Radiology & Pathology Correlation
GENERAL PRINCIPLES
What are x-rays?
Electromagnetic waves that interact with matter and are absorbed, scattered, or transmitted
How are plain radiographs produced?
By passing an x-ray beam through the patient and producing an x-ray shadow on film
What are the five basic densities on a radiograph, from least to most dense?
- Air—least dense
- Fat
- Water (blood and soft tissue)
- Bone
- Metal—most dense
How do the different densities appear on film?
Air does not absorb much radiation and appears black (radiolucent). Fat is generally gray and darker than muscle or blood. Bone and calcium appear white (radiopaque), as do metals and contrast agents, which absorb significant amounts of radiation.
Why are frontal and lateral views necessary when assessing plain radiographs?
Each view is a two-dimensional representation of a three-dimensional structure, and therefore two views are necessary to capture all three dimensions and to perform a complete evaluation.
What do the terms posteroanterior (PA) or anteroposterior (AP) indicate?
The direction in which the x-ray beam traverses the patient on its way to the film
Films taken with the patient lying directly on his or her side
Why is patient position important when evaluating a radiograph?
It can affect apparent organ size (eg, magnification of heart size), organ position, and blood flow.
What is the advantage of using contrast agents in radiography?
It allows better visualization of anatomic structures that are normally obscured by surrounding structures of similar densities.
What is computed tomography (CT)?
A diagnostic imaging method in which x-ray measurements from many angles are combined into a single image which is typically presented as a series of axial body slices
What is the relative radiation exposure per chest CT scan in comparison to a plain chest x-ray?
100 fold increase in radiation
What is the main advantage of CT over plain radiography?
CT produces higher quality and more detailed images.
Why should you NOT use intravenous (IV) contrast when doing a CT on a patient with a new head injury?
IV contrast can be confused with fresh blood in the brain.
What is ultrasonography?
A technique using high-frequency sound waves to make images
What else can be evaluated using these sound waves?
The direction and magnitude of moving blood (Doppler analysis)
What makes the technology used in ultrasonography attractive?
It does not use ionizing radiation and is relatively inexpensive.
What is nuclear imaging?
A noninvasive imaging technique that creates a picture by measuring the radiation emitted from a patient’s body after a radioactive material has been injected and allowed to distribute within the body.
What is magnetic resonance imaging (MRI)?
A diagnostic procedure that uses a combination of a large magnet, radio frequencies, and a computer to produce detailed images of the soft tissues of the body
What are the two basic types of images in magnetic resonance (MR)?
- T1-weighted images
- T2-weighted images
How does a T1-weighted image show fat and water?
Fat is seen as a bright signal (white) and water as a dark signal (black)
How does a T2-weighted image show fat and water?
Fat is seen as a dark signal (black) and water as a bright signal (white)
What are some advantages of MR?
Can produce detailed images of the central nervous system (CNS) and stationary soft tissues; does not use ionizing radiation
What are the disadvantages of MR?
Artifact is produced if the patient moves; inability to bring ferrous objects near the magnet; high cost and time intensive
What are the contraindications to having an MR scan?
Cardiac pacemakers, defibrillators, spinal cord stimulators, most aneurysm clips, and a patient’s inability to stay still (ie, children, claustrophobia)
HEAD AND NECK
What two modalities provide definitive imaging of the skull and brain?
- CT
- MRI
When is CT the procedure of choice?
When there is trauma (possible loss of bone integrity, penetrating injury, or hemorrhage) or the possibility of hemorrhagic stroke
When is imaging indicated in a patient with a headache?
Trauma, severe headache (ie, worse headache of the patient’s life), headache with neurologic findings
What does a thunderclap headache or a sudden onset of the “worst headache of one’s life” indicate?
Subarachnoid hemorrhage
What should one suspect if there is a fracture over the middle meningeal artery area?
Epidural hematoma
What are the signs of a basilar skull fracture?
Hemotympanum, periorbital ecchymoses (raccoon eye), cerebrospinal fluid rhinorrhea or otorrhea, and Battle sign
Ecchymosis over the skin of the mastoid region of the skull
What does a noncontrast CT scan show when there is acute brain hemorrhage?
An area of increased density
What additional findings can you have with an intracranial bleed?
Mass effect leading to compression of the ventricles or midline shift
What are the two types of stroke?
- Ischemic
- Hemorrhagic
Which patients tend to get hemorrhagic strokes?
Hypertensive or anticoagulated patients
What imaging technique is most appropriate for visualization of an acute hemorrhagic stroke?
A noncontrast CT scan because the fresh blood is very dense and appears white
Can the diagnosis of stroke be excluded with a normal CT scan?
No, a scan within 12 hours of the event may not yet show changes on CT.
What is the best way to visualize an ischemic stroke?
MRI. An ischemic stroke is difficult to visualize on a CT scan unless there is mass effect whereas edema due to ischemia can be identified as a bright area on MR T2-weighted images.
What is the best initial way to visualize an intracranial aneurysm?
CT-Angiography or MRI
Where do most intracranial aneurysms occur?
Anterior communicating artery
What is the imaging method of choice for most CNS neoplasms?
MRI
Are meningomas considered intracranial or extracranial tumors?
Extracranial—they arises from arachnoid cells external to the brain parenchyma.
Where is the majority of adult and pediatric primary brain tumors located, respectively?
Adult—supratentorial; pediatrics—infratentorial
On imaging, a pediatric patient has a suprasellar (supratentorial) mass with calcifications, what is the likely diagnosis?
Craniopharyngioma
What is the imaging study of choice for a patient with suspected multiple sclerosis (MS)?
An MRI of the brain and spinal cord because it will show demyelination plaques
Does the workup of vertigo involve imaging procedures?
No, unless patients do not respond to initial conservative measures
When vertigo is accompanied by sensorineural hearing loss, what type of study is suggested?
MRI of the brain
When vertigo is accompanied by conductive hearing loss, what type of study is recommended?
CT scan of the petrous bone
What is the best technique used to image intracranial infections?
MRI
What is the imaging procedure of choice for a patient with seizures?
MRI
Who requires imaging as part of a seizure workup?
Patients with new-onset seizures; epileptics with poor therapeutic response to medicines; seizure patients with new neurologic deficits
What is the initial imaging procedure of choice for a facial fracture?
Plain radiography
What is the best imaging technique for diagnosing upper airway obstruction?
Lateral soft tissue view of the neck
What is seen on lateral film when a patient presents with epiglottitis?
The affected epiglottis looks like a thumb rather than its normal curved shape (“thumb” sign)
What is seen on lateral film when a patient presents with a retropharyngeal abscess?
Prevertebral soft tissue swelling with or without air inside the tissue
What type of imaging should be done on a patient who presents with hyperthyroidism and an enlarged gland?
Radioactive iodine uptake scan, a type of nuclear medicine thyroid scan
What type of imaging should be done on a solitary thyroid nodule or a multinodular goiter?
Ultrasound with FNA (fine needle aspiration) of suspicious solid or calcified nodules
CHEST
When should an expiratory film be ordered in addition to the routine inspiratory film?
Suspected pneumothorax; suspected postobstructive atelectasis with foreign body aspiration
Is chest radiography routinely ordered for uncomplicated asthma attacks?
No, unless aspiration of foreign object needs to be excluded
What are the complications of an acute asthma attack, seen on a plain film?
Pneumomediastinum and pneumothorax
What is bronchiectasis?
Dilatation of the bronchi, either diffuse or focal, often as a result of chronic infection and subsequent cartilage damage
What is seen on chest radiograph in a patient with bronchiectasis?
Involvement of the medial aspects of both the right and left lower lobes with associated pleural thickening and honeycombing
What is seen on the chest x-ray of a patient with chronic bronchitis?
Increased or indistinct bronchovascular markings at the lung bases and bronchial wall thickening
When are chest radiographs indicated for patients with chronic obstructive pulmonary disease (COPD)?
Only with acute exacerbation, a suspected pneumonia, or history of weight loss
What is atelectasis?
Collapse of a small area of lung with resorption of air from the alveoli
What conditions cause atelectasis?
Obstructing bronchial lesion; extrinsic compression; fibrosis; loss of surface tension in the alveoli; shallow inspiration or decreased mobility
What commonly causes the collapse of an entire lung segment?
Obstruction—for example, a mucous plug, tumor, or foreign body such as malposition of an endotracheal tube
On chest x-ray (CXR), what is a consolidation and what does it represent?
An area of increased density (whiteness), that represents alveolar spaces filled with some material other than air, for example, pus, blood, fluid, or cells.
Increased visibility of a bronchus secondary to a change (increase) in the surrounding density. For example, water or edema in the lungs makes the surrounding lung more dense on CXR, highlighting the contrast between the now water-filled lung parenchyma and air-filled bronchus (an air bronchogram).
How is pneumonia diagnosed?
Correlation of signs and symptoms (clinical features) with confirmatory evidence of CXR
What does bacterial pneumonia look like on chest x-ray?
Typically, a dense consolidation that may involve patches of lung, a segment, or the entire lobe
In general, how would atypical PNA appear on CXR?
Bilateral, often diffuse ground glass consolidations
What does primary tuberculosis look like on chest x-ray?
Focal consolidation of the middle or lower lobe with lymphadenopathy and pleural effusion
What does reactivation tuberculosis look like?
Consolidation or cavitary nodule of either the posterior segment of the upper lobe or the superior segment of the lower lobe without lymphadenopathy
What are the complications of tuberculosis?
Death, miliary tuberculosis, abscess, empyema, secondary infection
What does healed tuberculosis look like on chest radiography?
Affected lung parenchyma undergoes fibrosis (especially in apices), often with areas of calcification (Ghon complex)
What does miliary tuberculosis look like on chest radiography?
A diffuse bilateral process with multiple very small nodules scattered throughout both lungs (named after the appearance of millet seeds)
What causes lung abscesses?
Necrotic pneumonias or superinfection of cavitary lesions
What is the typical appearance of a lung abscess?
A nodule or large mass with central cavitation that may have an air-fluid level and a thick wall (“rind”)
What is the differential diagnosis of a thick-walled cavitary lesion in the lung?
Either a lung abscess or a cavitating neoplasm, usually squamous cell carcinoma
What is the next step in the diagnosis of a lung abscess?
Bronchoscopy or CT-directed needle biopsy
What are Kerley B lines?
Linear opacities on chest x-ray that represent interlobular lymphatics which have been distended by fluid or tissue. They are an indication of increased pulmonary venous pressure.
What conditions are associated with Kerley B lines?
Left ventricular failure (CHF) and mitral stenosis
What are the findings of CHF on chest radiography?
Cardiomegaly, pulmonary vascular congestion and edema, Kerley B lines, and bilateral pleural effusions
What is the differential diagnosis for a solitary pulmonary nodule?
Granuloma; primary lung cancer; metastatic lesion; septic embolus; arteriovenous malformation; hamartoma; small area of atelectasis
What are the characteristics of a benign nodule?
Well-defined, round with dense central calcifications
What is the most important tool for characterizing a solitary pulmonary nodule?
Comparison of the patient’s current chest radiograph to an old chest radiograph
What lung cancers more commonly arise centrally (near the hilum)?
Squamous cell and small cell carcinomas
What are the peripherally located lung cancers?
Adenocarcinomas and large cell lung carcinoma
What is the most valuable imaging method for staging lung cancers?
CT scan
Where do lung cancers commonly metastasize?
Lymph nodes, liver, bones, brain, and adrenal glands
What does lymphoma classically look like on chest x-ray?
Large anterior mediastinal mass with hilar adenopathy
What is the most common cancer found in the lung?
Metastatic carcinoma
What is a spontaneous pneumothorax (PTX)?
An accumulation of air in the pleural space that results in lung collapse, often from rupture of an apical bleb
What is a tension pneumothorax?
A tension PTX is accumulating air in the pleural space, secondary to trauma, leading to creation of a one way valve that leads to continual increase of air in the pleural space and therefore increasing intrathoracic pressure. This results in a mediastinal shift with depression of the hemidiaphragm and displacement of the heart and trachea away from the side of the pneumothorax.
What is the negative outcome of increased intrathoracic pressure?
This is a medical emergency! The increase intrathoracic pressure decreases venous return and ultimately can lead to death.
How large does a pleural effusion need to be in order to be seen on a routine upright chest radiograph?
At least 250 mL
What is an empyema?
Pus within the pleural space usually as a result of a primary infectious process or postsurgical/posttraumatic circumstances
What are the most common etiologies of anterior mediastinal masses?
Thymoma, ectopic Thyroid, Teratomas, and Terrible lymphomas
*Four Ts
What are the most common etiologies of middle mediastinal masses?
Lymphadenopathy (lymphoma, sarcoid), duplication cysts, teratoma, fat pad, diaphragmatic hernia, extension of esophageal or bronchogenic carcinoma
What are the most common etiologies of posterior mediastinal masses?
Neurogenic tumors, including neurofibromas, schwannomas, or ganglioneuromas; other lesions include hernias, lymphadenopathy (lymphoma), aortic aneurysm, hematomas, or extramedullary hematopoiesis
On what side do most ruptures of the diaphragm occur?
On the left side because the liver usually protects the right side from damage
CARDIOVASCULAR SYSTEM
What causes cardiomegaly or an enlarged cardiac silhouette?
Valvular disease, cardiomyopathy, congenital heart disease, pericardial effusion, and mass lesions
In general, how can one differentiate between the multiple causes of cardiomegaly on plain film?
Cardiomyopathies and pericardial effusions generally lead to symmetric enlargement, whereas valvular disease and congenital heart disease often have specific chamber enlargement.
What are some causes of dilated cardiomyopathy?
Ischemia, alcohol, infections, metabolic disorders, collagen vascular disease, and toxic agents such as chemotherapeutic drugs
What does acute enlargement of the cardiac silhouette most likely represent?
Pericardial effusion
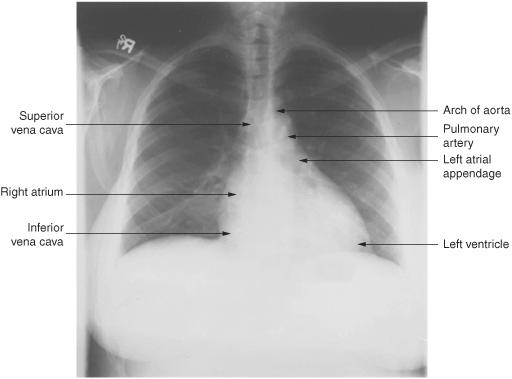
Figure 16.1 Normal CXR—Mediastinal silhouette. (Reproduced, with permission, from Tintanalli JE, Kelen GD, Stapczynski JS: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 6th ed, New York: McGraw Hill; fig 61-1.)
What does cardiac enlargement secondary to pericardial effusion look like?
The heart is pendulous and is much wider at the base giving it the appearance of a water bag.
What is the imaging procedure of choice if a pericardial effusion is suspected?
Echocardiography
What imaging studies provide the best quantitative evaluation of cardiac ejection fraction?
Nuclear medicine gated blood pool or multiple gated acquisition (MUGA) studies; echocardiography
What is the normal left ventricular ejection fraction?
65% to 75%
At what point does a patient require an angiogram?
Only if ejection fraction is less than 35% or if exercise treadmill, nuclear medicine, or echocardiography results are positive
What causes isolated left atrial enlargement?
Mitral stenosis
What is seen on a frontal chest radiograph of a patient with mitral stenosis?
Prominence of the left atrial appendage and the widening of the inferior carinal angle (greater than 75°)
What are the clinical signs of constrictive pericarditis?
These include signs of right cardiac failure such as hepatomegaly, distended neck veins, ascites, and peripheral edema.
What is the best study for constrictive pericarditis?
Echocardiogram
What are the three most common causes of pulmonary artery enlargement?
- Pulmonary stenosis
- Pulmonary hypertension
- Patent ductus arteriosus (PDA) or atrial septal defect (ASD) (due to increased flow through the pulmonary artery)
What is found on chest x-ray if a patient has tetralogy of Fallot?
Decreased pulmonary vascularity and a boot-shaped heart with an uplifted apex and a concavity along the left cardiac border
What is the differential diagnosis for cardiomegaly with an enlarged right atrium?
Ebstein anomaly/malformation, tricuspid atresia, and pulmonary atresia
Which causes of cyanotic heart disease have increased pulmonary vascularity?
All have increased vascular markings except tetralogy of Fallot.
What are the causes of acyanotic heart disease with normal pulmonary vascularity?
Aortic stenosis, pulmonary stenosis, coarctation, and interruption of the aortic arch
What should one look for in the case of acyanotic heart disease with increased pulmonary vascularity?
Left atrial enlargement and a possible PDA or VSD
How is coarctation of the aorta diagnosed?
Coarctation is suspected clinically with asymmetric pulses and/or blood pressures (classically, with hypertension in the right upper extremity, hypotension in the lower extremities, and diminished femoral and peripheral pulses). The diagnosis is confirmed with imaging, MRI, CT, or ECHO.
What is a characteristic x-ray finding of coarctation?
Notching of the inferior aspect of the ribs due to erosion by tortuous and dilated intercostal arteries that form secondary to necessary collateral flow given the restricted aortic blood flow
What are the chest x-ray findings in a patient with PE?
Most commonly there are NO findings on chest x-ray! If the PE is large enough to cause pulmonary infarction then a wedge-shaped consolidation (Hampton hump) and/or pulmonary vascular asymmetry (Westermark sign) may be apparent.
What is the most sensitive and specific study to evaluate for suspected PE?
CT angiogram (CTA) is the gold standard
What are the signs of a PE on an angiogram?
Signs include an abrupt termination of a vessel or an intraluminal filling defect
If a patient cannot tolerate a CTA (eg, in patients with renal failure) or in some subsets of patients including otherwise healthy nonsmokers or pregnant women, what other study can be obtained to evaluate for possible PE and minimize radiation exposure?
Ventilation-perfusion scan (V/Q scan)
What kind of defect does a PE cause on a V/Q scan?
A defect on the perfusion scan that is not seen on the ventilation scan (mismatched defect)
V/Q scans are of little value in what type of emboli?
Septic or fat emboli
What is the most common source of a PE?
Lower extremity DVT
What is the initial imaging test of choice for a patient with suspected DVT?
Duplex ultrasonography
What is seen on ultrasound when a DVT is suspected?
With pressure, the femoral vein usually compresses, but when there is a clot within the vein, echoes are seen within the lumen and no compression is identified.
A patient gets a nuclear medicine study to evaluate his coronary artery disease (CAD). How is a defect seen on both stress and rest images different from a defect seen only on stress images?
A defect seen on both stress and rest images likely represents a scar, whereas a defect seen only on stress images implies ischemia.
How are individual coronary arteries visualized and localized?
Coronary angiography
What does calcification of the aortic arch on chest x-ray suggest?
This clearly demonstrates that the patient has atherosclerosis, implying that they may also have underlying coronary artery disease (CAD) and/or peripheral artery disease (PAD).
What yields the most definitive evaluation of normal and anomalous aortic anatomy?
Injection of contrast material directly into the aorta (contrast angiography)
What is the most common cause of aortic tears?
Traumatic disruption secondary to motor vehicle accidents
What are the signs of a tear on an AP chest radiograph?
Increased mediastinal density and width at or above the level of the aortic arch; apical pleural density caused by blood above the left apical portion of the lung; deviation of the trachea to the right and depression of the left mainstem bronchus
What is the initial test of choice to exclude aortic injury?
CT scan
What causes aneurysms of the aortic arch and the descending thoracic aorta?
The most common cause is atherosclerosis, but they can also result from fibromuscular dysplasia and cystic medial necrosis.
What causes aneurysms of the ascending aorta?
Historically, aneurysms of the ascending aorta were due to syphilis. At present, Marfan syndrome is the more likely cause.
Separation of the layers of the wall of the aorta secondary to intimal tearing that allows for the creation of a false lumen where blood flow can occur
Which patients have an increased risk of developing an aortic dissection?
Hypertensive patients with atherosclerosis
What is a characteristic finding of aortic dissection on chest x-ray?
Dilated aorta with a widened and dense mediastinum and cardiomegaly
What other imaging technique can be used to diagnose dissection?
CT scan
What is the best way to evaluate an abdominal aortic aneurysm?
Abdominal ultrasonography
When is surgery an appropriate treatment option for patients with abdominal aortic aneurysms?
When the abdominal aortic diameter exceeds 5 cm
What is the gold standard for the evaluation of peripheral arteries?
Contrast angiography
BREAST
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


