Renal Pathology
EMBRYOLOGY
What embryologic structure gives rise to the urinary system?
The nephrogenic cord
What structure gives rise to the nephrogenic cord?
The urogenital ridge
What three sets of nephric structures does the nephrogenic cord develop into?
- Pronephros
- Mesonephros
- Metanephros
Which of the above structures is nonfunctional and regresses completely by week 5 of gestation?
The pronephros
The mesonephros differentiates within the nephrogenic cord to form what two structures?
- Mesonephric tubules
- Mesonephric duct (Wolffian duct)
What nephric structure develops into the definitive adult kidney?
The metanephros
When does the metanephros become functional?
At week 10 of development
What undergoes repeated divisions to form the ureters, renal pelvis, major and minor calyces, and collecting ducts?
The ureteric bud
Where is the fetal metanephros located?
In the sacral region
The kidneys ascend from the sacral region in fetal life to vertebral levels T12-L3 in the adult. This upward migration is accompanied by what other event?
The medial rotation of the kidneys by 90°
What is unique about the blood supply to the kidneys?
It varies as the kidneys ascend to their adult position. At approximately the L2 vertebral level, the definitive renal arteries will develop.
What are the arteries formed during ascent called?
Supernumerary arteries
The urinary bladder develops from what structure?
The upper end of the urogenital sinus which is continuous with the allantois
What does the allantois become in the adult human?
The median umbilical ligament (urachus)
What nephric structure becomes incorporated into the posterior wall of the bladder at the trigone?
The mesonephric ducts
An urachal cyst is a remnant of what structure?
The allantois (which later become the urachus)
What forms the female urethra?
The lower end of the urogenital sinus
The transitional epithelium and stratified squamous epithelium lining the female urethra are derived from what embryonic layer?
The endoderm
What are the three parts of the male urethra that are derived from endoderm?
- The prostatic urethra
- The membranous urethra
- The proximal part of the penile urethra
Endodermal outgrowths from what part of the male urethra develop into the prostate gland?
Prostatic urethra
Endodermal outgrowths from what part of the male urethra develop into the bulbourethral glands (Cowper glands)?
Membranous urethra
Endodermal outgrowths from what part of the male urethra develop into Littre glands?
Proximal part of the penile urethra
The distal part of the penile urethra is derived from what ectodermal structure?
The glandular plate
The glandular plate joins the penile urethra and becomes canalized to form what structure?
The navicular fossa
Ectodermal septa lateral to the navicular fossa become canalized themselves to form what structure?
The foreskin
HISTOLOGY
The metanephric vesicles differentiate into various structures that together form a nephron. What are the structures?
- Glomerulus
- Bowman capsule
- Proximal convoluted tubule
- Loop of Henle
- Distal convoluted tubule
- Connecting duct
What are the four histologic “compartments” of the kidney?
- Glomeruli
- Tubules
- Interstitium
- Vessels
What type of tissue lines the ureter, pelvis, major calyx, and minor calyx?
Transitional epithelium
What type of tissue lines the collecting ducts?
Simple cuboidal epithelium
What type of tissue lines the urinary bladder?
Transitional epithelium
RENAL PATHOPHYSIOLOGY
General Principles
What is renal failure (end-stage nephropathy)?
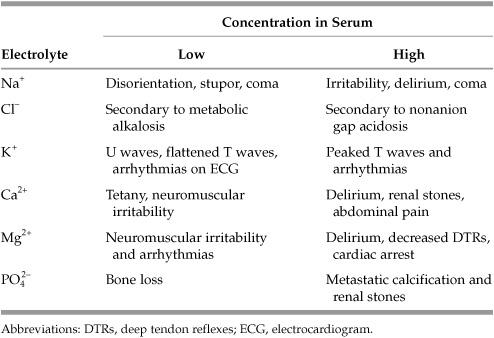
The inability of the kidneys to excrete wastes and maintain electrolyte balance. It can be broadly divided into acute and chronic renal failure. See Table 9.1 for manifestations of electrolyte abnormalities.
What are the common causes of renal failure?
- Acute tubular necrosis (ATN)
- Severe glomerular disease like rapidly progressive glomerular nephritis (RPGN)
- Diffuse renal vessel disease like polyarteritis nodosa and malignant hypertension
- Acute papillary necrosis associated with acute pyelonephritis
- Acute drug-induced interstitial nephritis
- Diffuse cortical necrosis
What happens in advanced cases of renal failure?
Patients develop uremia which is a clinical syndrome characterized by the buildup of waste products in the blood due to the inability of the kidneys to excrete them.
What are the indications for dialysis in acute renal failure?
- Hyperkalemia
- Central fluid overload
- Metabolic acidosis
- Severe hyperphosphatemia
- Severe uremia
What is the definitive treatment of hyperkalemia?
Treatment includes administration of a loop diuretic, administration of Kayexalate (cationic-exchange resin), or emergency dialysis. Glucose, insulin, and bicarbonate can be used as temporizing measures moving potassium into cells (cellular shifts) but do NOT actually decrease total body potassium.
What are the major clinical characteristics of uremia?
Azotemia is caused by abnormally high concentrations of urea and other nitrogenous substances in the blood and can lead to:
- Acidosis from the accumulation of sulfates, phosphates, and organic acids
- Hyperkalemia
- Abnormal control of fluid volume
- Hypocalcemia leading to renal osteodystrophy
- Anemia caused by decreased erythropoietin
- Hypertension due to increased rennin
What are other common clinical manifestations of uremia?
Anorexia, nausea, and vomiting; neurologic manifestations ranging from diminished mental function to convulsions and coma; bleeding from disordered platelet function; accumulation of urochrome and other urinary pigments in the skin; fibrinous pericarditis
What are the nonrenal causes of acute renal failure?
- Prerenal azotemia which can result from decreased renal blood flow caused by blood loss, decreased cardiac output, systemic hypovolemia, or septic shock
- Postrenal azotemia which can result from bilateral obstruction of urinary flow
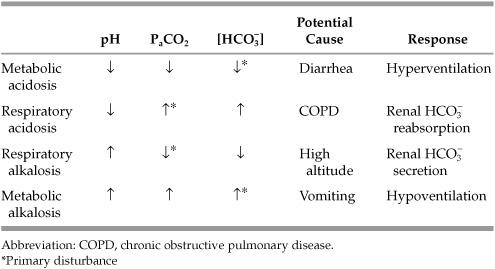
What is the step-wise approach to diagnosing acid-base disorders?
- Is the patient acidemic or alkalemic?
- Is the primary disturbance respiratory or metabolic?
- For a respiratory disturbance, is it acute or chronic?
- For metabolic acidosis, is an anion gap present?
- If an anion gap is present, are there still other coexistent metabolic disturbances?
- What is the degree of compensation by the respiratory system for a metabolic disturbance?
How do you determine whether an acute primary disturbance is respiratory or metabolic?
A respiratory disturbance will alter the arterial PaCO2 level (normal 40), while a metabolic disturbance will alter the serum HCO3− level (normal 24).
What causes anion gap acidosis?
Methanol; Uremia; Diabetic ketoacidosis; Paraldehyde or phenformin; Iron tablets or isoniazid (INH); Lactic acidosis; Ethylene glycol; Salicylates
*MUD PILES
What causes nonanion gap acidosis?
Hyperalimentation; adrenal insufficiency; uteroenteric fistula; pancreaticoduodenal fistula; diarrhea; glue sniffing; renal tubular acidosis; hyperchloremia
What causes metabolic alkalosis?
This can result from volume contraction, hypokalemia, alkali ingestion, excess glucocorticoids/mineralocorticoids, or Bartter syndrome. All of these conditions elevate serum bicarbonate levels.
What causes respiratory acidosis (accumulation of CO2)?
Central nervous system (CNS) depression; pleural disease; lung disease—chronic obstructive pulmonary disease (COPD), pneumonia; musculoskeletal disease—kyphoscoliosis, Guillain-Barre, polio
What causes respiratory alkalosis (excess elimination of CO2)?
CNS hemorrhage; drugs; pregnancy; decreased lung compliance—interstitial lung disease; liver cirrhosis; anxiety
Table 9.2 Acid-Base Physiology
What is renal tubular acidosis (RTA)?
A disease that occurs when the kidneys fail to excrete acids into the urine
What is the mechanism of disease in RTA?
Impaired tubular bicarbonate absorption or hydrogen secretion that results in hypochloremic acidosis
What are the major types of RTA?
Type I (classic distal), type II (proximal), and type IV (distal)
What is type III RTA?
It is considered a variant of type I RTA with transient wasting of bicarbonate.
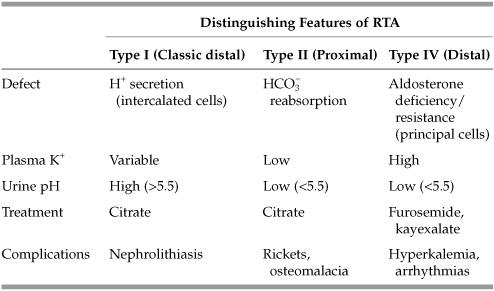
What are the most common etiologies of type I RTA?
Idiopathic, hereditary, collagen vascular disease (ie, Sjögren syndrome and SLE), cirrhosis, and nephrocalcinosis
What are the most common etiologies of type II RTA?
Hereditary, Fanconi syndrome, and carbonic anhydrase inhibitors
What are the most common etiologies of type IV RTA?
Conditions and drugs that impair the action of aldosterone—endocrine abnormalities, hypertension, DM, trimethoprim/pentamidine, nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin receptor blockers (ARB), angiotensin-converting enzyme (ACE) inhibitors, heparin, and immunosuppressive agents
Congenital
What is renal agenesis?
The failure of development of one (unilateral) or both (bilateral) kidneys
Is renal agenesis compatible with life?
Unilateral renal agenesis is compatible with life because the single kidney hypertrophies to maintain adequate function. However, bilateral renal agenesis is 100% fatal in singleton pregnancies.
What effects does bilateral renal agenesis (BRA) have on the developing fetus?
Fetal kidneys are necessary for amniotic fluid production. As such, there will be less than the normal amount of amniotic fluid present (oligohydramnios) which will subsequently impair pulmonary development.
What is the most common cause of fetal death in BRA?
Pulmonary hypoplasia—fetal urine is essential for development of lung, aiding in alveolar expansion through hydrostatic pressure and providing proline, an essential amino acid to the developing lung.
What is a Potter sequence?
A term used to describe the sequence of events that results in the typical physical appearance of a fetus that develops under conditions of oligohydramnios. Oligohydramnios may be due to several etiologies including bilateral renal agenesis.
What are some clinical features of Potter sequence?
Deformed limbs (Sirenomelia, “mermaid syndrome,” clubbed feet and/or bowed legs), redundant/wrinkly skin, abnormal facies, hypoplastic lungs
What is a pelvic kidney?
A kidney which fails to ascend to its normal position and remains in the pelvic cavity
What is a pancake kidney?
The fusion of two kidneys that are in close proximity in the pelvis due to a limited amount of space within the pelvic cavity
What is a horseshoe kidney?
A congenital anomaly that results in the fusion of the inferior poles of the kidneys forming a horseshoe shape
The normal ascent of a horseshoe kidney is arrested by what structure?
The inferior mesenteric artery
What is a common complaint in patients with ectopic ureteric orifices?
Incontinence
In males, where will an ectopic ureter drain?
The neck of the bladder or the prostatic urethra
In females, where will an ectopic ureter drain?
The neck of the bladder or the vestibule of the vagina
What is polycystic kidney disease (PKD)?
A disorder characterized by the growth of numerous fluid-filled cysts in the kidneys. These cysts slowly replace much of the renal parenchyma and result in diminished function with eventual renal failure. The disorder may be inherited in AD or AR pattern or may be the result of an acquired sporadic mutation.

Figure 9.1 Polycystic kidney disease. Numerous fluid-filled cysts replacing the majority of the renal parenchyma. Normally a kidney measures ∼12 cm in superior to inferior dimension. This kidney measures greater than 18 cm in superior to inferior dimension. (Reproduced, with permission, Wettach T, et al: Road Map Pathology, New York: McGraw-Hill, 2009; fig 10-1b.)
PKD is associated with the formation of cysts in what other organs?
Liver, pancreas, and lungs
- Autosomal dominant PKD—a common form of the disease that usually presents in midlife
- Autosomal recessive PKD—a rare form of the disease that usually presents in infancy or early childhood
- Acquired cystic kidney disease (ACKD)—an acquired form of the disease that develops in association with long-term kidney problems, dialysis, and old age
What are the common signs of PKD?
Palpable renal masses; hypertension; headaches; urinary tract infections; hematuria; cysts in the kidneys and other organs
What is the treatment of PKD?
Treatment includes dialysis and kidney transplantation.
What vascular problem is associated with the autosomal dominant form of PKD?
Berry aneurysms (often in the Circle of Willis)
What is a simple renal cyst?
An innocuous serous fluid filled cyst that is a common incidental finding with no clinical significance
What are the radiographic characteristics of a simple cyst?
Renal cysts have smooth contours, are usually avascular, and give fluid signals on ultrasonography.
A patient with end-stage renal disease who has undergone prolonged dialysis is at risk for what condition?
Dialysis-associated acquired cysts
What is nephronophthisis (uremic medullary cystic disease)?
A childhood kidney disease marked by progressive symmetrical destruction of the kidneys with cystic lesions in the medulla, involving both the tubules and glomeruli
What are the clinical signs and symptoms that characterize nephronophthisis?
Anemia, polyuria, polydipsia, isosthenuria (decreased ability to concentrate the urine), progressive renal failure, and death in early childhood
How does this differ from medullary sponge kidney?
Medullary sponge kidney is characterized by multiple small cysts in the medulla; however, renal failure is uncommon, and it is also associated with renal stones.
Inflammatory/Autoimmune
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


