Pulmonary Hemorrhage without Vasculitis
Pulmonary hemorrhage ranges from a focal procedural finding to a dramatic manifestation of underlying lung disease, and may be seen associated with or without vasculitis. In this chapter and the next, the underlying causes of pulmonary hemorrhage are discussed.
Pulmonary hemorrhage without vasculitis may be seen without any histologic abnormalities and may be incidental to biopsy procedure, etc. It may also be seen as a manifestation of infections, diffuse alveolar damage (DAD), chronic passive congestion, pulmonary vascular abnormalities such as arteriovenous malformation, and idiopathic pulmonary hemosiderosis.
Part 1 Hemorrhage without Other Histologic Abnormalities
Abida K. Haque
Acute pulmonary hemorrhage is frequently seen in biopsies as a procedural artifact of the biopsy of this highly vascular organ. Lung trauma secondary to motor vehicle accidents, diving accidents, drowning or near drowning, for example, can also produce similar histologic changes. Localized pulmonary hemorrhage may be seen adjacent to, as well as involving, neoplasms, thromboemboli, pneumonia, and airway ulceration. Coagulopathy-associated pulmonary hemorrhage can appear identical to procedure-induced hemorrhage, and in these cases, clinical history, laboratory findings, and the presence of hemosiderin-laden macrophages, provide a clue to the underlying cause of hemorrhage. Idiopathic pulmonary hemosiderosis is a rare cause of hemorrhage without other histologic abnormalities. Changes of acute lung injury, erythrophagocytosis, or hemosiderin-laden macrophages strongly suggest hemorrhage attributable to an underlying process or disease.
Histologic Features
Intra-alveolar red blood cells, with or without fibrin and white blood cells.
Alveolar septa lack inflammation, necrosis, or other abnormalities.
Absence of erythrophagocytosis or hemosiderin-laden macrophages.
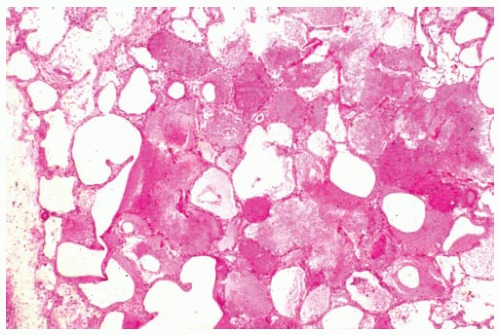 Figure 49.1 Recent pulmonary hemorrhage with alveoli containing dense, granular eosinophilic fluid. Alveolar septum on one side is widened by edema fluid. |
Part 2 Hemorrhage Associated with Infections
Abida K. Haque
Bacterial infections, including mycobacterial infections, with or without associated lung abscess, bronchiectasis, or bronchitis, may cause pulmonary hemorrhage, with potential bacterial etiologies including Staphylococcus aureus, Pseudomonas aeruginosa, and Klebsiella pneumoniae. Viral infections, including cytomegalovirus and herpesvirus, may also cause pulmonary hemorrhage. In endemic areas, paragonimiasis is a parasitic cause of pulmonary hemorrhage. Fungal infections, with or without fungal invasion or mycetoma, may be a cause of pulmonary hemorrhage. Candida and Aspergillus organisms are two potential etiologies, among other fungal organisms.
Histologic Features
Intra-alveolar red blood cells, with variable numbers of leukocytes and hemosiderin-laden macrophages, and variable amounts of fibrin, in association with histologic features of infection (see Chapters 95, 97, and 99).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree