
Figure 4.2 Lung volumes.
- Tidal volume (VT)
- Inspiratory reserve volume (IRV)
- Expiratory reserve volume (ERV)
- Residual volume (RV)
- Vital capacity (VC)
- Functional reserve capacity (FRC)
- Total lung capacity (TLC)
What are the volumes that make up the following capacities?
Inspiratory capacity (IC)
IC = VT + IRV
FRC
FRC = RV + ERV
VC
VC = ERV + VT + IRV
TLC
TLC = RV + ERV + VT + IRV
Which lung volumes and capacities cannot be measured using spirometry?
RV, FRC, and TLC
How can the above capacities be measured?
Nitrogen washout
Helium dilution
Body plethysmography
How does FRC change with position?
FRC increases when standing/sitting and decreases when supine
How does age affect the following parameters of pulmonary function tests (PFTs)?
TLC
Decreased
RV
Increased
VC
Decreased
FRC
Does not change
Define minute ventilation (VE):
Volume of air inspired or expired per minute:
VE = VT × frequency
What are:
Forced vital capacity (FVC)
Volume exhaled with maximal expiratory effort
Forced expiratory volume in 1 second (FEV1)
Volume that can be forcefully expired in 1 second
What is the normal ratio of FEV1 per FVC?
80% (FEV1/FVC = 0.8)
What is alveolar ventilation?
The volume of air reaching the alveoli per minute
Why is alveolar ventilation less than minute ventilation?
Last part of inspired air only reaches the conducting zone and never reaches the respiratory zone
How does shallow versus deep breathing affect alveolar ventilation?
Rapid shallow breathing produces much less alveolar ventilation; most of each breath ventilates the conducting zone
How is dead space calculated?
Vd = Vt × ([PaCO2 × PeCO2]/PaCO2)
Vd: Dead space volume
Vt: Total lung volume
PaCO2: Partial pressure of arterial CO2
PeCO2: Partial pressure of expired CO2
RESPIRATORY MECHANICS
What are the muscles of inspiration?
- Diaphragm (majority of work at rest)
- External intercostals (increase thoracic size and prevent retraction)
- Accessory muscles of inspiration (not used during quiet breathing)
What are the accessory muscles of inspiration?
Sternocleidomastoid, scalenes, strap muscles of neck
What is the innervation of the diaphragm?
Phrenic nerve (C3,4,5 keep the diaphragm alive)
Where does referred diaphragmatic pain occur?
Ipsilateral shoulder (remember the dermatomes of the nerve roots!)
Does the diaphragm contribute more to inspiration while supine or standing?
Supine; when standing, external intercostals contribute significantly
What action does the diaphragm perform?
As it contracts it flattens into the abdominal cavity, increasing the volume of the thoracic cavity
Which muscles are involved in normal, quiet expiration?
None. It is a passive process due to the elastic recoil by the lungs.
Which muscles are active in active expiration (e.g., exercise)?
Abdominal muscles and internal intercostals
During quiet breathing, which is longer, inspiration or expiration?
Expiration, in about a 2:1 ratio
Where is the intrapleural space?
It is between the lung and the chest wall. It is actually only a “potential space” under normal conditions because the visceral and parietal pleural layers are usually closely apposed.
What is the normal intrapleural pressure at rest?
Slightly subatmospheric (−3 to −5 cm H2O)
How can the intrapleural pressure be measured?
A swallowed balloon can measure the intrathoracic pressure, which approximates the intrapleural pressure.
What is the normal series of events during inspiration?
Respiration initiated by central
nervous system
↓
Diaphragm contracts, along with
other external intercostals↓Thoracic volume increases
Decrease in intrapleural pressure
↓
Alveoli expand
↓
Alveolar pressure becomes
subatmospheric
↓
Air flows into alveoli to equilibrate
with atmospheric pressure
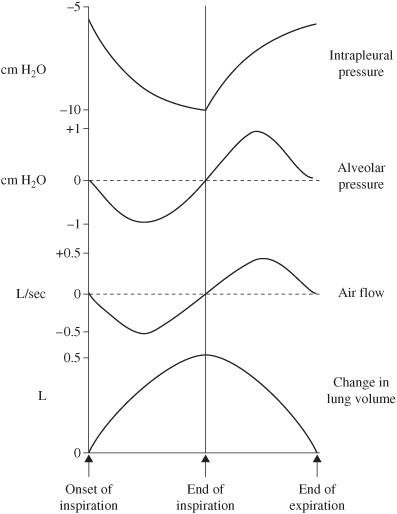
Figure 4.3 Volume, pressure, and airflow during a respiratory cycle.
Define compliance (C):
An indication of how easily the lungs and chest wall can be stretched or inflated. In general terms, it refers to the lungs ability to accommodate incoming volume.
What is the equation for compliance?
C= ΔV/ΔP
ΔV = change in volume
ΔP = change in pressure
What physiologic elements influence compliance?
Most widely discussed are things like intrinsic recoil of pulmonary tissues, but remember that lung volume and alveolar surface tension also contribute
What processes can cause a decrease in compliance?
Pulmonary congestion and various restrictive lung diseases
What causes an increase in compliance?
Destruction of lung tissue with concomitant loss of elastic tissues (e.g., emphysema)
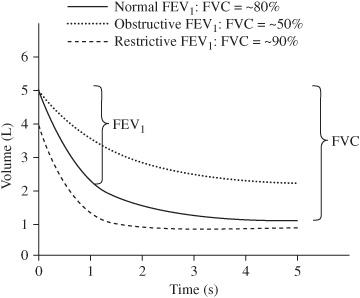
Figure 4.4 Comparison of spirograms between normal and diseased lungs.
Compare the FEV1: FVC ratio of a normal lung to a lung with emphysema or chronic bronchitis (COPD)
Normal lung has an FEV1: FVC ratio of 80%, emphysematous lung has an FEV1: FVC ratio of <80% (usually 60%-70% or less).
What other obstructive lung disease cause this pattern?
Asthma, bronchiectasis
What physical examination findings correlate with obstructive lung disease?
Increased anteroposterior diameter of the chest (barrel chested), and prolonged expiratory phase
How does the FVC compare between a normal lung and one with restrictive disease?
Total FVC is lower due to decreased lung compliance
How does compliance change with lung volumes?
Increases at low volumes, decreases at high volumes
Define elasticity:
The recoil force generated by distension of a structure
How is compliance related to elasticity?
Inversely (C= 1/E)
What contributes to the lungs’ recoil properties?
Lung parenchyma (elastin, collagen, etc)
Surface tension at air-liquid interface in alveoli
How does Laplace law relate to surface tension, and how does that affect the collapsibility of alveoli?

P = collapsing pressure (dyne/cm2)
T = surface tension (dyne/cm)
r= alveolar radius (cm)
Which is easier to keep open, a large alveoli or a small one?
Large alveoli (alveolar radius is inversely proportional to collapsing pressure, see above equation)
Which cells produce surfactant?
Type II alveolar epithelial cells
What are the functions of pulmonary surfactant?
- Reduce surface tension at low lung volumes (prevent atelectasis)
- Increase surface tension at high lung volumes (contribute to lung recoil)
- Increase alveolar radius
- Reduce pulmonary capillary infiltration
What is the effect of surfactant on compliance and elasticity?
Surfactant increases compliance, and decreases elasticity
What is surfactant composed of?
- Dipalmitoyl phosphatidylcholine (aka lecithin)-major
- Phosphatidylglycerol
- Other lipids
- Neutral lipids
- Proteins
How may surfactant synthesis be reduced?
Developmental deficiency (e.g., prematurity)
Hypovolemia
Hypothermia
Acidosis
Hypoxemia
Rare genetic disorders of surfactant synthesis
What is the significance of surfactant in infant respiratory distress syndrome (IRDS)?
In this condition a surfactant deficiency results in high surface tension in the alveoli of the lungs, leading to alveolar collapse and atelectasis. Because of this, there is decreased FRC with subsequent arterial hypoxemia.
What does the therapy for IRDS include?
- Positive end-expiratory pressure (PEEP)
- Steroids
- Exogenous surfactant
By what week do the fetal lungs make surfactant?
Week 34 to 36
What may indicate fetal pulmonary maturity?
The ratio of lecithin to sphingomyelin or L/S ratio in the amniotic fluid. Over the course of gestation, lecithin gradually increases with pulmonary maturity while the sphingomyelin remains constant, so it serves as a useful meter.
The presence of minor phospholipids (e.g., phosphatidylglycerol) is also indicative in cases where the L/S ratio is borderline.
What L/S ratio usually indicates pulmonary maturity?
2:1
What can be used to help accelerate the maturation of surfactant in the lungs of a fetus?
Glucocorticoid hormones
Under normal conditions, what structural feature of individual alveoli helps to prevent them from collapsing?
Alveolar walls and airway walls are structurally connected so that tension on alveolar walls created by one collapsing alveolus helps to hold adjacent alveoli open.
What is the above theory called?
Alveolar interdependence
What two types of resistance make up pulmonary resistance?
- Airway resistance (~80%)
- Pulmonary tissue resistance (~20%)
In what pathologic states is pulmonary tissue resistance increased?
Fibrosis from any cause, examples include amyloidosis and sarcoidosis
What factors determine airway resistance?
Gas viscosity
Diameter of the airway
Length of the airway
What law describes airway resistance?
Poiseuille law:

R = resistance
η = viscosity of inspired gas
l = length of airway
r= radius of airway
How are airway resistance and airflow related?
Much like flow through the cardiovascular system, they are inversely related:

Q = airflow (L/min)
Δ P= pressure gradient (cm H2O)
R = airway resistance (cm/H2O/L/min)
Which part of the respiratory system is the major site of airway resistance?
Medium-sized bronchi
Which part of the respiratory system has the highest individual resistance?
Small terminal airways; they are not the major site of airway resistance because they are far more numerous and are arranged in parallel
What factors can change airway resistance?
Altering the radius of the airways
Changes in lung volume
Viscosity/density of the inspired gas
What is bronchoconstriction/dilation?
Changes in the diameter of conducting airways
What causes bronchoconstriction?
Parasympathetic discharge
Substance P
Adenosine
Hypersensitivity response (e.g., histamines)
Arachidonic acid metabolites (e.g., prostaglandins and leukotrienes)
How does bronchoconstriction affect airways?
- Reduces airway radius
- Increases resistance
- Via the above two changes, limits airflow during inspiration or expiration
What causes bronchodilation?
Sympathetic discharge and sympathetic agonists via β2 receptors
How do obstructive diseases affect respiratory mechanics?
Increase airway resistance; it creates air trapping which increases lung volumes
How do restrictive diseases affect respiratory mechanics?
Decrease compliance, affecting inspiration mechanics; more on this later
GAS EXCHANGE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


