James H. Ford II, PhD, FHIMSS, Kim A. Hoffman, PhD, and Kimberly Johnson, MBA, MSEd
31
FRAMEWORK FOR CHANGE
A series of reports from the Institute of Medicine (IOM) and the implementation of the Patient Protection and Affordable Care Act (ACA) as well as the final rules associated with the Mental Health Parity Act provide a framework for change in the field of substance abuse treatment. The IOM reports identified needs for better health care and outlined strategies to improve the quality of health care in America. These recommend that alcohol, drug, and mental health treatment systems emphasize six dimensions of quality of care: That health care should be safe, effective, patient centered, timely, efficient, and equitable. They also recommended that public agencies and payers promote the development of process and outcome measures that track quality of care. Another IOM report, Substance Use Disorders in the U.S. Armed Forces (2012), recognizes the effect of combat on veterans’ substance use and strongly recommends the full implementation of the Department of Defense evidence-based guideline for treating substance use disorders.
Mandates such as the ACA stipulate that drug and alcohol treatment services must provide evidence-based, patient-centered care delivered in ways that are safe, timely, efficient, and equitable and comply with the key components of the Mental Health Parity and Addiction Equity Act (MHPAEA). The ACA creates new incentives to reform health care and build patient-centered and robust monitoring systems. However, it is unclear whether the current system of care has the resources to meet the proposed mandates. For example, the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act requires the development of electronic medical records that are interoperable (i.e., the ability to exchange information between different electronic medical record systems) and include all patient medical care. Most treatment centers in the public setting have not yet made this investment. As the ACA is implemented, many addiction treatment programs may not be capable of providing the mandated professionally and medically oriented services. The ACA also requires that all benchmark and benchmark-equivalent state Medicaid plans comply with the MHPAEA. Under this law, insurance companies can no longer arbitrarily limit the number of hospital days or outpatient treatment sessions or assign higher co-payments or deductibles for those in need of behavioral health care services. These rule changes will eliminate barriers to the use of services for alcohol, drug, and mental health disorders and may lead to greater use of mental health and addiction treatment services.
DEFINING AND MEASURING QUALITY TREATMENT AND OUTCOMES
The use of standardized quality measures in addiction treatment has not been widely adopted in addiction treatment. In response, organizations such as the Washington Circle Group, the National Quality Forum (NQF), and the American Society of Addiction Medicine are leading efforts to develop, implement, and use standardized measures.
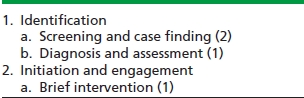
The Washington Circle Group (http://www.washingtoncircle.org/) is composed of experts in substance abuse policy, research, and performance management who are developing and testing measures that monitor the performance of health plans and public treatment systems. The group has developed and evaluated six quality measures related to substance abuse treatment that focus on treatment identification, initiation, engagement, and continuity of care. Studies indicate that in the public sector, initiation and engagement in treatment predict the likelihood of future arrests or incarcerations; treatment continuity predicts 3-month treatment recovery as measured by substance use. Studies conducted in the VA using the Washington Circle measures show mixed results.
The NQF is a congressionally chartered membership organization charged with using an empirically based consensus process to define and disseminate standards and measures for the health care system. A recent NQF report identifies 11 treatment practices, organized into four domains and subdomains, as evidence-based treatments for alcohol, tobacco, and drug use disorders (Table 31-1). Endorsement by NQF members of these practices is the first formal consensus on evidence-based practices for treatment of substance use conditions. The NQF continues to define, test, and disseminate operational measures for these sanctioned practices in the field of mental health and substance abuse care. Adoption and use of these measures is necessary in order to receive incentive payments or avoid penalties in the final rule for stage two criteria for meaningful use of electronic health record systems.
TABLE 31-1. NQF TREATMENT PRACTICE DOMAINS
In 2013, the American Society for Addiction Medicine (ASAM) convened a workgroup to identify the critical outcomes that care systems should accomplish for patients with addiction. The workgroup seeks to identify standards for addictions specialist physicians who address their role in direct patient care and improving systems outcomes. The plan is to give priority to standards that have the highest impact on quality, are feasible, and reduce costs. The workgroup will review current measures and define the domains of addiction specialist performance. Workgroup members will define the role of the addiction specialist physician in maximizing the likelihood that these outcomes are achieved. In addition, they will identify and prioritize gaps in standards and measures to form a research agenda.
ACCREDITATION FOR TREATMENT PROGRAMS
Three organizations—the Joint Commission, the Commission on Accreditation of Rehabilitation Facilities, and the Council on Accreditation for Children and Family Services—are the primary entities that provide peer-reviewed accreditation for alcohol and drug treatment programs. Accreditation is optional for treatment programs that do not dispense methadone. The Federal Drug Administration governs the accreditation of opioid treatment programs, which do dispense methadone. The FDA requires these programs to receive certification from a national accreditation organization or state agency documenting that the treatment program meets regulatory standards and will comply with the standards. The accreditation process requires a significant investment of resources; the 2010 National Survey of Substance Abuse Treatment Services survey indicates that <50% of alcohol and drug treatment programs have received accreditation.
BUILDING SYSTEM CAPACITY TO DELIVER EFFECTIVE TREATMENTS
Since 2003, behavioral health providers as well as other community-based treatment providers have been using the NIATx process improvement model to improve treatment quality. The NIATx process improvement model (www.niatx.net) integrates the work of quality improvement pioneers such as Edward Deming and Joseph Juran with five key process improvement principles that facilitate organizational changes. The principles are as follows:
1. Understand and involve customers in identifying and fixing problems.
2. Address or fix a key problem that is important to executive leadership and tied to the organizational strategic plan.
3. Identify and support a powerful change leader in the organization whose role is to lead a change team in creating and implementing organizational change.
4. Seek ideas from outside the organization or from other industries (e.g., banking or hospitality) and adapt those promising practices to your organization.
5. Use rapid plan–do–study–act (PDSA) cycles to implement and evaluate changes that are intended to improve processes of care related to the customer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


