Reconstruction of the Bile Duct: Anatomic Principles and Surgical Techniques
Steven M. Strasberg
The purpose of bile duct reconstruction is restoration of functional biliary–enteric continuity. The main indications are bile duct injury, elective bile duct resection, and liver transplantation. Biliary–enteric drainage from all parts of the liver is critical to well-being. Obstruction results in biliary stasis, bacterial contamination with deconjugation and precipitation of bilirubin, brown pigment stone formation, cholangitis, and eventually secondary biliary cirrhosis.
Studies of surgical anatomy and advances in surgical technique have contributed to the generally excellent results that are now possible after biliary reconstruction. The most important contributions have been the description of the variations of biliary anatomy, the understanding of the blood supply to the bile duct, development surgical techniques that expose sections of left and right hepatic ducts for anastomosis, and the use of fine suturing techniques under magnification. The key principles of bile duct repair are to perform precisely constructed mucosa-to-mucosa anastomoses, which drain all parts of the liver and which are well vascularized and tension free. With the exception of restoration of biliary–enteric continuity after liver transplantation, reconstruction usually requires hepaticojejunostomy as opposed to primary end-to-end repair of bile ducts. Choledochoduodenostomy has been used successfully in some cases of low supraduodenal biliary injuries, although it is more often appropriate for biliary
obstruction in the intrapancreatic portion of the bile duct. This chapter will focus on the indications and techniques of hepatojejunostomy with particular emphasis on management of iatrogenic biliary injuries.
obstruction in the intrapancreatic portion of the bile duct. This chapter will focus on the indications and techniques of hepatojejunostomy with particular emphasis on management of iatrogenic biliary injuries.
Definitions
The following terms are useful in describing biliary anatomy relevant to this chapter. Readers are advised to further familiarize themselves with the Brisbane 2000 Terminology of Liver Anatomy and Resections (see Suggested Readings).
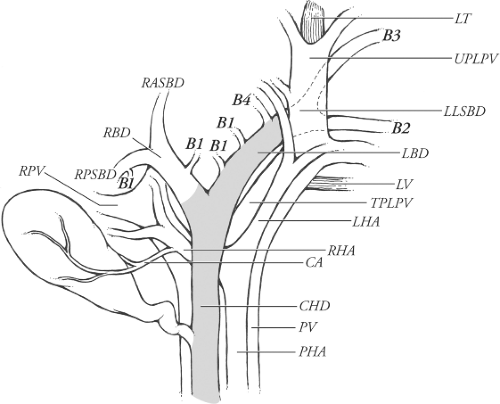
Prevailing Pattern
The prevailing pattern is the commonest anatomical arrangement. In some cases the prevailing pattern is present less than 50% of the time. For instance, the prevailing pattern of insertion of the segment 4 bile duct into the left lateral sectional bile duct to form the left bile duct (synonym: left hepatic duct) is present about 30% of the time according to Couinaud. The prevailing pattern of anatomical structures in the porta hepatis is shown in Figure 1.
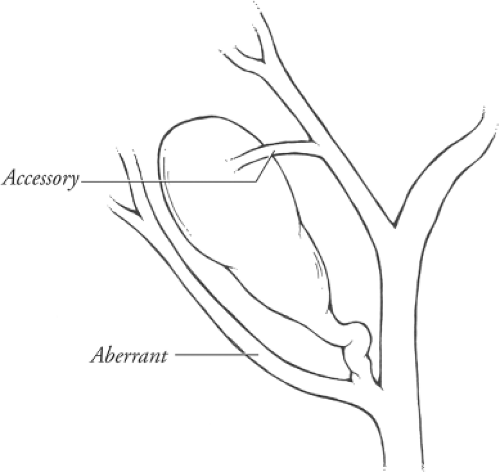
Anomaly
A deviation from the prevailing pattern. Any pattern that is other than the prevailing pattern is anomalous. Anomaly is not defined by frequency. Anomalies may be rare or approach the frequency of the prevailing pattern. Both aberrant and accessory bile ducts are anomalies because they are not present in the prevailing pattern.
Aberrant ducts are located outside the prevailing anatomical location. Some types of aberrant bile ducts are common and others are rare. Aberrant ducts are not supernumerary and their occlusion results in obstruction of bile flow from the part of the liver that they drain. Accessory bile ducts are auxiliary or supernumerary. They drain portions of the liver also drained by other bile ducts. Consequently, occlusion of an accessory duct does not obstruct bile drainage (Fig. 2). Accessory bile ducts are uncommon.
Prevailing Pattern and Important Variations of Bile Ducts Draining the Right Hemiliver
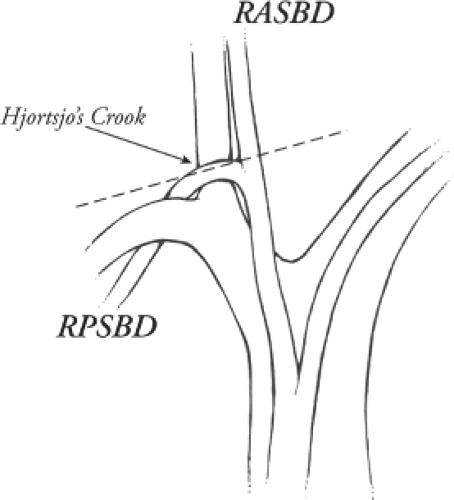
Normally only a short portion of the right bile duct, about 1 cm, is in an extrahepatic position. The prevailing pattern of bile
duct drainage from the right liver is shown in Figure 3A. The segmental ducts from Sg6 and Sg7 (called B6,B7) unite to form the right posterior sectional bile duct and the segmental ducts from Sg5 and Sg8 (B5,B8) unite to form the right anterior sectional bile duct. The sectional ducts unite to form the right bile duct, which unites with the left bile duct at the confluence to form the common hepatic duct. The right posterior sectional duct normally hooks over the origin of the right anterior sectional portal vein (Hjortsjo’s crook), where it is danger of being injured if the right anterior sectional pedicle is clamped too close to its origin (Fig. 4).
duct drainage from the right liver is shown in Figure 3A. The segmental ducts from Sg6 and Sg7 (called B6,B7) unite to form the right posterior sectional bile duct and the segmental ducts from Sg5 and Sg8 (B5,B8) unite to form the right anterior sectional bile duct. The sectional ducts unite to form the right bile duct, which unites with the left bile duct at the confluence to form the common hepatic duct. The right posterior sectional duct normally hooks over the origin of the right anterior sectional portal vein (Hjortsjo’s crook), where it is danger of being injured if the right anterior sectional pedicle is clamped too close to its origin (Fig. 4).
There are two important sets of biliary anomalies on the right side of the liver. The first involves insertion of a right sectional duct into the left bile duct. This is a common anomaly. The right posterior sectional duct inserts into the left bile duct in 20% of people (Fig. 3B), and the right anterior bile duct does so in 6% (Fig. 3C). A right sectional bile duct inserting into the left bile duct is in danger of injury during left hepatectomy. During this procedure, the left bile duct should be divided close to the umbilical fissure to avoid injury to a right sectional duct (Fig. 3B; “correct”). If the left duct is divided at its termination at the normal site of confluence of the right and left hepatic ducts, the right sectional duct may be injured and require reconstruction (Fig. 3B; “incorrect”). The second important anomaly is insertion of a right bile duct into the biliary tree at a lower level than the prevailing site of confluence (Fig. 3D). Low union may affect the main right bile duct, a sectional right duct, a segmental duct, or a subsegmental duct. The duct will unite with the common hepatic duct below the prevailing site of confluence in about 2% of people or first unite with the cystic duct and then with the common hepatic duct. The latter anomaly places the aberrant duct at great risk for injury during laparoscopic cholecystectomy.
The effect of these right-sided variations is that reconstruction of a high iatrogenic injury, which extends above the confluence (E4; see below), or reconstruction after planned resection of the confluence may require repair of both right sectional bile ducts as well as the left hepatic duct. In 25% of cases, this will be due simply to the fact that the patient has no right bile duct. The need to repair both right sectional ducts may also be due to injury or resection of the right duct, especially when it is short. The two right sectional ducts may be in close proximity, but in some cases due to low insertion of a sectional duct there may be a distance of 2 to 3 cm between the two right sectional ducts (E5; see below). The anatomical arrangement must be determined preoperatively. It cannot be assumed that drainage of one right hepatic duct will drain the entire right liver. Low insertions of right hepatic ducts may also lead to the requirement to reconstruct more than one right bile duct after resection of a hilar cholangiocarcinoma. Similarly, an aberrant right duct and the common hepatic duct may need to be constructed after pancreatoduodenectomy. The possibility of an aberrant right duct should be kept in mind when dividing tissues on the right side of the common hepatic duct at the level of the cystic duct during pancreatoduodenectomy since inadvertent injury is possible.
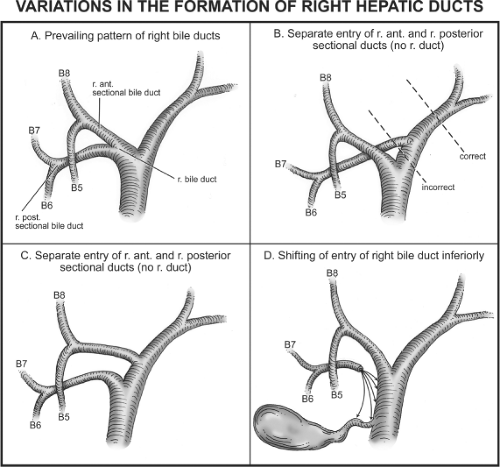 Fig. 3. (A–D) Prevailing pattern and important variations of bile ducts draining the right hemiliver. |
Prevailing Pattern and Important Variations of Bile Ducts Draining the Left Hemiliver
The left hepatic duct has a much longer extrahepatic course than the right bile duct. Normally a 2- to 3-cm length of the left hepatic bile duct is in an extrahepatic position. This portion of the left duct extends from the confluence of the right and left bile ducts along the base of Sg4, two-thirds of the way toward the umbilical fissure. This is a key anatomic feature, which makes this length of duct the prime site for high biliary–enteric anastomosis.
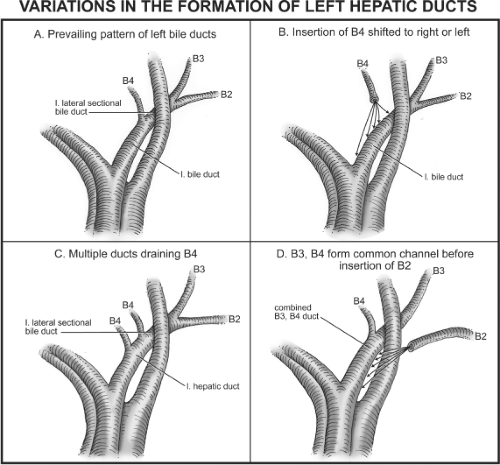
The prevailing pattern of bile duct drainage from the left liver is shown in Figure 5A
and is present in only 30% of individuals; that is, variations are present in the majority of individuals. The segmental ducts from Sg2 and Sg3 (B2,B3) unite to form the left lateral sectional bile duct. This duct passes behind the umbilical portion of the portal vein and unites with the duct from segment 4 (B4), (also called the left medial sectional duct since section and segment are synonymous for this volume of liver). The union of these ducts to form the left hepatic duct occurs about one-third of the distance between the umbilical fissure and the confluence of left and right bile ducts.
and is present in only 30% of individuals; that is, variations are present in the majority of individuals. The segmental ducts from Sg2 and Sg3 (B2,B3) unite to form the left lateral sectional bile duct. This duct passes behind the umbilical portion of the portal vein and unites with the duct from segment 4 (B4), (also called the left medial sectional duct since section and segment are synonymous for this volume of liver). The union of these ducts to form the left hepatic duct occurs about one-third of the distance between the umbilical fissure and the confluence of left and right bile ducts.
The main anomalies of the left ductal system, which are important in biliary reconstruction, involve variations in site of insertion of B4 (Fig. 5B), multiple ducts coming from B4 (Fig. 5C), and the primary union of B3 and B4 with subsequent union of B2 (Fig. 5D). B4 may join the left lateral sectional duct to the left or right of its point of union in the prevailing pattern (Fig. 5B); in the former case the insertion of B4 is at the umbilical fissure and in the latter the insertion may occur at any place to the right of the prevailing location up to the point that the left lateral sectional duct unites with the right bile duct. In the latter instance, which according to Couinaud is present in 8% of individuals, there is no left hepatic duct. Instead, there is a triple confluence of the right hepatic duct and the two ducts from the left liver (B4 and the left lateral sectional duct to form the common hepatic duct).
The left duct runs at a variable angle. In some individuals, it is almost horizontal but in others it runs sharply upward. It is much easier to expose a long length of duct in the former type. The angle of the duct is readily visible on cholangiography and will prepare the surgeon for the increased difficulty of dissection that sometimes may be present due to this factor.
The implications for reconstruction of left-sided anomalies are that the surgeon must be prepared to anastomose multiple ducts on the left, especially when performing extended bile duct resections for cholangiocarcinoma. When there is absence of the left hepatic duct, it may be necessary to repair two left hepatic ducts after a biliary injury also. The most common situation in which this is required is when the confluence of B4 and the left lateral sectional duct (B2,B3) have been resected, leaving the orifices of these ducts to be anastomosed with the intestine. When a right trisectionectomy is performed, it is not unusual to resect the confluence of B2,B3 so that these ducts require separate anastomosis. However, there are many variations and the main point is that the anatomical arrangement in a particular patient should be understood as far as possible preoperatively and that the surgeon should be prepared for the performance of multiple small anastomoses intraoperatively.
Prevailing Pattern of Bile Ducts Draining the Caudate Lobe (Sg1)
Normally two to three caudate ducts enter the biliary tree. Their orifices are usually located posteriorly on the left duct, right duct, or right posterior sectional duct. This is fortunate as they are less prone to injury. In most cases (even in E4 injuries), the caudate ducts will be included when standard reconstructions are performed. However, occasionally caudate ducts are separated from their point of insertion on the biliary tree and failure to reconstruct these ducts or resect the caudate can result in biliary fistula postoperatively. In hilar cholangiocarcinoma, resection of the caudate is usually advisable and reconstruction is not needed.
The main variations of bile duct anatomy have been described. Surgeons need to be aware that rare even unique patterns of confluence or position are possible—for instance, the right hepatic duct has been described to egress from the liver in the umbilical fissure to the left of the umbilical portion of the left portal vein!
Blood Supply of Bile Ducts
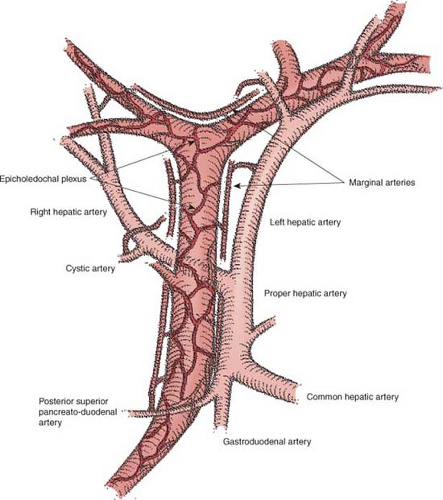
The blood supply to the ducts can be thought of a having three elements—afferent arteries, marginal arteries, and the epicholedochal plexus.
Afferent Arteries
Bile ducts are supplied only by arteries, unlike the liver. These supplying vessels are branches of the hepatic arteries or less commonly of the superior mesenteric artery or other upper abdominal arteries (Fig. 6). The posterior superior pancreatoduodenal artery supplies much of the retroduodenal and intrapancreatic common bile duct and also part of the supraduodenal common bile duct. The proper hepatic artery, cystic artery, and artery to segment 4 also commonly send afferents to the bile duct; however, the common hepatic artery itself and virtually any of its extrahepatic branches can give afferent twigs to the biliary tree. Also, aberrant arteries arising from
the superior mesenteric artery (replaced right hepatic artery) or left gastric artery (replaced left hepatic artery) can supply the bile ducts.
the superior mesenteric artery (replaced right hepatic artery) or left gastric artery (replaced left hepatic artery) can supply the bile ducts.
Marginal Arteries
The afferent vessels empty into marginal arteries, which lie upon and run parallel to the long axis of the bile ducts. They are disposed at 3 or 9 o’ clock on the common bile duct/common hepatic duct or run across the top of the confluence of the right and left bile ducts (Fig. 6). The latter marginal artery is called the “hilar marginal artery.” Infrequently there is a 12 o’ clock marginal artery. The longitudinal arteries are readily seen when the bile duct is transected, for instance, during a Whipple procedure.
Epicholedochal Plexus
The marginal arteries supply a fine arterial network that lies upon and surrounds the common bile duct, the common hepatic duct, as well as the left and right hepatic ducts, called the epicholedochal plexus (Fig. 6). The part of the network around the confluence of the right and left hepatic ducts is the hilar component of the epicholedochal plexus, and is often called the hilar plexus. The epicholedochal plexus lies between the bile duct and the hilar plate in the part of the biliary tree that lies adjacent to the plate. Therefore, while it is adjacent to the hilar plate, the plexus is not within the hilar plate in the sense of being inside the fibrous tissue of the plate. A critical point of surgical anatomy is that dissection in the plane between the hilar plate and the bile ducts has the potential to devascularize bile ducts. Therefore, when dividing a bile duct in those portions of the biliary tree next to or within the plate/sheath system, the division of the duct should be done in conjunction with division of the sheath and without dissection between duct and sheath. Branches of the epicholedochal plexus pierce the bile duct and supply it through two deeper and finer
intracholedochal plexuses in the wall of the bile duct.
intracholedochal plexuses in the wall of the bile duct.
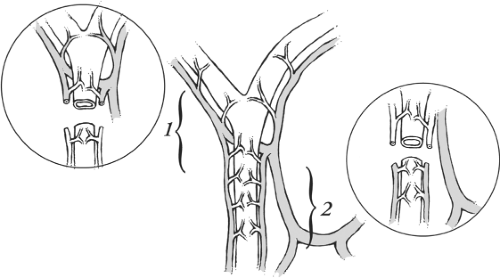
The complex system supplying the bile ducts provides redundancy. However, there appears to be a watershed of arterial blood supply on the bile duct. If the common hepatic bile duct is transected at a high level, that is, close to the confluence, the arterial blood supply to the inferior cut edge of the common hepatic duct will mainly come from the posterior superior pancreatoduodenal artery through the marginal arteries running up the supraduodenal bile duct to the level of transection—a distance of several centimeters. Consequently, ischemia of the inferior cut edge of the bile duct is possible (Fig. 7). Similarly, when the bile duct is transected at the level of the duodenum, the upper cut edge of the common bile duct may be ischemic (Fig. 7). The clinical implication is that when hepaticojejunostomy is performed the bile duct should be divided close to its upper end to ensure good blood supply, for example, 1 to 2 cm below the normal site of confluence of the left and right ducts. A corollary is that choledocho-choledochostomy is inherently somewhat risky because of the potential for one or other of the cut ends to be ischemic depending on the level of transection.
The fact that only the hepatic artery supplies the bile ducts has other implications for bile duct reconstruction. Occlusion of the hepatic artery can lead to necrosis of bile ducts without necrosis of hepatic parenchyma, which will still be supplied by the portal vein. This scenario is seen with some frequency when hepatic artery thrombosis complicates liver transplantation, but it also may occur very rarely in association with iatrogenic injuries or noniatrogenic trauma. The result may be necrosis of the intrahepatic as well as extrahepatic biliary tree, a condition that is treatable only by liver transplantation. More commonly, the problem is that an arterial injury is not appreciated when a bile duct repair is performed soon after an iatrogenic injury. This factor may result in an ischemic anastomotic stricture that appears at a later date. The potential for this problem is one reason for advocating delay of repair to give the ducts time to “die back” to a healthy level. This scenario is most commonly seen when the right hepatic artery is injured along with the common hepatic duct during laparoscopic cholecystectomy. In this vasculobiliary injury the mechanical damage occurs at the mid common hepatic duct but the associated ischemia results in evolution of the injury to a higher level, often up to the confluence of the right and left hepatic ducts. Ischemia of bile ducts may be also be induced by extensive dissection at the time of repair especially by dissections that expose the posterior surface of bile ducts and injure small arteries entering the ducts from this aspect. For this reason, we advocate anastomosis to the anterior surface rather than the terminal cut surface of bile duct when reconstructing biliary injuries, even on the right side. When the injury is very high and on the right side, this may be very difficult to achieve and ductal ischemia is a constant threat. In these circumstances, resection is sometimes an attractive alternative. With elective bile duct resections, anastomosis to the terminal end of bile ducts does not have the same problems as with repairs after iatrogenic injury; however, even in this case, bile ducts should be divided sharply and not dissected free from surrounding tissue.
Iatrogenic Biliary Injuries
These injuries, which have become more common since the introduction of laparoscopic cholecystectomy, may result in the requirement for bile duct reconstruction. Successful outcome of these often challenging cases requires exact diagnosis of the level of the injury and careful preoperative planning.
Classification and Approach to Biliary Injuries
Biliary injuries may be classified as shown in Figure 8. The Bismuth classification of biliary strictures has been used by many to classify biliary injuries. It functioned well in this role during the era of open cholecystectomy, but an expanded classification seemed appropriate after the introduction of laparoscopic cholecystectomy because certain types of injury became more common and others appeared. The current classification incorporates the Bismuth classification under types E1 to E5 and adds other injuries under headings A to D. Type A injuries are leaks at the cystic duct stump or from the gallbladder bed and will not be discussed in this chapter as they do not require reconstruction. B and C injuries are occlusions (type B) or transections (type C) of aberrant right hepatic ducts. Such ducts may drain liver volumes ranging from portions of segments to the entire right liver. These types were formerly included as subtypes of Bismuth type 5; however, as they are potentially serious injuries and are much more common since the introduction of laparoscopic cholecystectomy they require their own designation. Type B injuries (occlusion of aberrant ducts) may be silent. If so, they will result only in asymptomatic atrophy of the involved liver volume, which is compensated by hypertrophy of the normally drained liver. However, type B injuries may also present with pain or cholangitis many years after the injury has occurred. Generally, silent B injuries are not treated unless they involve a liver section or the whole right liver and are discovered before atrophy has destroyed the affected volume. Type C injuries usually require reconstruction due to persistence of biliary fistula unless the volume affected is less than a segment. In the latter case, they will often spontaneously convert to silent B injuries as the tiny duct becomes obstructed by
scarring. D injuries are partial (<50%) transections of major bile ducts. When the transection involves more than 50%, the injury should be considered an E type. When D injuries involve less than 25% of the circumference of the bile duct, they may be repaired primarily with fine absorbable sutures over a T-tube. It is preferable to bring the T-tube out of the bile duct through a separate opening in the duct so that one of the arms or the tube crosses the repair. When D injuries involve a larger circumference or have been caused by diathermy, or when the bile duct is very small, reconstruction by hepaticojejunostomy is the preferred solution. D injuries will not be discussed further.
scarring. D injuries are partial (<50%) transections of major bile ducts. When the transection involves more than 50%, the injury should be considered an E type. When D injuries involve less than 25% of the circumference of the bile duct, they may be repaired primarily with fine absorbable sutures over a T-tube. It is preferable to bring the T-tube out of the bile duct through a separate opening in the duct so that one of the arms or the tube crosses the repair. When D injuries involve a larger circumference or have been caused by diathermy, or when the bile duct is very small, reconstruction by hepaticojejunostomy is the preferred solution. D injuries will not be discussed further.
The E types are injuries of the main bile ducts that range from a low injury, >2 cm below the confluence of the right and left bile ducts (E1), to a high injury in which there is no longer communication between the left and right bile ducts (E4). E4 injuries may affect the main right or left hepatic ducts only, or involve sectional ducts or even segmental ducts depending on the level of injury and anatomical pattern of union of the bile ducts. Type E5 injury is an uncommon variant in which the common hepatic duct and an aberrant right duct are injured simultaneously. B, C, and E1 to E5 are the major biliary injuries. When describing E type injuries using this classification, one should also record whether the problem is a complete separation of the upper from the lower biliary tree or a stenosis. If a complete separation is present, then it should be noted whether transection or occlusion is present. The length of stenosis or missing duct should also be recorded.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree