Pulmonary Hemorrhage with Vasculitis
Pulmonary hemorrhage with vasculitis is almost always immunologically mediated. Systemic manifestations and serologic tests provide important clues to the diagnosis. Regardless of etiology, patients present with a triad of hemoptysis, anemia, and alveolar densities on chest radiographs. Diseases associated with pulmonary hemorrhage syndrome may be broadly classified into those associated with antiglomerular basement membrane antibody-associated Goodpasture syndrome, immune complex-mediated diseases with proliferative glomerulonephritis including Wegener’s granulomatosis, collagen vascular diseases, Churg-Strauss syndrome, microscopic polyarteritis, and Behçet disease. Serologic tests of patients with pulmonary hemorrhage, specifically antiglomerular basement membrane (AGBM) antibody and antineutrophil cytoplasmic antibody (ANCA), are essential for diagnosis and management. The most common histologic finding in this group of patients is necrotizing alveolitis. Pulmonary-renal syndromes involve the occurrence of both diffuse alveolar hemorrhage/pulmonary capillaritis and glomerulonephritis and include ANCA-associated vasculitides, Goodpasture syndrome, and systemic lupus erythematosis. Features that clinically suggest that a patient has vasculitis include multisystem disease, diffuse alveolar hemorrhage (the subject of this chapter), acute glomerulonephritis, pulmonary-renal syndrome, palpable purpura, and mononeuritis multiplex.
ANCA is comprised of several autoantibodies with specificity for the primary granules of neutrophil proteases, and lysosomal granules of monocytes. ANCA antibodies are divided into two groups based on their immunoflourescence staining pattern: a cytoplasmic pattern (C-ANCA) with specificity directed against proteinase-3, and P-ANCA with specificity directed against myeloperoxidase. Common systemic vasculitis syndromes with positive ANCA serology include Wegener’s granulomatosis, microscopic polyarteritis, idiopathic crescentic glomerulonephritis, Kawasaki disease, Churg-Strauss syndrome, classic polyarteritis nodosa, and Goodpasture syndrome.
Part 1 Vasculitis in Collagen Vascular Diseases
Abida K. Haque
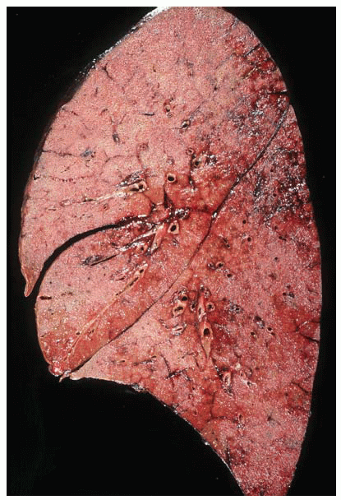
Collagen vascular diseases represent an infrequent cause of diffuse alveolar hemorrhage (DAH), with systemic lupus erythematosus (SLE) the most frequent collagen vascular disease to cause DAH. This group is heterogeneous and patients may present with multisystem manifestations, or with predominantly lung and renal disease. DAH is an uncommon complication of SLE and is fatal in about 50% of patients who experience it. Most patients
have hemoptysis, dyspnea, and fever, or may have pulmonary infiltrates on radiograph with falling hematocrit and hemorrhage in their bronchoalveolar lavage. DAH may even more rarely complicate other connective-tissue diseases such as rheumatoid arthritis or mixed connective-tissue disease.
have hemoptysis, dyspnea, and fever, or may have pulmonary infiltrates on radiograph with falling hematocrit and hemorrhage in their bronchoalveolar lavage. DAH may even more rarely complicate other connective-tissue diseases such as rheumatoid arthritis or mixed connective-tissue disease.
Histologic Features
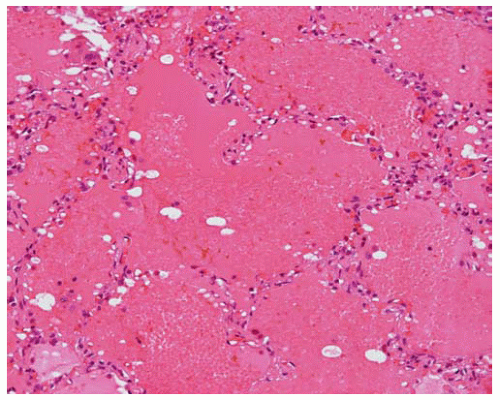
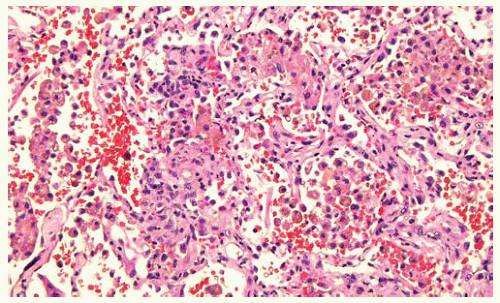
Pulmonary capillaritis with neutrophils and other leukocytes infiltrating the alveolar septa associated with intra-alveolar red blood cells, intra-alveolar hemosiderin-filled macrophages, and sometimes alveolar septal necrosis.
Only bland pulmonary hemorrhage in some cases.
Part 2 Antiglomerular Basement Membrane Antibody Disease (Goodpasture Syndrome)
Abida K. Haque
Antiglomerular basement membrane antibody disease (AGBM), or Goodpasture syndrome, is a primary immune-complex mediated vasculitis that typically presents as a pulmonary-renal syndrome affecting young adult males. The disease is characterized by the presence of pulmonary-renal syndrome and circulating antiglomerular basement membrane antibodies to the carboxy-terminal NC1 domain of the α3 chain of type IV collagen. Type IV collagen is found in basement membranes of glomeruli and alveoli, where it is accessible to the circulating antibodies. These antibodies are detected in the serum or by immunofluorescence of kidney or lung biopsies to establish the diagnosis. Treatment is by steroids and other cytotoxic immunosuppressive agents and by plasmapheresis.
Histologic Features
Alveoli filled with red blood cells, fibrin, and hemosiderin-laden macrophages.
Alveolar septa are widened and infiltrated by neutrophils (necrotizing alveolitis) in most, but not all, cases.
Vasculitis and alveolar hemorrhage subside with 1 to 2 weeks of effective therapy.
Focal septal fibrosis and, rarely, hyaline membranes may be seen.
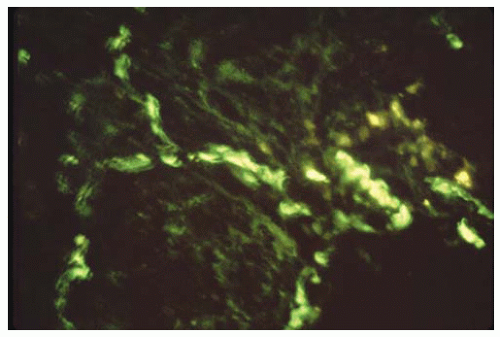
Alveolar and capillary basement membranes show linear IgG deposits with immunofluorescence.
Linear C3 deposits may be observed along alveolar basement membranes by immunofluorescence.
Part 3 Wegener’s Granulomatosis
Roberto Barrios
Keith M. Kerr
Wegener’s granulomatosis (WG) is a multisystem disorder characterized by aseptic necrotizing granulomatous inflammation and vasculitis. In its “classic,” form it affects the upper and lower respiratory tracts and the kidneys (complete form, Wegener triad). Limited forms confined to the respiratory tract have been described. Men are affected more frequently than women, with a mean age at onset of approximately 40 years. Typically in WG, chronic sinusitis or rhinitis, refractory to usual therapy, heralds the onset of the disease. The estimated sedimentation rate (ESR) is significantly increased. Autoantibodies against extranuclear cytoplasmic components of polymorphonuclear leukocytes have been detected in patients with WG. These antibodies are directed against proteinase-3 of the neutrophil cytoplasmic azurophil granules, which results in the granulated cytoplasmic staining pattern (C-ANCA). C-ANCA has been found to be both sensitive and relatively specific (although not diagnostic) for WG, particularly when the disease is in an “active” phase. Although C-ANCA is quite useful in terms of diagnosis, it may not always be reliable as an indicator of “activity.” Mild anemia may be found, but significant peripheral blood eosinophilia is absent (in contrast to Churg-Strauss syndrome, in which peripheral eosinophilia is seen).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree