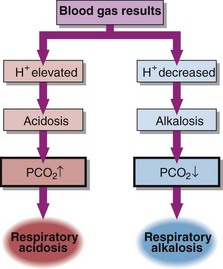
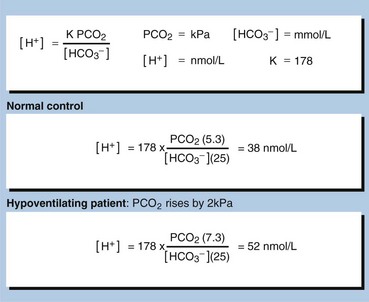
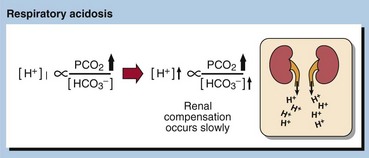
22 In respiratory acid–base disorders the primary disturbance is caused by changes in arterial blood PCO2 (Fig 22.1). Respiratory disorders are related to changes either in the amount of air moving in or moving out of the lungs (ventilation), or in the ability of gases to diffuse across the alveolar membrane (gas exchange). In both cases PCO2 changes and the carbonic acid concentration rises or falls. Respiratory acidosis may be acute or chronic. Acute conditions occur within minutes or hours. They are uncompensated. Renal compensation has no time to develop as the mechanisms that adjust bicarbonate reabsorption take 48–72 hours to become fully effective. The primary problem in acute respiratory acidosis is alveolar hypoventilation. If airflow is completely or partially reduced, the PCO2 in the blood will rise immediately and the [H+] will rise quickly (Fig 22.2). A resulting low PO2 and high PCO2 causes coma. If this is not relieved rapidly, death results. Examples of acute, and hence uncompensated, respiratory acidosis are: Chronic respiratory acidosis usually results from chronic obstructive airways disease (COAD) and is usually a long-standing condition, accompanied by maximal renal compensation. In a chronic respiratory acidosis the primary problem again is usually impaired alveolar ventilation, but renal compensation contributes markedly to the acid–base picture. Compensation may be partial or complete. The kidney increases hydrogen ion excretion and ECF bicarbonate levels rise. Blood [H+] tends back towards normal (Fig 22.3).
Respiratory and mixed acid–base disorders
Respiratory acidosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine