| Schizophrenia |
| Substance-induced (i.e., drug-induced) psychotic disorders |
| Schizophreniform disorder |
| Schizoaffective disorder |
| Delusional disorder |
| Brief psychotic disorder |
| Psychotic disorder due to a general medical condition |
| Mania |
| Depression |
| Cognitive disorders |
| Alzheimer’s dementia |
Psychosis itself can be paranoid, disorganized/excited, or depressive. Perceptual distortions and motor disturbances can be associated with any type of psychosis. Perceptual distortions include being distressed by hallucinatory voices; hearing voices that accuse, blame, or threaten punishment; seeing visions; reporting hallucinations of touch, taste or odor; or reporting that familiar things and people seem changed. Motor disturbances are peculiar, rigid postures; overt signs of tension; inappropriate grins or giggles; peculiar repetitive gestures; talking, muttering, or mumbling to oneself; or glancing around as if hearing voices.
In paranoid psychosis, the patient has paranoid projections, hostile belligerence and grandiose expansiveness. Paranoid projection includes preoccupation with delusional beliefs; believing that people are talking about oneself; believing one is being persecuted or being conspired against; and believing people or external forces control one’s actions. Hostile belligerence is verbal expression of feelings of hostility; expressing an attitude of disdain; manifesting a hostile, sullen attitude; manifesting irritability and grouchiness; tending to blame others for problems; expressing feelings of resentment; complaining and finding fault; as well as expressing suspicion of people. Grandiose expansiveness is exhibiting an attitude of superiority; hearing voices that praise and extol; believing one has unusual powers or is a well-known personality, or that one has a divine mission.
In a disorganized/excited psychosis there is conceptual disorganization, disorientation, and excitement. Conceptual disorganization can be characterized by giving answers that are irrelevant or incoherent, drifting off the subject, using neologisms, or repeating certain words or phrases. Disorientation is not knowing where one is, the season of the year, the calendar year, or one’s own age. Excitement is expressing feelings without restraint; manifesting speech that is hurried; exhibiting an elevated mood; an attitude of superiority; dramatizing oneself or one’s symptoms; manifesting loud and boisterous speech; exhibiting overactivity or restlessness; and exhibiting excess of speech.
Depressive psychosis is characterized by psychomotor retardation, apathy, and anxious self-punishment and blame. Psychomotor retardation and apathy are manifested by slowed speech; indifference to one’s future; fixed facial expression; slowed movements; deficiencies in recent memory; blocking in speech; apathy toward oneself or one’s problems; slovenly appearance; low or whispered speech; and failure to answer questions. Anxious self-punishment and blame is the tendency to blame or condemn oneself; anxiety about specific matters; apprehensiveness regarding vague future events; an attitude of self-deprecation, manifesting as a depressed mood; expressing feelings of guilt and remorse; preoccupation with suicidal thoughts, unwanted ideas, and specific fears; and feeling unworthy or sinful.
This discussion of clusters of psychotic symptoms does not constitute diagnostic criteria for any psychotic disorder. It is given merely as a description of several types of symptoms in psychosis to give the reader an overview of the nature of behavioral disturbances associated with the various psychotic illnesses.
Schizophrenia is more than a psychosis
Although schizophrenia is the commonest and best-known psychotic illness, it is not synonymous with psychosis, but is just one of many causes of psychosis. Schizophrenia affects 1% of the population, and in the US there are over 300 000 acute schizophrenic episodes annually. Between 25% and 50% of schizophrenia patients attempt suicide, and 10% eventually succeed, contributing to a mortality rate eight times greater than that of the general population. Life expectancy of a patient with schizophrenia may be 20–30 years shorter than the general population, not only due to suicide, but in particular due to premature cardiovascular disease. Accelerated mortality from premature cardiovascular disease in patients with schizophrenia is caused not only by genetic and lifestyle factors, such as smoking, unhealthy diet, and lack of exercise leading to obesity and diabetes, but also – sorrily – from treatment with some antipsychotic drugs which themselves cause an increased incidence of obesity and diabetes, and thus increase cardiac risk. In the US, over 20% of all social security benefits are used for the care of patients with schizophrenia. The direct and indirect costs of schizophrenia in the US alone are estimated to be in the tens of billions of dollars every year.
Schizophrenia by definition is a disturbance that must last for six months or longer, including at least one month of delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, or negative symptoms. Positive symptoms are listed in Table 4-3 and shown in Figure 4-1. These symptoms of schizophrenia are often emphasized, since they can be dramatic, can erupt suddenly when a patient decompensates into a psychotic episode (often called a psychotic “break,” as in break from reality), and are the symptoms most effectively treated by antipsychotic medications. Delusions are one type of positive symptom, and these usually involve a misinterpretation of perceptions or experiences. The most common content of a delusion in schizophrenia is persecutory, but it may include a variety of other themes including referential (i.e., erroneously thinking that something refers to oneself), somatic, religious, or grandiose. Hallucinations are also a type of positive symptom (Table 4-3) and may occur in any sensory modality (e.g., auditory, visual, olfactory, gustatory, and tactile), but auditory hallucinations are by far the most common and characteristic hallucinations in schizophrenia. Positive symptoms generally reflect an excess of normal functions, and in addition to delusions and hallucinations may also include distortions or exaggerations in language and communication (disorganized speech), as well as in behavioral monitoring (grossly disorganized or catatonic or agitated behavior). Positive symptoms are well known because they are dramatic, are often the cause of bringing a patient to the attention of medical professionals and law enforcement, and are the major target of antipsychotic drug treatments.
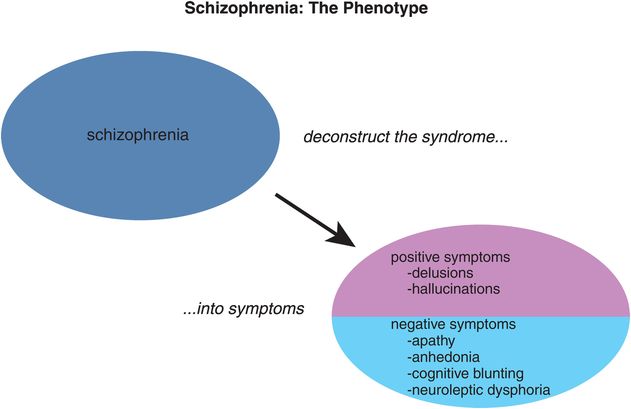
Figure 4-1. Positive and negative symptoms of schizophrenia. The syndrome of schizophrenia consists of a mixture of symptoms that are commonly divided into two major categories, positive and negative. Positive symptoms, such as delusions and hallucinations, reflect the development of the symptoms of psychosis; they can be dramatic and may reflect loss of touch with reality. Negative symptoms reflect the loss of normal functions and feelings, such as losing interest in things and not being able to experience pleasure.
| Delusions |
| Hallucinations |
| Distortions or exaggerations in language and communication |
| Disorganized speech |
| Disorganized behavior |
| Catatonic behavior |
| Agitation |
Negative symptoms are listed in Tables 4-4 and 4-5 and shown in Figure 4-1. Classically, there are at least five types of negative symptoms all starting with the letter A (Table 4-5):
- alogia – dysfunction of communication; restrictions in the fluency and productivity of thought and speech
- affective blunting or flattening – restrictions in the range and intensity of emotional expression
- asociality – reduced social drive and interaction
- anhedonia – reduced ability to experience pleasure
- avolition – reduced desire, motivation or persistence; restrictions in the initiation of goal-directed behavior
| Blunted affect |
| Emotional withdrawal |
| Poor rapport |
| Passivity |
| Apathetic social withdrawal |
| Difficulty in abstract thinking |
| Lack of spontaneity |
| Stereotyped thinking |
| Alogia: restrictions in fluency and productivity of thought and speech |
| Avolition: restrictions in initiation of goal-directed behavior |
| Anhedonia: lack of pleasure |
| Attentional impairment |
| Domain | Descriptive Term | Translation |
|---|---|---|
| Dysfunction of communication | Alogia | Poverty of speech; e.g., talks little, uses few words |
| Dysfunction of affect | Affective blunting | Reduced range of emotions (perception, experience and expression); e.g., feels numb or empty inside, recalls few emotional experiences, good or bad |
| Dysfunction of socialization | Asociality | Reduced social drive and interaction; e.g., little sexual interest, few friends, little interest in spending time with (or little time spent with) friends |
| Dysfunction of capacity for pleasure | Anhedonia | Reduced ability to experience pleasure; e.g., finds previous hobbies or interests unpleasurable |
| Dysfunction of motivation | Avolition | Reduced desire, motivation, persistence; e.g., reduced ability to undertake and complete everyday tasks; may have poor personal hygiene |
Negative symptoms in schizophrenia, such as blunted affect, emotional withdrawal, poor rapport, passivity and apathetic social withdrawal, difficulty in abstract thinking, stereotyped thinking and lack of spontaneity, commonly are considered a reduction in normal functions and are associated with long periods of hospitalization and poor social functioning. Although this reduction in normal functioning may not be as dramatic as positive symptoms, it is interesting to note that negative symptoms of schizophrenia determine whether a patient ultimately functions well or has a poor outcome. Certainly, patients will have disruptions in their ability to interact with others when their positive symptoms are out of control, but their degree of negative symptoms will largely determine whether patients with schizophrenia can live independently, maintain stable social relationships, or re-enter the workplace.
Although formal rating scales can be used to measure negative symptoms in research studies, in clinical practice it may be more practical to identify and monitor negative symptoms quickly by observation alone (Figure 4-2) or by some simple questioning (Figure 4-3). Negative symptoms are not just part of the syndrome of schizophrenia – they can also be part of a “prodrome” that begins with subsyndromal symptoms that do not meet the diagnostic criteria of schizophrenia and occur before the onset of the full syndrome of schizophrenia. Prodromal negative symptoms are important to detect and monitor over time in high-risk patients so that treatment can be initiated at the first signs of psychosis. Negative symptoms can also persist between psychotic episodes once schizophrenia has begun, and reduce social and occupational functioning in the absence of positive symptoms.
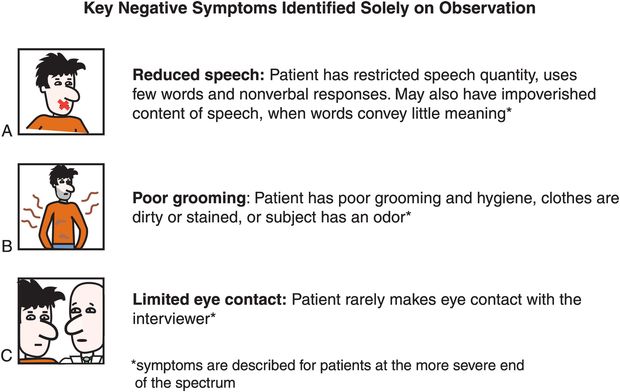
Figure 4-2. Negative symptoms identified by observation. Some negative symptoms of schizophrenia – such as reduced speech, poor grooming, and limited eye contact – can be identified solely by observing the patient.
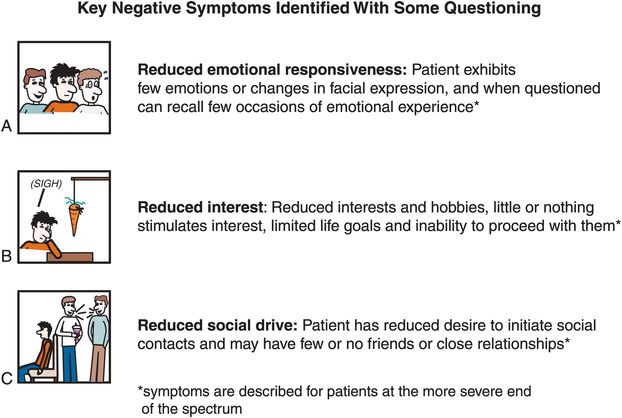
Figure 4-3. Negative symptoms identified by questioning. Other negative symptoms of schizophrenia can be identified by simple questioning. For example, brief questioning can reveal the degree of emotional responsiveness, interest level in hobbies or pursuing life goals, and desire to initiate and maintain social contacts.
Current antipsychotic drug treatments are limited in their ability to treat negative symptoms, but psychosocial interventions along with antipsychotics can be helpful in reducing negative symptoms. There is even the possibility that instituting treatment for negative symptoms during the prodromal phase of schizophrenia may delay or prevent the onset of the illness, but this is still a matter of current research.
Beyond positive and negative symptoms of schizophrenia
Although not recognized formally as part of the diagnostic criteria for schizophrenia, numerous studies subcategorize the symptoms of this illness into five dimensions: not just positive and negative symptoms, but also cognitive symptoms, aggressive symptoms, and affective symptoms (Figure 4-4). This is perhaps a more sophisticated, if complicated, manner of describing the symptoms of schizophrenia.
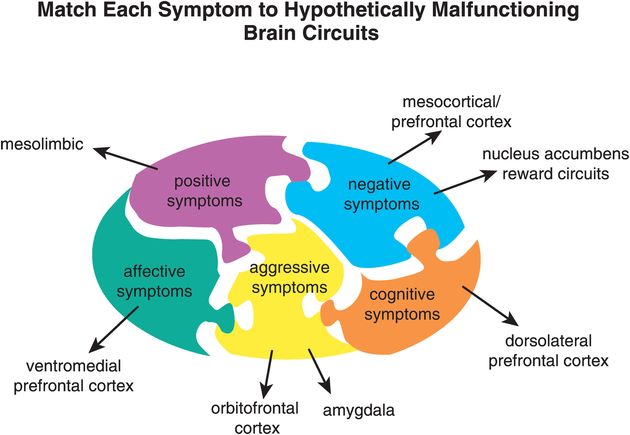
Figure 4-4. Localization of symptom domains. The different symptom domains of schizophrenia are hypothesized to be regulated by unique brain regions. Positive symptoms of schizophrenia are hypothetically modulated by malfunctioning mesolimbic circuits, while negative symptoms are hypothetically linked to malfunctioning mesocortical circuits and may also involve mesolimbic regions such as the nucleus accumbens, which is part of the brain’s reward circuitry and thus plays a role in motivation. The nucleus accumbens may also be involved in the increased rate of substance use and abuse seen in patients with schizophrenia. Affective symptoms are associated with the ventromedial prefrontal cortex, while aggressive symptoms (related to impulse control) are associated with abnormal information processing in the orbitofrontal cortex and amygdala. Cognitive symptoms are associated with problematic information processing in the dorsolateral prefrontal cortex. Although there is overlap in function among different brain regions, understanding which brain regions may be predominantly involved in specific symptoms can aid in customization of treatment to the particular symptom profile of each individual patient with schizophrenia.
Aggressive symptoms such as assaultiveness, verbally abusive behaviors, and frank violence can occur with positive symptoms such as delusions and hallucinations, and be confused with positive symptoms. Behavioral interventions may be particularly helpful to prevent violence linked to poor impulsivity by reducing provocations from the environment. Certain antipsychotic drugs such as clozapine, or very high doses of standard antipsychotic drugs, or occasionally the use of two antipsychotic drugs simultaneously, may also be useful for aggressive symptoms and violence in some patients.
It can also be difficult to separate the symptoms of formal cognitive dysfunction from the symptoms of affective dysfunction and from negative symptoms, but research is attempting to localize the specific areas of brain dysfunction for each symptom domain in schizophrenia in the hope of developing better treatments for the often-neglected negative, cognitive, and affective symptoms of schizophrenia. In particular, neuropsychological assessment batteries are being developed to quantify cognitive symptoms, in order to detect cognitive improvement after treatment with a number of novel psychotropic drugs currently being tested. Cognitive symptoms of schizophrenia are impaired attention and impaired information processing manifested as impaired verbal fluency (ability to produce spontaneous speech), problems with serial learning (of a list of items or a sequence of events), and impairment in vigilance for executive functioning (problems with sustaining and focusing attention, concentrating, prioritizing, and modulating behavior based upon social cues).
Important cognitive symptoms of schizophrenia are listed in Table 4-6. These do not include symptoms of dementia and memory disturbance more characteristic of Alzheimer’s disease, but cognitive symptoms of schizophrenia emphasize “executive dysfunction,” which includes problems representing and maintaining goals, allocating attentional resources, evaluating and monitoring performance, and utilizing these skills to solve problems. Cognitive symptoms of schizophrenia are important to recognize and monitor because they are the single strongest correlate of real-world functioning, even stronger than negative symptoms.
| Problems representing and maintaining goals |
| Problems allocating attentional resources |
| Problems focusing attention |
| Problems sustaining attention |
| Problems evaluating functions |
| Problems monitoring performance |
| Problems prioritizing |
| Problems modulating behavior based upon social cues |
| Problems with serial learning |
| Impaired verbal fluency |
| Difficulty with problem solving |
Symptoms of schizophrenia are not necessarily unique to schizophrenia
It is important to recognize that several illnesses other than schizophrenia can share some of the same five symptom dimensions as described here for schizophrenia and shown in Figure 4-4. Thus, disorders in addition to schizophrenia that can have positive symptoms include bipolar disorder, schizoaffective disorder, psychotic depression, Alzheimer’s disease and other organic dementias, childhood psychotic illnesses, drug-induced psychoses, and others. Negative symptoms can also occur in other disorders and can also overlap with cognitive and affective symptoms that occur in these other disorders. However, as a primary deficit state, negative symptoms are fairly unique to schizophrenia. Schizophrenia is certainly not the only disorder with cognitive symptoms. Autism, post-stroke (vascular or multi-infarct) dementia, Alzheimer’s disease, and many other organic dementias (Parkinsonian/Lewy body dementia, frontotemporal/Pick’s dementia, etc.) can also be associated with cognitive dysfunctions similar to those seen in schizophrenia.
Affective symptoms are frequently associated with schizophrenia but this does not necessarily mean that they fulfill the diagnostic criteria for a comorbid anxiety or affective disorder. Nevertheless, depressed mood, anxious mood, guilt, tension, irritability, and worry frequently accompany schizophrenia. These various symptoms are also prominent features of major depressive disorder, psychotic depression, bipolar disorder, schizoaffective disorder, organic dementias, childhood psychotic disorders, and treatment-resistant cases of depression, bipolar disorder, and schizophrenia, among others. Finally, aggressive and hostile symptoms occur in numerous other disorders, especially those with problems of impulse control. Symptoms include overt hostility, such as verbal or physical abusiveness or assault, self-injurious behaviors including suicide, and arson or other property damage. Other types of impulsiveness such as sexual acting out are also in this category of aggressive and hostile symptoms. These same symptoms are frequently associated with bipolar disorder, childhood psychosis, borderline personality disorder, antisocial personality disorder, drug abuse, Alzheimer’s and other dementias, attention deficit hyperactivity disorder, conduct disorders in children, and many others.
Brain circuits and symptom dimensions in schizophrenia
The various symptoms of schizophrenia are hypothesized to be localized in unique brain regions (Figure 4-4). Specifically, the positive symptoms of schizophrenia have long been hypothesized to be localized to malfunctioning mesolimbic circuits, especially involving the nucleus accumbens. The nucleus accumbens is considered to be part of the brain’s reward circuitry, so it is not surprising that problems with reward and motivation in schizophrenia, symptoms that can overlap with negative symptoms and lead to smoking, drug and alcohol abuse, may be linked to this brain area as well. The prefrontal cortex is considered to be a key node in the nexus of malfunctioning cerebral circuitry responsible for each of the remaining symptoms of schizophrenia: specifically, the mesocortical and ventromedial prefrontal cortex with negative symptoms and affective symptoms, the dorsolateral prefrontal cortex with cognitive symptoms, and the orbitofrontal cortex and its connections to amygdala with aggressive, impulsive symptoms (Figure 4-4).
This model is obviously oversimplified and reductionistic, because every brain area has several functions, and every function is certainly distributed to more than one brain area. Nevertheless, allocating specific symptom dimensions to unique brain areas not only assists research studies, but has both heuristic and clinical value. Specifically, every patient has unique symptoms, and unique responses to medication. In order to optimize and individualize treatment, it can be useful to consider which specific symptoms any given patient is expressing, and therefore which areas of that particular patient’s brain are hypothetically malfunctioning (Figure 4-4). Each brain area has unique neurotransmitters, receptors, enzymes, and genes that regulate it, with some overlap, but also with some unique regional differences, and knowing this can assist the clinician in choosing medications and in monitoring the effectiveness of treatment.
Neurotransmitters and circuits in schizophrenia
Dopamine
The leading hypothesis for schizophrenia is based upon the neurotransmitter dopamine. To understand the potential role of dopamine in schizophrenia, it is first important to review how dopamine is synthesized, metabolized, and regulated; and the role of dopamine receptors and the localization of key dopamine pathways in the brain.
Dopaminergic neurons
Dopaminergic neurons utilize the neurotransmitter dopamine (DA), which is synthesized in dopaminergic nerve terminals from the amino acid tyrosine after it is taken up into the neuron from the extracellular space and bloodstream by a tyrosine pump, or transporter (Figure 4-5). Tyrosine is converted into DA first by the rate-limiting enzyme tyrosine hydroxylase (TOH) and then by the enzyme DOPA decarboxylase (DDC) (Figure 4-5). DA is then taken up into synaptic vesicles by a vesicular monoamine transporter (VMAT2) and stored there until it is used during neurotransmission.
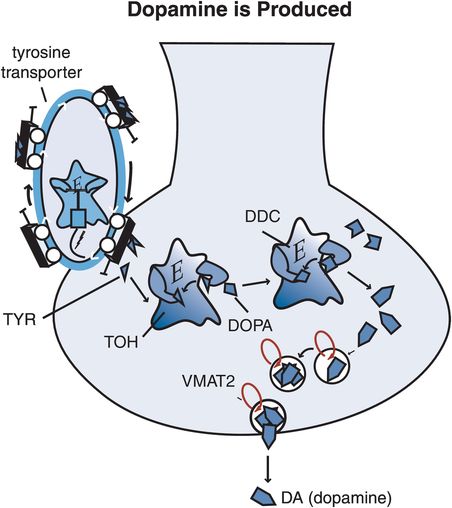
Figure 4-5. Dopamine synthesis. Tyrosine (TYR), a precursor to dopamine, is taken up into dopamine nerve terminals via a tyrosine transporter and converted into DOPA by the enzyme tyrosine hydroxylase (TOH). DOPA is then converted into dopamine (DA) by the enzyme DOPA decarboxylase (DDC). After synthesis, dopamine is packaged into synaptic vesicles via the vesicular monoamine transporter (VMAT2) and stored there until its release into the synapse during neurotransmission.
The DA neuron has a presynaptic transporter (reuptake pump) called DAT, which is unique for DA and which terminates DA’s synaptic action by whisking it out of the synapse back into the presynaptic nerve terminal; there it can be re-stored in synaptic vesicles for subsequent reuse in another neurotransmission (Figure 4-6). DATs are not present in high density at the axon terminals of all DA neurons. For example, in prefrontal cortex, DATs are relatively sparse and DA is inactivated by other mechanisms. Excess DA that escapes storage in synaptic vesicles can be destroyed within the neuron by the enzymes monoamine oxidase (MAO)-A or MAO-B, or outside the neuron by the enzyme catechol-O-methyl-transferase (COMT) (Figure 4-6). DA that diffuses away from synapses can also be transported by norepinephrine transporters (NETs) as a “false” substrate, and DA action will be terminated in this manner.
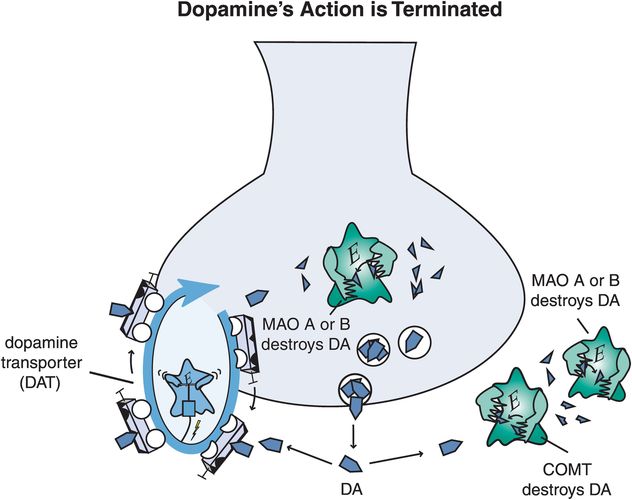
Figure 4-6. Dopamine’s action is terminated. Dopamine’s action can be terminated through multiple mechanisms. Dopamine can be transported out of the synaptic cleft and back into the presynaptic neuron via the dopamine transporter (DAT), where it may be repackaged for future use. Alternatively, dopamine may be broken down extracellularly via the enzyme catechol-O-methyl-transferase (COMT). Other enzymes that break down dopamine are monoamine oxidase A (MAO-A) and monoamine oxidase B (MAO-B), which are present in mitochondria within the presynaptic neuron and in other cells such as glia.
Receptors for dopamine also regulate dopaminergic neurotransmission (Figure 4-7). The DA transporter DAT and the vesicular transporter VMAT2 are both types of receptors. A plethora of additional dopamine receptors exist, including at least five pharmacological subtypes and several more molecular isoforms. Perhaps the most extensively investigated dopamine receptor is the dopamine 2 (D2) receptor, as it is stimulated by dopamine agonists for the treatment of Parkinson’s disease, and blocked by dopamine antagonist antipsychotics for the treatment of schizophrenia. As will be discussed in greater detail in Chapter 5 on antipsychotic drugs, dopamine 1, 2, 3, and 4 receptors are all blocked by some atypical antipsychotic drugs, but it is not clear to what extent dopamine 1, 3, or 4 receptors contribute to the clinical properties of these drugs.
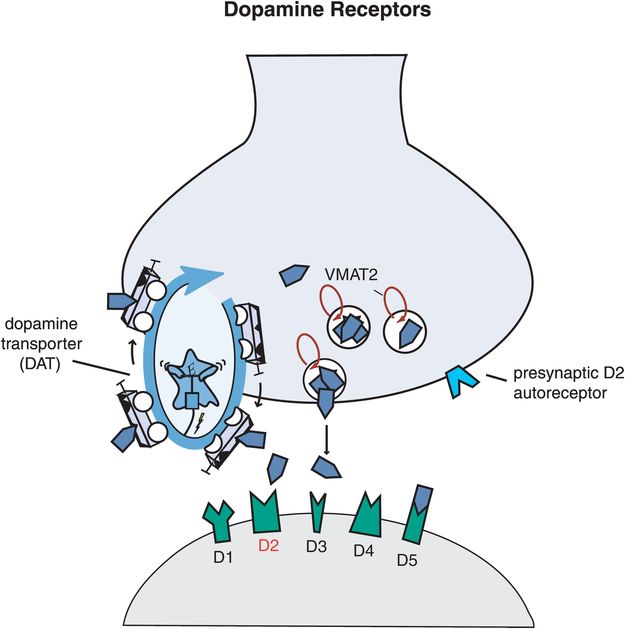
Figure 4-7. Dopamine receptors. Shown here are receptors for dopamine that regulate its neurotransmission. The dopamine transporter (DAT) exists presynaptically and is responsible for clearing excess dopamine out of the synapse. The vesicular monoamine transporter (VMAT2) takes dopamine up into synaptic vesicles for future neurotransmission. There is also a presynaptic dopamine D2 autoreceptor, which regulates release of dopamine from the presynaptic neuron. In addition, there are several postsynaptic receptors. These include D1, D2, D3, D4, and D5 receptors. The functions of the D2 receptors are best understood, because this is the primary binding site for virtually all antipsychotic agents as well as for dopamine agonists used to treat Parkinson’s disease.
Dopamine 2 receptors can be presynaptic, where they function as autoreceptors (Figure 4-7). Presynaptic D2 receptors thus act as “gatekeepers,” either allowing DA release when they are not occupied by DA (Figure 4-8A) or inhibiting DA release when DA builds up in the synapse and occupies these gatekeeping presynaptic autoreceptors (Figure 4-8B). Such receptors are located either on the axon terminal (Figure 4-9) or on the other end of the neuron in the somatodendritic area (Figure 4-10). In both cases, occupancy of these D2 receptors provides negative feedback input, or a braking action upon the release of dopamine from the presynaptic neuron.
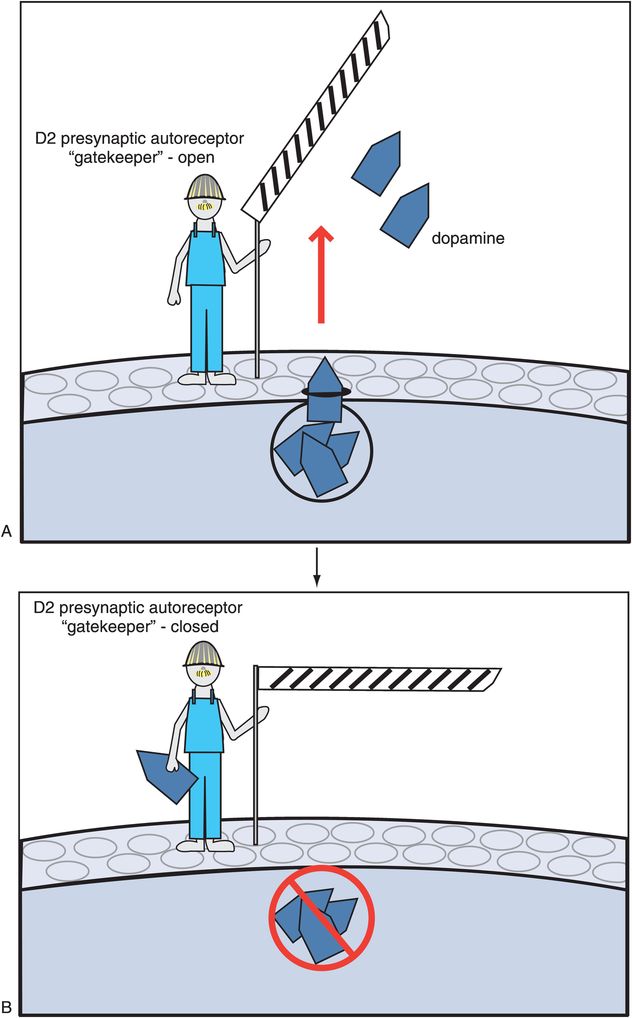
Figure 4-8. Presynaptic dopamine 2 (D2) autoreceptors. Presynaptic D2 autoreceptors are “gatekeepers” for dopamine. That is, when these gatekeeping receptors are not bound by dopamine (no dopamine in the gatekeeper’s hand), they open a molecular gate, allowing dopamine release (A). However, when dopamine binds to the gatekeeping receptors (now the gatekeeper has dopamine in his hand), they close the molecular gate and prevent dopamine from being released (B).
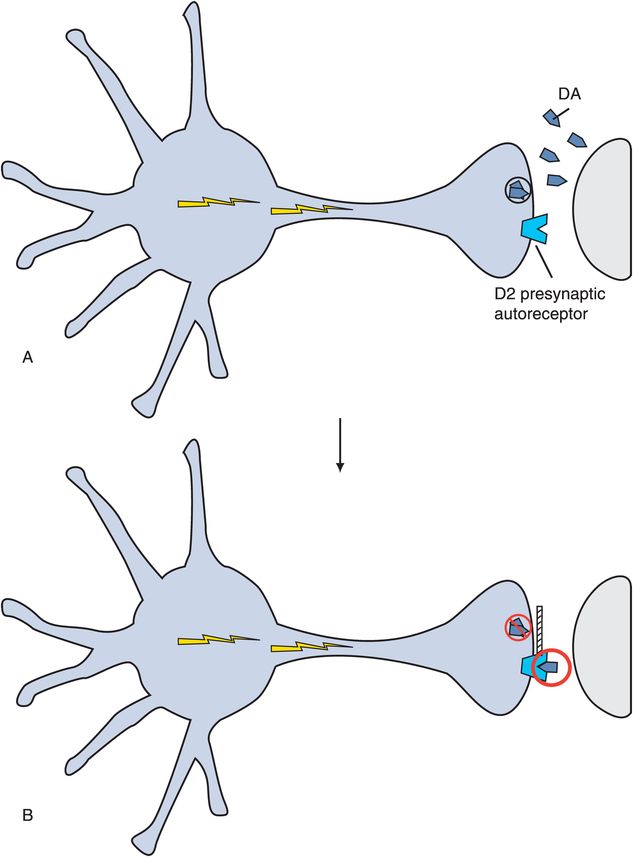
Figure 4-9. Presynaptic dopamine-2 autoreceptors. Presynaptic D2 autoreceptors can be located on the axon terminal, as shown here. When dopamine builds up in the synapse (A), it is available to bind to the autoreceptor, which then inhibits dopamine release (B).
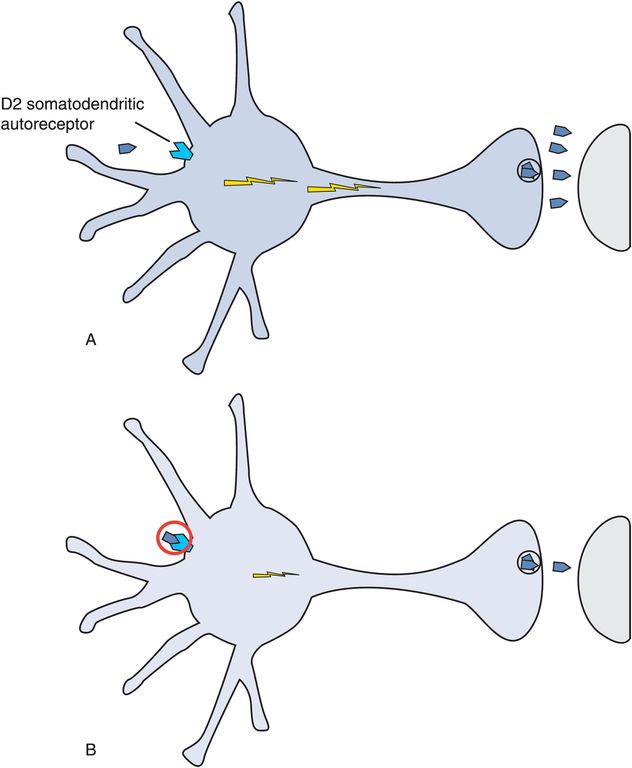
Figure 4-10. Somatodendritic dopamine-2 autoreceptors. D2 autoreceptors can also be located in the somatodendritic area, as shown here (A). When dopamine binds to the receptor here, it shuts off neuronal impulse flow in the dopamine neuron (see loss of lightning bolts in the neuron in B), and this stops further dopamine release.
Key dopamine pathways in the brain
The five dopamine pathways in the brain are shown in Figure 4-11. They include the mesolimbic dopamine pathway, the mesocortical dopamine pathway, the nigrostriatal dopamine pathway, the tuberoinfundibular dopamine pathway, and a fifth pathway that innervates the thalamus.
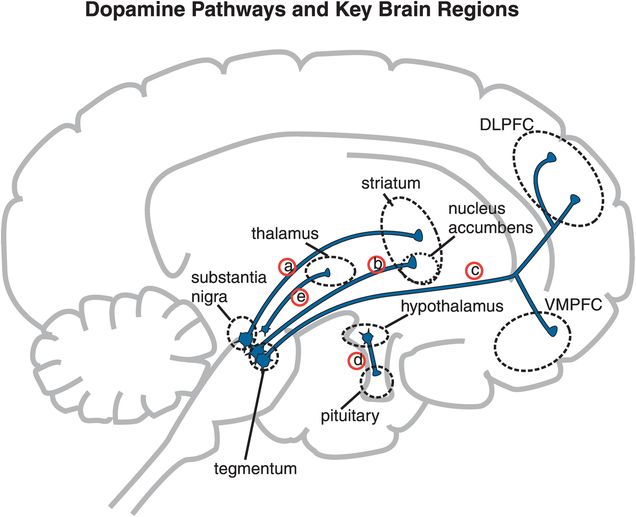
Figure 4-11. Five dopamine pathways in the brain. The neuroanatomy of dopamine neuronal pathways in the brain can explain the symptoms of schizophrenia as well as the therapeutic effects and side effects of antipsychotic drugs. (a) The nigrostriatal dopamine pathway, which projects from the substantia nigra to the basal ganglia or striatum, is part of the extrapyramidal nervous system and controls motor function and movement. (b) The mesolimbic dopamine pathway projects from the midbrain ventral tegmental area to the nucleus accumbens, a part of the limbic system of the brain thought to be involved in many behaviors such as pleasurable sensations, the powerful euphoria of drugs of abuse, as well as delusions and hallucinations of psychosis. (c) A pathway related to the mesolimbic dopamine pathway is the mesocortical dopamine pathway. It also projects from the midbrain ventral tegmental area but sends its axons to areas of the prefrontal cortex, where they may have a role in mediating cognitive symptoms (dorsolateral prefrontal cortex, DLPFC) and affective symptoms (ventromedial prefrontal cortex, VMPFC) of schizophrenia. (d) The fourth dopamine pathway of interest, the tuberoinfundibular dopamine pathway, projects from the hypothalamus to the anterior pituitary gland and controls prolactin secretion. (e) The fifth dopamine pathway arises from multiple sites, including the periaqueductal gray, ventral mesencephalon, hypothalamic nuclei, and lateral parabrachial nucleus, and it projects to the thalamus. Its function is not currently well known.
The dopamine hypothesis of schizophrenia: the mesolimbic dopamine pathway and positive symptoms of schizophrenia
The mesolimbic dopamine pathway projects from dopaminergic cell bodies in the ventral tegmental area of the brainstem to axon terminals in one of the limbic areas of the brain, namely the nucleus accumbens in the ventral striatum (Figure 4-11). This pathway is thought to have an important role in several emotional behaviors, including the positive symptoms of psychosis, such as delusions and hallucinations (Figure 4-12). The mesolimbic dopamine pathway also is important for motivation, pleasure, and reward.
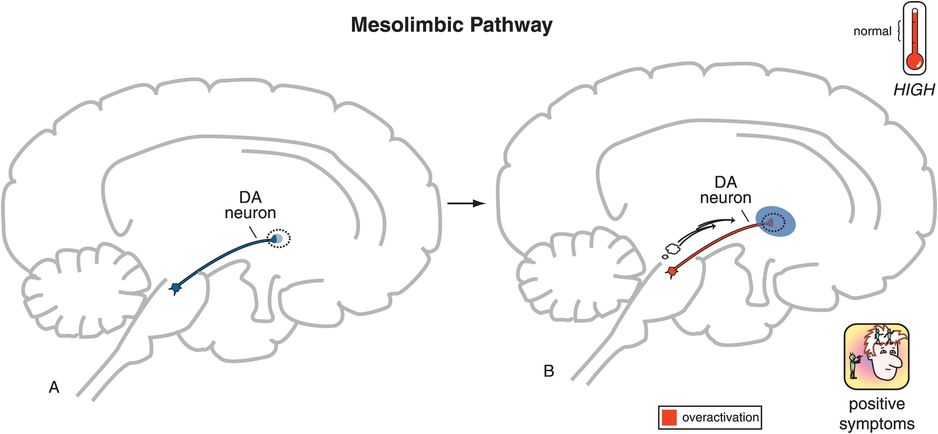
Figure 4-12. Mesolimbic dopamine pathway. The mesolimbic dopamine pathway, which projects from the ventral tegmental area in the brainstem to the nucleus accumbens in the ventral striatum (A), is involved in regulation of emotional behaviors and is believed to be the predominant pathway regulating positive symptoms of psychosis. Specifically, hyperactivity of this pathway is believed to account for delusions and hallucinations (B).
For more than 40 years, it has been observed that diseases or drugs that increase dopamine will enhance or produce positive psychotic symptoms, whereas drugs that decrease dopamine will decrease or stop positive symptoms. For example, stimulant drugs such as amphetamine and cocaine release dopamine, and if given repetitively can cause a paranoid psychosis virtually indistinguishable from the positive symptoms of schizophrenia. Stimulant drugs are discussed in detail in subsequent chapters on treatment of attention deficit hyperactivity disorder, and on drug abuse.
All known antipsychotic drugs capable of treating positive psychotic symptoms are blockers of the dopamine D2 receptor. Antipsychotic drugs are discussed in Chapter 5. These observations have been formulated into a theory of psychosis sometimes referred to as the “dopamine hypothesis of schizophrenia.” Perhaps a more precise modern designation is the “mesolimbic dopamine hypothesis of positive symptoms of schizophrenia,” since it is believed that it is hyperactivity specifically in this particular dopamine pathway that mediates the positive symptoms of psychosis (Figure 4-13). Hyperactivity of the mesolimbic dopamine pathway hypothetically accounts for positive psychotic symptoms whether those symptoms are part of the illness of schizophrenia, or of drug-induced psychosis, or whether they are positive psychotic symptoms accompanying mania, depression, or dementia. Hyperactivity of mesolimbic dopamine neurons may also play a role in aggressive and hostile symptoms in schizophrenia and related illnesses, especially if serotonergic control of dopamine is aberrant in patients who lack impulse control. Although it is not known what causes this mesolimbic dopamine hyperactivity, current theories now state that it is the downstream consequence of dysfunction in prefrontal cortex and hippocampal glutamate activity, as will be discussed below.
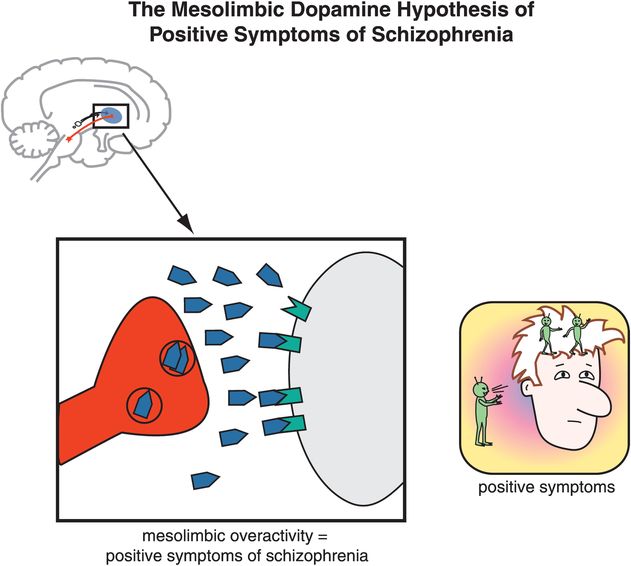
Figure 4-13. Mesolimbic dopamine hypothesis. Hyperactivity of dopamine neurons in the mesolimbic dopamine pathway theoretically mediates the positive symptoms of psychosis such as delusions and hallucinations. This pathway is also involved in pleasure, reward, and reinforcing behavior, and many drugs of abuse interact here.
The mesocortical dopamine pathway and cognitive, negative, and affective symptoms of schizophrenia
Another pathway also arising from cell bodies in the ventral tegmental area, but projecting to areas of the prefrontal cortex, is known as the mesocortical dopamine pathway (Figures 4-14 and 4-15). Branches of this pathway into the dorsolateral prefrontal cortex are hypothesized to regulate cognition and executive functions (Figure 4-14), whereas branches of this pathway into the ventromedial parts of the prefrontal cortex are hypothesized to regulate emotions and affect (Figure 4-15). The exact role of the mesocortical dopamine pathway in mediating symptoms of schizophrenia is still a matter of debate, but many researchers believe that cognitive and some negative symptoms of schizophrenia may be due to a deficit of dopamine activity in mesocortical projections to dorsolateral prefrontal cortex (Figure 4-14), whereas affective and other negative symptoms of schizophrenia may be due to a deficit of dopamine activity in mesocortical projections to ventromedial prefrontal cortex (Figure 4-15).
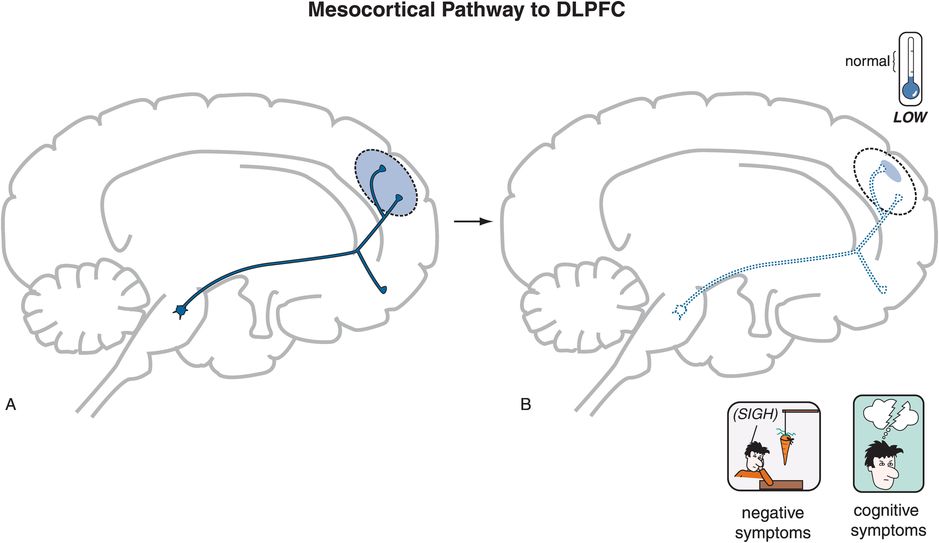
Figure 4-14. Mesocortical pathway to dorsolateral prefrontal cortex. Another major dopaminergic pathway is the mesocortical dopamine pathway, which projects from the ventral tegmental area to the prefrontal cortex (A). Projections specifically to the dorsolateral prefrontal cortex (DLPFC) are believed to be involved in the negative and cognitive symptoms of schizophrenia. In this case, expression of these symptoms is thought to be associated with hypoactivity of this pathway (B).
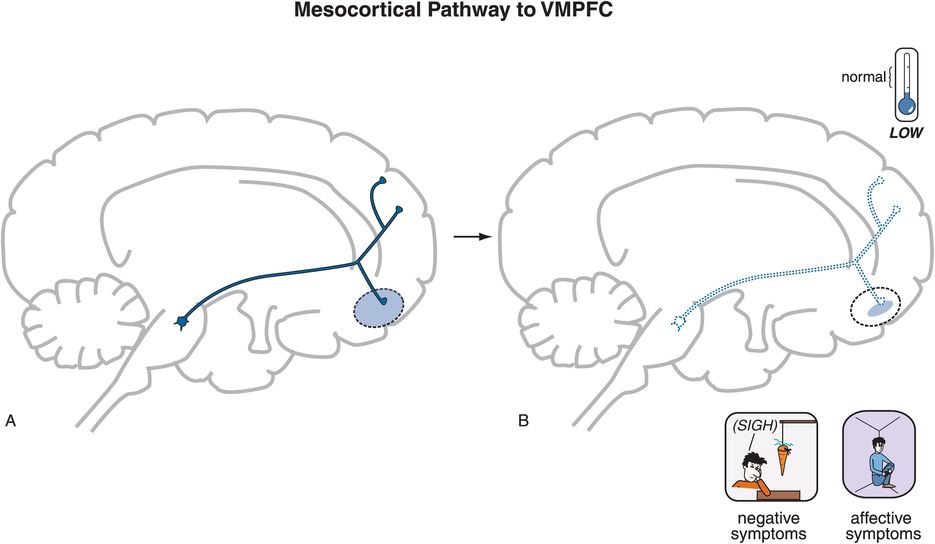
Figure 4-15. Mesocortical pathway to ventromedial prefrontal cortex. Mesocortical dopamine projections specifically to the ventromedial prefrontal cortex (VMPFC) are believed to mediate negative and affective symptoms associated with schizophrenia (A). These symptoms are believed to arise from hypoactivity in this pathway (B).
The behavioral deficit state suggested by negative symptoms certainly implies underactivity or lack of proper functioning of mesocortical dopamine projections that may be the consequence of neurodevelopmental abnormalities in the NMDA (N-methyl-D-aspartate) glutamate system, described in the next section. Whatever the cause, a corollary to the original DA hypothesis of schizophrenia now incorporates theories for the cognitive, negative, and affective symptoms, and might be more precisely designated as the “mesocortical dopamine hypothesis of cognitive, negative, and affective symptoms of schizophrenia,” since it is believed that it is underactivity specifically in mesocortical projections to prefrontal cortex that mediate the cognitive, negative, and affective symptoms of schizophrenia (Figure 4-16).
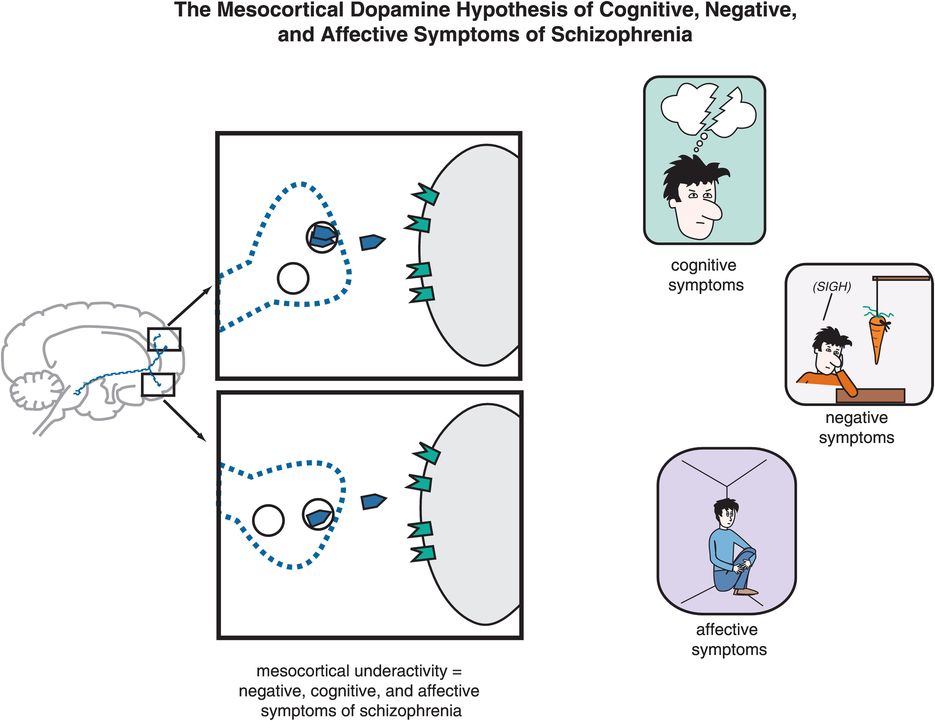
Figure 4-16. Mesocortical dopamine hypothesis of negative, cognitive, and affective symptoms of schizophrenia. Hypoactivity of dopamine neurons in the mesocortical dopamine pathway theoretically mediates the cognitive, negative, and affective symptoms of schizophrenia.
Theoretically, increasing dopamine in the mesocortical dopamine pathway might improve negative, cognitive, and affective symptoms of schizophrenia. However, since there is hypothetically an excess of dopamine elsewhere in the brain – within the mesolimbic dopamine pathway – any further increase of dopamine in that pathway would actually worsen positive symptoms. Thus, this state of affairs for dopamine activity in the brain of patients with schizophrenia poses a therapeutic dilemma: how do you increase dopamine in the mesocortical pathway while simultaneously decreasing dopamine activity in the mesolimbic dopamine pathway? The extent to which atypical antipsychotics have provided a solution to this therapeutic dilemma will be discussed in Chapter 5.
Mesolimbic dopamine pathway, reward and negative symptoms
When a patient with schizophrenia loses motivation and interest, and has anhedonia and lack of pleasure, such symptoms could also implicate a deficient functioning of the mesolimbic dopamine pathway, not just deficient functioning in the mesocortical dopamine pathway. This idea is supported by observations that treating patients with antipsychotics, particularly the conventional antipsychotics, can produce a worsening of negative symptoms and a state of “neurolepsis” that looks very much like negative symptoms of schizophrenia. Since the prefrontal cortex does not have a high density of D2 receptors, this implicates possible deficient functioning within the mesolimbic dopamine system causing inadequate reward mechanisms, exhibited as behaviors such as anhedonia and drug abuse, as well as negative symptoms, exhibited as lack of rewarding social interactions, and lack of general motivation and interest. Perhaps the much higher incidence of substance abuse in schizophrenia than in healthy adults, especially of nicotine but also of stimulants and other substances of abuse, could be partially explained as an attempt to boost the function of defective mesolimbic dopaminergic pleasure centers, perhaps at the cost of activating positive symptoms.
Nigrostriatal dopamine pathway
Another key dopamine pathway in the brain is the nigrostriatal dopamine pathway, which projects from dopaminergic cell bodies in the brainstem substantia nigra via axons terminating in the basal ganglia or striatum (Figure 4-17). The nigrostriatal dopamine pathway is a part of the extrapyramidal nervous system, and controls motor movements. Deficiencies in dopamine in this pathway cause movement disorders including Parkinson’s disease, characterized by rigidity, akinesia/bradykinesia (i.e., lack of movement or slowing of movement), and tremor. Dopamine deficiency in the basal ganglia also can produce akathisia (a type of restlessness), and dystonia (twisting movements especially of the face and neck). These movement disorders can be replicated by drugs that block D2 receptors in this pathway, and this will be discussed briefly in Chapter 5.
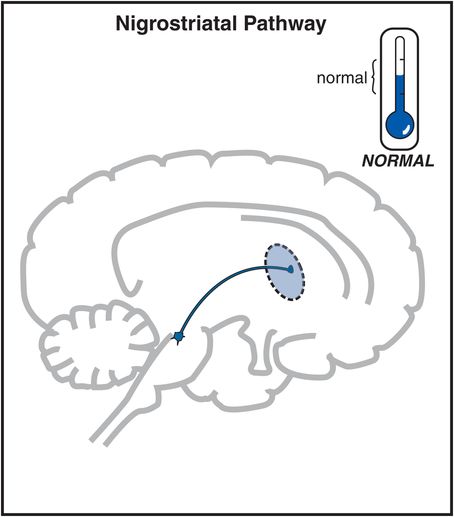
Figure 4-17. Nigrostriatal dopamine pathway. The nigrostriatal dopamine pathway projects from the substantia nigra to the basal ganglia or striatum. It is part of the extrapyramidal nervous system and plays a key role in regulating movements. When dopamine is deficient, it can cause parkinsonism with tremor, rigidity, and akinesia/bradykinesia. When DA is in excess, it can cause hyperkinetic movements such as tics and dyskinesias. In untreated schizophrenia, activation of this pathway is believed to be “normal.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


