Reproductive Physiology
DEVELOPMENT
What determines sexual differentiation?
The composition of the sex chromosomes, either XY or XX corresponding to male and female phenotypes, respectively
What is gonadal sex?
Presence of testes in
or ovaries in
What is phenotypic or somatic sex?
Characteristics of internal/external genitalia
On a genomic level, what is it that determines sex?
The presence of the Y chromosome. It contains the SRY gene which redirects development.
What are the names of the two parallel duct systems which develop in the fetus?
- The mesonephric (wolffian) duct system
- The paramesonephric (müllerian) duct system
What cells give rise to the primitive gonad?
Primordial germ cells migrate from the yolk sac to the genital ridge
What factor determines 2 gonadal sex?
Absence of testicular differentiation factor (TDF): embryonic indifferent gonads automatically become ovaries
What three factors (or absence of factors) determine 9 phenotypic sex?
- Absence of MIF: müllerian duct develops into uterus, fallopian tubes, and upper vagina
- Estrogen: stimulates urogenital sinus and tubercle to differentiate into lower vagina, clitoris, and vulva
- Absence of TDF: embryonic indifferent gonads automatically become ovaries
What factor determines  gonadal sex?
gonadal sex?
TDF, produced by Y chromosome
What three factors determine  phenotypic sex?
phenotypic sex?
- Müllerian inhibiting factor (MIF): inhibits paramesonephric (müllerian) duct from developing into uterus and fallopian tubes
- Testosterone: stimulates mesonephric (wolffian) duct to differentiate into epididymis, seminal vesicles, and vas deferens
- Dihydrotestosterone (DHT): stimulates urogenital sinus and tubercle to differentiate into penis, urethra, prostate, and scrotum
Describe the process of male sexual differentiation.
Presence of SRY gene
↓
Leydig and Sertoli development
↓
Testosterone and müllerian inhibiting factor (MIF)
↓
Regression of the paramesonephric duct
↓
External genitalia differentiation
When during gestation do the testes descend into the scrotum?
During the last trimester; it requires the secretion of fetal gonadotropins
What condition describes the failure of testicular descent?
Cryptorchidism
What is the final stage in sexual development called?
Puberty
What endocrine event starts puberty?
Pulsatile increase in luteinizing hormone and follicle-stimulating hormone secretion
What regulatory event allows puberty to begin?
During childhood, gonodotropin-releasing hormone (GnRH) secretion is tonically suppressed. In adolescence it is secreted in a pulsatile pattern which promotes pubertal development.
Name some of the phenotypic changes that characterize puberty (more discussed later).
Pubic hair growth (pubarche), breast enlargement (thelarche), growth spurt, development of secondary sexual characteristics, etc.
MALE REPRODUCTIVE PHYSIOLOGY
Why do the testes descend into the scrotum?
To maintain temperature ~2°C below core body temperature, which is vital for normal spermatogenesis
Name the anatomic components of the testis and their associated function(s).
Seminiferous tubules (85% testis mass): spermatogenesis by Sertoli and germ cells
Rete testis: connects tubules and efferent ductules
Efferent ductules: transports sperm to epididymis by ciliary motion and contraction
Epididymis: reservoir and site of further morphologic and functional changes to sperm
Vas deferens: propels sperm into urethra by muscular contractions
What is the blood-testes barrier?
Tight junctions that protect spermatogenesis by preventing movement of immunologic proteins from circulation to the lumen of the seminiferous tubules
Why is the blood-testes barrier so important?
The process of meiosis leads to genetic reorganization and novel protein expression and production. This barrier is important in protecting the testes from autoimmune disruption.
Which cell type in the testis is the precursor to the male gamete?
Germ cells
Describe spermatogenesis.
Three general phases:
- Proliferation of spermatogonia
- Generation of genetic diversity
- Maturation of sperm
Spermatogonium (primitive germ cell)
↓
1° spermatocyte (occurs in adolescence)
↓meiotic division
2° spermatocyte
↓
Spermatid
↓ time
Spermatozoa (mature sperm)
What hormone most influences spermatogenesis?
Testosterone
What cell in the seminiferous tubule secretes testosterone?
Leydig cell
What cells primarily anchor and support the developing spermatid?
Sertoli cells (historically they were referred to as “nurse” cells)
What important hormone is secreted by Sertoli cells and increases testosterone concentrations in the seminiferous tubules?
Androgen-binding protein (ABP); this allows local concentrations of testosterone to be dramatically higher than systemic concentrations
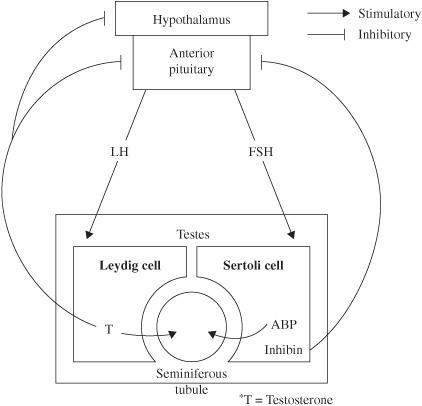
Which two anterior pituitary hormones are responsible for regulating the testosterone and ABP secretion described above?
- LH
- FSH
LH stimulates Leydig cells (Luteinizing—Leydig) to secrete testosterone; FSH stimulates Sertoli cells to secrete ABP
Describe the negative feedback that influences this endocrine cycle.
Testosterone directly feeds back to inhibit LH secretion. The Sertoli cell secretes inhibin which then exerts negative influence over the anterior pituitary.
How long does it take for spermatogonia to mature into spermatozoa?
~74 days
How is testosterone synthesized?
Cholesterol
↓ cholesterol desmolase
Pregnenolone
↓ 17 α-hydroxylase
17-hydroxy-pregnenolone
↓ 17, 20-lyase
DHEA
↓ 3 p-hydroxysteroid DH*
Androstenedione
↓↑ 21 β-hydroxylase
Testosterone
*DH = dehydrogenase
Name the actions of testosterone.
Embryonic differentiation of wolffian ducts to
reproductive tract
Puberty
secondary sexual characteristics
Contribute to Sertoli cells’ maintenance of spermatogenesis
What are the  secondary sexual characteristics influenced by testosterone?
secondary sexual characteristics influenced by testosterone?
Growth of penis, epididymis, vas deferens, and prostate
Growth spurt
Voice changes
↑ muscle mass
↑ sex drive
What factors regulate testosterone secretion?
- GnRH
- LH
- Testosterone (negative feedback)
Diagram the hypothalamus-pituitary-gonadal (HPG) axis of testosterone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



