Problem 11 Reflux in a 35-year-old man
A 35-year-old man presents with symptoms of epigastric bloating and heartburn. He also describes a retrosternal burning sensation, particularly at night, which may wake him from sleep. He has experienced ‘stomach’ symptoms for most of his adult life and has used over-the-counter antacids periodically with some relief. In the past few months his symptoms have become more frequent. His job has become more stressful recently, and he thinks the increased stress is related to his worsening symptoms. His symptoms have now reached a level that has made him report to his general practitioner.
He has no other past medical history and takes no regular medications. He smokes between 5 and 10 cigarettes per day and only drinks alcohol at the weekend, when he often drinks in excess of 10 pints of beer. He is overweight with a body mass index (BMI) of 32. His general examination is otherwise normal.
The patient has already tried increasing the dosage of his PPI, but to no effect.
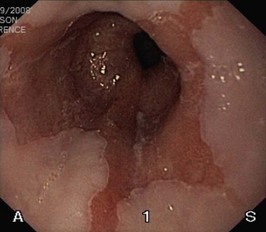
You are concerned by his anaemia and arrange for him to undergo an urgent upper GI endoscopy. (Remember, in iron deficient anaemia, if the upper GI endoscopy is normal, a colonoscopy may be indicated.) The view in Figure 11.1 shows the lower oesophagus.
Answers
A.1 Dyspepsia or reflux disease.
• Dyspepsia is a term often used for many upper gastrointestinal symptoms such as epigastric discomfort and heartburn and is poorly defined. Some pathological conditions may be found as the cause of these symptoms, but in many cases no abnormality is identified and the condition is described as functional dyspepsia.
• Reflux disease, more correctly termed gastro-oesophageal reflux disease (GORD), is the reflux of gastric contents back into the oesophagus.
Several methods have been developed to test for the presence of H. pylori.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree