Reproductive Pathology
EMBRYOLOGY
When is the genotype of an embryo established?
At fertilization
Define the undifferentiated stage of embryologic development:
A period when the genetically female and male embryos are phenotypically indistinguishable
When does phenotypic sexual differentiation occur?
It begins during week 7 of development and is completed by week 12 when characteristics of the external genitalia can be recognized.
What are the possible phenotypes of sexual differentiation?
Female phenotype, intersex phenotype, or male phenotype
In what sequence do the genital organs develop in utero?
Development begins with the gonads, then the genital ducts, and finally the primordia of the external genitalia.
The gonads of an embryo in the undifferentiated stage develop into what structures?
Either ovaries or testes
Development of ovaries or testes is dependent on the presence of what two hormones?
- Estrogen
- Testosterone
What gene on the short arm of the Y chromosome codes for male sex differentiation?
SRY gene
What are the two types of genital ducts found in the undifferentiated embryo?
- Paramesonephric or mullerian ducts—play a major role in female development
- Mesonephric or wolffian ducts and tubules—play a major role in male development
The urogenital systems of both males and females develop from what embryologic structure?
Urogenital ridge
What is the name of the thickening along the urogenital ridge from which the gonads develop?
Gonadal ridge
What are primordial germ cells?
Undifferentiated cells that migrate to the gonadal ridge to become either sperm or egg cells
What develops from the gonadal ridge and contains the primordial germ cells?
Primary sex cords
Development of the primary sex cords in females results in the differentiation of an outer cortex and an inner medulla. What part develops into the ovary?
Outer cortex
Primary sex cords also undergo differentiation in males. What part develops into the testes?
Inner medulla
Following primary sex cord development, secondary sex cords arise from the surface epithelium. Primordial germ cells then migrate and incorporate into these structures. In the female, secondary sex cords subsequently break up into smaller cell clusters. What are these clusters called?
Primordial follicles
What do primordial follicles contain?
Primary oocytes surrounded by a layer of simple squamous cells and connective tissue stroma
The gonads initially develop in the abdomen and then descend into the pelvis in females or into the scrotum in males. Which embryologic structure is involved in this descent?
Gubernaculum
The gubernaculum becomes what adult structures in the female?
Ovarian and round ligaments
What function do remnants of the gubernaculum serve in the adult male?
They serve to anchor the testes within the scrotum.
The paramesonephric (müllerian) ducts develop into what structures in the female?
Fallopian tube, uterus, and the upper one-third of the vagina
From which embryologic structure is the lower two-thirds of the vagina derived?
Vaginal plate
What substance suppresses development of the paramesonephric ducts in males?
Müllerian-inhibiting factor
In the female, the mesonephric ducts and tubules become part of the urinary system and eventually regress after the formation of what structure?
Metanephric kidneys
In males, the mesonephric (wolffian) duct and tubules develop into what structures?
Seminal vesicles, epididymis, ejaculatory duct, and ductus deferens
*Mesonephric ducts and tubules SEED
Some mesonephric tubules in the testes develop into what structures?
The efferent ductules of the testes
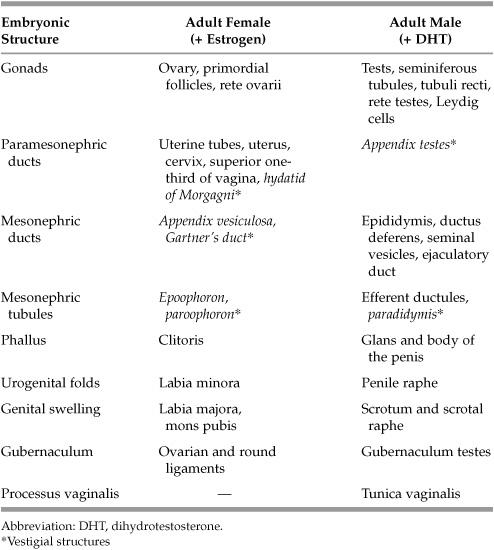
Table 10.1 Development of the Male and Female Reproductive Systems
At what stage of embryologic development does separation occur to result in dichorionic-diamniotic twins?
After day 1 to 3—each twin has its own placenta and own amniotic sac
At what stage of embryologic development does separation occur to result in monochorionic-monoamniotic twins?
After day 8 to 13—the twins have a shared placenta and a shared amniotic sac
If separation occurs between days 4 to 7, what sort of shared environment will the twins have?
These twins are likely to be monochorionic-diamniotic and will have a shared placenta but two amniotic sacs.
ANATOMY
Describe the venous drainage of the gonads:
The left ovarian or testicular vein drain to the left gonadal vein which drains to the left renal vein which drains to the inferior vena cava, whereas the right ovarian or testicular vein drains into the right gonadal vein which drains directly into the inferior vena cava.
What vessels are contained in the suspensory ligament (ie, infundibulopelvic or IP ligament) of the ovary?
Ovarian vessels
What vessels are contained in the transverse cervical (cardinal) ligament?
Uterine vessels
Where does spermatogenesis occur?
Spermatogenesis begins in the seminiferous tubules and is completed in the epididymis.
Which part of the autonomic nervous system regulates male erection?
Parasympathetic nervous system
Which part of the autonomic nervous system regulates ejaculation?
Sympathetic nervous system
* Point and Shoot
Describe the anatomic pathway followed by sperm in the process of spermatogenesis and ejaculation:
Seminiferous tubules, epididymis, vas deferens, ejaculatory ducts, urethra
HISTOLOGY
What are the histologic components of the ovary?
Germinal epithelium, cortical stroma containing theca and granulosa cells, and follicles containing germ cells
What are the two histologic compartments of the testis?
- Seminiferous tubules containing germ cells and Sertoli cells
- Interstitium containing Leydig cells
What are germ cells?
Cells in the ovary or testis which will develop into ova or sperm, respectively
What are Sertoli cells?
Sustentacular cells that nurture the developing germ cells through the various stages of spermatogenesis
Cells that are found in the interstitium adjacent to the seminiferous tubules and produce testosterone
Leydig cells produce testosterone when stimulated by what hormone?
Luteinizing hormone (LH)
What cells secrete müllerian-inhibiting factor?
Sertoli cells
In males, when do germinal cells differentiate into primary spermatocytes?
Puberty
Describe spermatogenesis:
Germ cells become primary spermatocytes under the hormonal influence of testosterone. Each primary spermatocyte undergoes a meiotic division which results in two haploid secondary spermatocytes. The secondary spermatocytes then divide again forming four spermatids. These spermatids mature into four sperm.
From which cellular structure is the acrosome of sperm derived?
Golgi apparatus
What two events must take place after ejaculation before a sperm can be fully functional and capable of fertilization?
- Capacitation
- Acrosome reaction
What is capacitation?
A series of enzymatic and biochemical events which occur while sperm are in the female genital tract prior to fertilization. The result of capacitation is that sperm are hypermotile and have destabilized plasma membranes facilitating initiation of the acrosome reaction.
What is the acrosome reaction?
A reaction that occurs when a sperm contacts the zona pellucida of an ova. During the reaction, enzymes are released from the acrosome of the sperm facilitating penetration of the outer layer of the ova and subsequent fertilization.
Formed ova within primordial follicles arrest at what stage of meiotic division?
First prophase of meiotic division
The first meiotic division is completed before ovulation takes place. The cell then continues onto a second division that is also arrested. At what stage of meiosis does this second arrest occur?
Metaphase
When is the second meiotic division of an oocyte completed?
At fertilization
During meiosis, a primary oocyte will divide into four daughter cells. Of the four daughter cells, only one will become an ovum and the rest will degenerate. What are the cells that degenerate called?
Polar bodies
During the ovulatory cycle, which hormone stimulates endometrial proliferation?
Estrogen
During the ovulatory cycle, which hormone serves to maintain the endometrium to support an implanted embryo?
Progesterone
Loss of stimulation, by which hormone leads to menstruation?
Progesterone
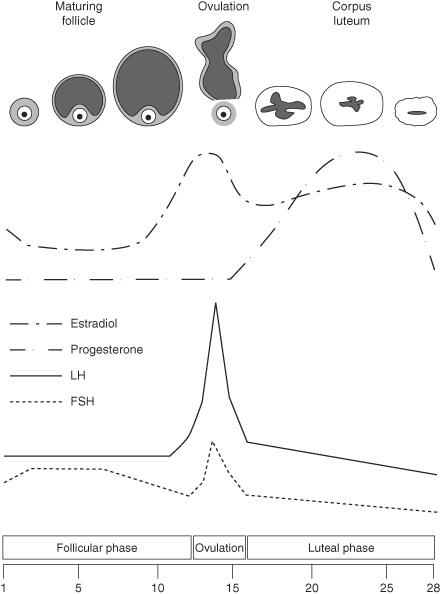
Table 10.2 The Ovulatory Cycle
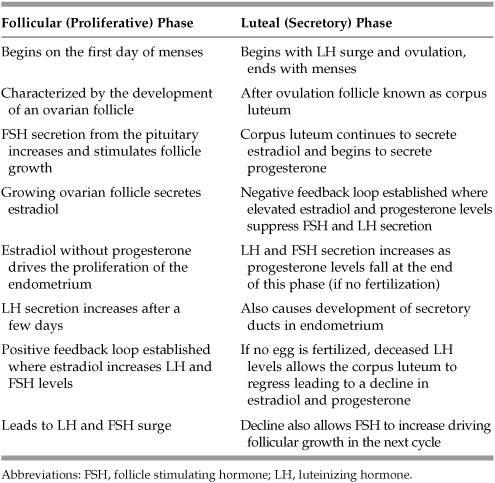
Figure 10.1 Ovulatory cycle.
What hormonal changes result in menopause?
Due to age-related decline in the number of ovarian follicles, estrogen production decreases and is eventually inadequate to stimulate ovulation and endometrial proliferation.
What are the histologic components found in breast tissue?
Glandular epithelium of the terminal duct-lobular unit, fibro-fatty stroma, and adipose tissue
PATHOLOGY
Congenital
What is a double uterus with a double vagina?
A congenital anomaly that results from the complete lack of fusion of the paramesonephric ducts and the sinovaginal bulbs
What is the defect that results in a bicornuate uterus?
The partial fusion of the paramesonephric ducts
What is a bicornuate uterus with a rudimentary horn?
A condition that develops due to the retarded growth of one of the paramesonephric ducts and results in a uterus with one normal and one abnormal horn
What defect results in the absence of the uterus or vagina?
The failure of the paramesonephric ducts and the sinovaginal bulbs to develop
What is atresia of the vagina?
A condition where the vaginal lumen is blocked due to failure of the vaginal plate to canalize and form a lumen
What is an imperf orate hymen?
A condition resulting when the vaginal plate fails to canalize resulting in vaginal outflow obstruction
What is gonadal dysgenesis?
A condition that occurs when the primordial germ cells migrate into the gonad but later degenerate resulting in hypoplastic and dysfunctional gonads
What causes gonadal dysgenesis?
Primarily chromosomal abnormalities (eg, Turner syndrome, XX gonadal dysgenesis) which result in absence of both Müllerian-inhibiting factor and testosterone
What is a hypospadia?
A congenital abnormality in males that results in the displacement of the urethral meatus
Where does a hypospadiac urethra usually open?
A hypospadiac urethra opens anywhere along the urethral groove running from the tip along the ventral aspect of the shaft to the junction of the penis and scrotum or perineum.
A congenital abnormality more commonly seen in males in which the urethra is on the dorsal surface of the penis (or results in a bifid clitoris in females). Of note, epispadias is not a type of hypospadias.
Epispadias is commonly associated with what condition?
Exstrophy of the bladder
What is phimosis and paraphimosis?
- Phimosis—constriction of the opening of the foreskin which prevents it from being pulled back over the head of the penis
- Paraphimosis—occurs when the foreskin is retracted behind the corona of the penis and cannot be returned to the unretracted position
What causes phimosis?
Congenital abnormality, inflammation, or trauma
What is a chordee?
A congenital malformation of unknown etiology that results in the downward displacement of the penis
What other congenital abnormality is associated with chordee?
Hypospadias
What is polythelia?
Also known as supernumerary nipple, polythelia is development of a nipple along the “milk line” which extends from bilateral axilla to the groin.
What is polymastia?
Also known as supernumerary breast, polymastia is development of glandular breast tissue with or without an associated nipple and also usually along the “milk line.”
Inflammation
What is a Bartholin cyst?
A fluid-filled cyst resulting from an inflammatory obstruction of the Bartholin duct
What is lichen sclerosus?
A benign, chronic inflammatory dermatosis of the vulva that results in a white, patch or plaque with epidermal atrophy
What are the clinical characteristics of lichen sclerosus?
Pruritus and leukoplakia
What are cervical polyps?
Inflammatory proliferations of the cervical mucosa not associated with malignancy
What is balanitis?
A nonspecific inflammation of the glans penis and prepuce that is caused by physical trauma, irritation, or infection
What is chemical epididymitis?
An inflammatory process resulting from the reflux of sterile urine that causes epididymal irritation
Neoplastic
What is the most common gynecologic malignancy in the United States?
Endometrial carcinoma
What is the most common malignant tumor of the vulva?
Squamous cell carcinoma
What skin malignancy may occur on the vulva?
Malignant melanoma
Though primary carcinoma of the vagina is rare, what is the most common type of neoplasm affecting the vagina?
Squamous cell carcinoma
What is vaginal adenosis?
A benign condition characterized by the overgrowth of glandular-type cells in areas normally lined by stratified squamous epithelium
Vaginal adenosis can be a precursor to what condition?
Clear cell adenocarcinoma
If a female patient tells you that she was exposed to diethylstilbestrol (DES) while in utero, what condition is she at risk of developing?
Clear cell adenocarcinoma of the vagina
What is sarcoma botryoides of the genital tract?
A rare variant of rhabdomyosarcoma that arises in the wall of the vagina, usually occurring in females under the age of 8
How does sarcoma botryoides typically present?
It presents as a polypoid mass resembling a “bunch of grapes” that projects into the vagina and may protrude from the vulva.
What is cervical dysplasia?
Disordered squamous epithelial growth marked by the loss of polarity and nuclear hyperchromasia. It is categorized as cervical intraepithelial neoplasia (CIN) 1, 2, and 3.
What is carcinoma in situ?
It is synonymous with CIN 3 and involves dysplastic changes extending through the entire thickness of the epithelium but not invading the basement membrane.
Can cervical dysplasia lead to squamous cell carcinoma of the cervix?
Yes, lower grades of dysplasia can progress to carcinoma in situ (CIS/CIN3) and all have the potential to progress to invasive cancer.
What are the most common types of cervical cancer?
Squamous cell cancer (arising from the ectocervix) and adenocarcinoma (arising from the endocervix)
What are the epidemiologic risk factors for cervical cancer?
Early sexual activity; multiple sexual partners; lower socioeconomic status; cigarette smoking
Which human papillomavirus (HPV) subtypes are most frequently associated with squamous cell carcinoma of the cervix?
HPV types 16,18, 31, and 33
HPV DNA sequences are often integrated into the genome of dysplastic or malignant cervical epithelial cells. What is the molecular mechanism associated with this process?
HPV viral proteins E6 and E7 bind and inactivate the gene products of p53 and Rb, both tumor suppressor genes, thus allowing the cells to accumulate DNA damage.
What causes endometrial hyperplasia?
Excess estrogen stimulation caused by anovulatory cycles, polycystic ovarian syndrome (PCOS), estrogen-secreting ovarian tumors, and estrogen replacement therapy
Why is endometrial hyperplasia concerning?
Although not considered premalignant, hyperplasia is believed to put a woman at higher risk of developing endometrial carcinoma.
What are the conditions that predispose a woman to endometrial carcinoma?
Nulliparity; older age; prolonged estrogen stimulation; systemic conditions such as obesity, diabetes, and hypertension
Why is obesity associated with endometrial cancer?
Estrogens can be synthesized in peripheral adipose tissue creating an environment of prolonged estrogen stimulation.
What is the most common of all tumor types in females?
Uterine leiomyoma
What is a leiomyoma?
A benign smooth muscle tumor commonly arising in the uterine wall
Leiomyomas are usually estrogen-sensitive. Would you expect tumor size to vary throughout a women’s lifetime?
Yes, tumor size would be expected to increase during pregnancy and decrease during menopause.
What is the most common complaint of women with leiomyomas?
Menorrhagia
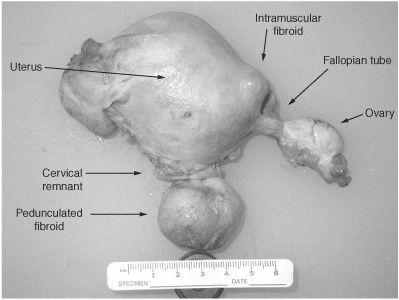
Figure 10.2 Supracervical hysterectomy specimen containing multiple fibroids. Two fibroids are visible—the first near the fallopian tube. The second is a pedun-culated fibroid which is attached via a stalk to the left cornu of the uterus but passed through the cervical os and was located in the superior portion of the vagina at the time of resection. (Reproduced, with permission, from OHSU.)
Do leiomyomas commonly transform into malignant neoplasms (leiomyosarcomas)?
No, leiomyosarcomas typically arise de novo and are thought to only very rarely result from malignant transformation.
Describe the gross morphologic characteristics of a leiomyosarcoma:
A bulky mass arising in the uterine wall possibly associated with visible areas of necrosis and hemorrhage
What are two most common tumors that arise in the fallopian tubes?
- Adenomatoid tumor (benign)
- Adenocarcinoma
Ovarian tumors are classified into various categories based on what feature determined by the World Health Organization (WHO)?
Cell of tumor origin—epithelial, sex cord-stromal, germ cell
Tumors of surface epithelial origin of the ovary include what types of tumors?
Serous tumors; mucinous tumors; endometrioid tumors; clear cell tumors; Brenner tumors
What is a serous cystadenoma?
A benign cystic tumor lined with fallopian tube-like epithelium (single layer of tall, columnar, ciliated cells) that are frequently bilateral
What is a serous cystadenocarcinoma?
An aggressive, epithelium-lined cystic neoplasm filled with serous fluid that accounts for approximately 50% of all ovarian carcinomas (frequently bilateral)
What is a mucinous cystadenoma?
A benign tumor characterized by multilocular cysts lined by mucus-secreting epithelium
What is a mucinous cystadenocarcinoma?
Malignant tumors that can cause intraperitoneal accumulation of mucinous material (pseudomyxoma peritonei)
What is a Brenner tumor?
A tumor of urothelial-like ovarian surface epithelium
Tumors of germ cell origin typically occur in what age group?
Women younger than 20 years of age
What is a dysgerminoma?
The most common malignant germ cell ovarian neoplasm
A dysgerminoma is homologous to what testicular germ cell tumor?
Testicular seminoma
Yolk sac (endodermal sinus) tumors of the ovaries are homologous to yolk sac tumors of the testes. What tumor marker is typically found in serum?
Alpha-fetoprotein (AFP)
Ovarian choriocarcinoma is a highly malignant tumor that is associated with what tumor marker?
Human chorionic gonadotropin (hCG)—primary ovarian choriocarcinoma is extremely rare, while metastatic choriocarcinoma to the ovary from a uterine primary is more common
What is a teratoma?
A tumor that exhibits evidence of simultaneous differentiation from all three germ layers—endodermal, mesodermal, and ectodermal lines. These elements may be mature or immature.
What tissue types are commonly encountered in teratomas?
Hair, teeth, bone, cartilage, skin, brain, gut, and thyroid
What is the difference in histologic appearance and clinical behavior between immature and mature teratomas?
- Immature teratomas are usually composed of primitive small round blue cells and neural tube-like structures, while mature teratomas generally resemble the normal derivates that they are emulating (skin, hair, thyroid, etc).
- Immature teratomas are typically malignant, while mature teratomas (dermoid cysts) are benign.
What is a struma ovarii tumor?
A teratoma containing thyroid tissue as the predominant tissue type
Tumors of ovarian sex cord-stromal origin include what tumors?
Thecoma-fibroma group tumors, granulosa cell tumors, and Sertoli-Leydig cell tumors
What is a fibroma?
A solid tumor consisting of bundles of spindle-shaped fibroblasts
What is Meigs syndrome?
A syndrome characterized by the triad of ovarian fibroma, ascites, and pleural effusion
What are thecomas?
Solid tumors of spindle-shaped fibroblasts with round, lipid-containing cells
What are granulosa cell tumors?
Estrogen-secreting tumors that often cause precocious puberty in children and are associated with endometrial hyperplasia/carcinoma in adults
What is pathognomonic of granulosa cell tumors?
Call-Exner bodies
What are Call-Exner bodies?
Small spaces filled with eosinophilic fluid and basement membrane material between granulosa cells in both maturing ovarian follicles and ovarian tumors of granulosa cell origin
What are Sertoli-Leydig cell tumors?
Androgen-secreting tumors associated with masculinization
Where are the primary tumors that metastasize to the ovaries usually located?
Gastrointestinal tract, breast, and endometrium
What are Krukenberg tumors?
Ovarian masses caused by metastatic mucin-secreting adenocarcinoma (usually from gastric, pancreatobiliary, or colonic primaries)
What is fibrocystic change (aka f ibrocystic disease) of the breast?
The most common disorder of the breast characterized by multifocal fibrosis and cyst formation. It is a painful condition common to patients between the ages of 25 and 50 years.
What are the two histologic types of fibrocystic disease and what are the associated features?
- Proliferative—associated with adenosis (increased size of breast lobules) and hyperplasia
- Nonproliferative—associated with fluid-filled cysts, with or without fibrosis
Is fibrocystic disease a premalignant condition?
No—generally, it is considered non-malignant and believed to not indicate increased risk of breast carcinoma.
What is a fibroadenoma?
A benign breast tumor of the intralobular stroma that presents as a firm, rubbery, painless, well-circumscribed mass
What is a phyllodes tumor?
A large, bulky tumor with usually benign behavior, although it can have malignant potential, that arises from intralobular connective tissue of the breast
What is the typical presentation of a papilloma of the breast?
It presents with serous or bloody discharge and a palpable mass.
What is an intraductal papilloma?
A benign proliferation of epithelial and myoepithelial cells on fibrovascular stalks arising in large or small lactiferous ducts
Where do most breast masses occur?
Upper outer quadrant of the breast
Who typically gets breast cancer?
Mostly postmenopausal women and women predisposed by age, positive family history, personal history of breast cancer, early menarche or late menopause, obesity, nulliparity, first pregnancy after age 30, and high animal fat diet
Briefly describe the various histologic types of breast cancer:
- Invasive ductal carcinoma—firm, fibrous, infiltrating mass, likely preceded by ductal carcinoma in-situ
- Invasive lobular—multiple foci and may be bilateral, likely preceded by lobular carcinoma in-situ
- Medullary—fleshy, cellular with lymphocytic infiltrate (good prognosis)
- Mucinous (Colloid) – gelatinous, pools of mucin surrounding tumor cells (good prognosis)
- Inflammatory—lymphatic involvement of carcinoma (poor prognosis)
- Paget disease of the breast—eczematous patches on nipples or areola; represents spread of underlying ductal carcinoma through the breast ducts to the skin of the nipple
Where can breast cancer metastasize to?
Anywhere in the body, but especially the axillary lymph nodes, lung, liver, brain, and bone
What oncogene abnormality is found in some patients with breast cancer?
Amplification of c-erbV2 (HER-2/neu)
What are the general treatments available to women with breast cancer?
Surgery (breast-conserving vs mastectomy), radiotherapy, chemotherapy, hormone therapy, and pain management
Hormone therapy is a form of systemic treatment that can be combined with surgery or radiotherapy to destroy undetected cancer cells and cells outside the breast. What are examples of this therapy?
Antiestrogens (tamoxifen), ovarian treatments (ovarian ablation), and aromatase inhibitors
What is extramammary Paget disease?
It is a neoplastic condition clinically similar to Paget disease of the breast characterized by inflammatory, eczema-like changes affecting the epidermis of the genital or perianal skin and other nonbreast cutaneous sites.
What is the origin of the neoplastic cells in extramammary Paget disease?
While this is still debated and somewhat controversial, most cases likely arise de novo from the epidermis or within an adnexal structure, either from apocrine gland ducts or keratinocyte stem cells. This is in comparison to mammary Paget disease, where the large majority of cases clearly arise from underlying breast carcinoma.
What is Bowen disease?
A preinvasive form of squamous cell carcinoma that presents as a single erythematous plaque on the shaft of the penis or scrotum
What patient population is frequently affected by Bowen disease?
Uncircumcised men older than 50 years
What are some postulated causes of Bowen disease?
Arsenic ingestion and HPV infection
What is the most frequent cancer affecting the glans penis?
Squamous cell carcinoma
Squamous cell carcinoma is characterized by slow growth and local metastasis. What are the regional lymph nodes typically affected?
Inguinal and iliac lymph nodes
As in cervical carcinoma, squamous cell carcinoma of the penis is associated with what HPV serotypes?
HPV types 16,18, 31, and 33
What are the two major groups of testicular tumors?
- Germ cell tumors
- Nongerm cell tumors
What are the important risk factors associated with testicular tumors?
- Cryptorchidism
- Genetic factors
- Testicular dysgenesis
What is a seminoma?
The most frequently occurring germ cell tumor that presents as painless enlargement of the testis
Testicular seminoma has a peak incidence in males of what age group?
30 to 40 years
What tumor marker can be found in the serum of patients with testicular seminoma?
hCG
A patient newly diagnosed with seminoma asks you about treatment and prognosis. What do you tell him?
Though malignant, seminomas are very radiosensitive and can often be cured.
What is an embryonal carcinoma?
An aggressive germ cell tumor that is characterized by rapid and bulky growth, and often presents with pain and metastasis
Embryonal carcinoma has a peak incidence in males of what age group?
20 to 30 years
What tumor markers can be found in the serum of patients with embryonal carcinoma?
hCG and AFP (only if concomitant yolk sac differentiation occurs)
What is a yolk sac (endodermal sinus) tumor?
A malignant germ cell tumor that accounts for over 80% of the testicular germ cell tumors in children. It is composed of primitive germ cells that form glomeruloid or embryonal-like structures.
What tumor marker can be found in the serum of patients with yolk sac tumors?
AFP
What is a testicular choriocarcinoma?
A highly malignant neoplasm composed of both cytotrophoblastic and syncytiotrophoblastic elements that is often encountered as a component of mixed germ cell tumors
Choriocarcinoma has a peak incidence in males of what age group?
20 to 30 years
What tumor marker can be found in the serum of patients with choriocarcinoma?
hCG
Unlike other germ cell tumors, how do choriocarcinomas metastasize?
Hematogenously
How does the treatment and prognosis of testicular choriocarcinoma differ from other types of germ cell tumors?
Tumors respond poorly to radiation and chemotherapy. Surgery is usually limited to radical orchiectomy for tissue diagnosis; mortality is very high.
What are mixed germ cell tumors?
Tumors that consist of varying combinations of germ cell tumor types. Testicular germ cell tumors are usually mixed and composed of various tumor types, including seminoma, yolk sac, embryonal, choriocarcinoma, and teratoma.
Mixed germ cell tumors have variable prognosis. What feature usually dictates prognosis?
The least mature element making up the mixed germ cell tumor
What are the available treatments for most germ cell tumors?
Treatment usually includes radiation and chemotherapy, depending on the histologic type of the neoplasm. In particular, chemotherapy has dramatically improved the prognosis of nonseminomatous germ cell tumors.
What are the two types of nongerm cell testicular tumors?
- Leydig cell tumors
- Sertoli cell tumors
What is a Leydig cell tumor?
A nongerm cell tumor derived from testicular stroma (interstitium) which may elaborate androgens and other steroids
How do patients with Leydig cell tumors typically present?
They usually present with a testicular mass and changes secondary to hormonal abnormalities.
What conditions are Leydig tumors typically associated with?
Precocious puberty in children and gynecomastia in adults
What is a key histologic feature of Leydig cell tumors?
Intracytoplasmic Reinke crystals
What is a Sertoli cell tumor?
A nongerm cell tumor composed of Sertoli cells or a mixture of Sertoli and granulosa cells
Do Sertoli cell tumors secrete any hormones?
They secrete both androgens and estrogens, but rarely in sufficient quantities to produce feminization or precocious puberty.
What is the difference in clinical behavior between mature teratomas in males compared to females?
Mature teratomas in females are benign, but in males they are most often associated with mixed immature elements such as yolk sac and embryonal carcinoma, therefore conferring a worse prognosis.
What is testicular lymphoma?
The most common testicular neoplasm in patients over age 60. Most are diffuse, large cell, non-Hodgkin lymphomas, and disseminate widely with poor outcomes.
What is the most common form of cancer in men?
Carcinoma of the prostate
What tumor marker is associated with prostate cancer?
Serum prostate-specific antigen (PSA)
What zone of the prostate is most frequently involved in prostate cancer?
Peripheral zone
Where does prostate cancer metastasize?
It frequently metastasizes to bone causing osteoblastic lesions.
What laboratory test would be an indicator of osteoblastic lesions?
Elevations in serum alkaline phosphatase
How is prostate cancer treated?
Localized disease may be treated with surgery and/or radiotherapy. Hormonal treatment with orchiectomy or administration of estrogens is generally reserved for patients with advanced disease.
Infectious
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree