INTRODUCTION
The pseudomonads and Acinetobacter species are widely distributed in soil and water. Pseudomonas aeruginosa sometimes colonizes humans and is the major human pathogen of the pseudomonads. P aeruginosa is invasive and toxigenic, produces infections in patients with abnormal host defenses, and is an important nosocomial pathogen. Of the Acinetobacter species, Acinetobacter baumannii is responsible for most human infections. It is a significant nosocomial pathogen, especially in critical or intensive care units, and is frequently resistant to multiple antibiotics.
THE PSEUDOMONAD GROUP
The pseudomonads are Gram-negative, motile, aerobic rods, some of which produce water-soluble pigments. The pseudomonads occur widely in soil, water, plants, and animals. P aeruginosa is frequently present in small numbers in the normal intestinal flora and on the skin of humans, and is the major pathogen of the group. Other pseudomonads infrequently cause disease. The classification of pseudomonads is based on rRNA/DNA homology and common culture characteristics.
PSEUDOMONAS AERUGINOSA
P aeruginosa is widely distributed in nature and is commonly present in moist environments in hospitals. It can colonize normal humans, in whom it is a saprophyte. It causes disease in humans with abnormal host defenses, especially in individuals with neutropenia.
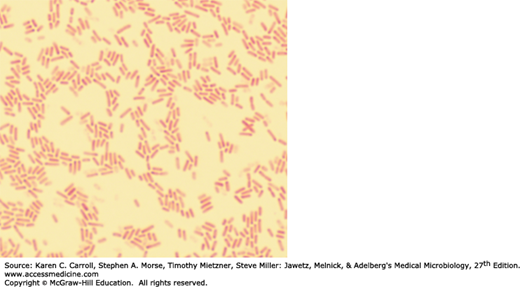
P aeruginosa is motile and rod shaped, measuring about 0.6 × 2 μm (Figure 16-1). It is Gram-negative and occurs as single bacteria, in pairs, and occasionally in short chains.
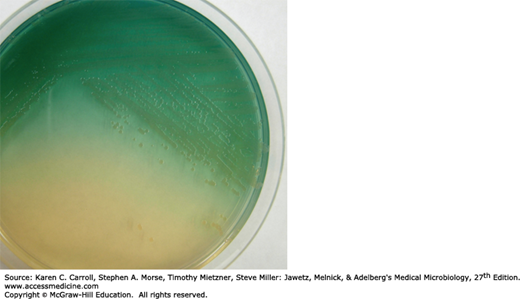
P aeruginosa is an obligate aerobe that grows readily on many types of culture media, sometimes producing a sweet or grape-like or corn taco–like odor. Some strains hemolyze blood. P aeruginosa forms smooth round colonies with a fluorescent greenish color. It often produces the nonfluorescent bluish pigment pyocyanin, which diffuses into the agar. Other Pseudomonas species do not produce pyocyanin. Many strains of P aeruginosa also produce the fluorescent pigment pyoverdin, which gives a greenish color to the agar (Figure 16-2). Some strains produce the dark red pigment pyorubin or the black pigment pyomelanin.
FIGURE 16-2
Pseudomonas aeruginosa on a 10-cm Mueller-Hinton agar plate. Individual colonies are 3–4 mm in diameter. The organism produces pyocyanin, which is blue, and pyoverdin, which is green. Together these pigments produce the blue-green color that is seen in the agar around the pseudomonas growth. (Courtesy of S Lowe.)
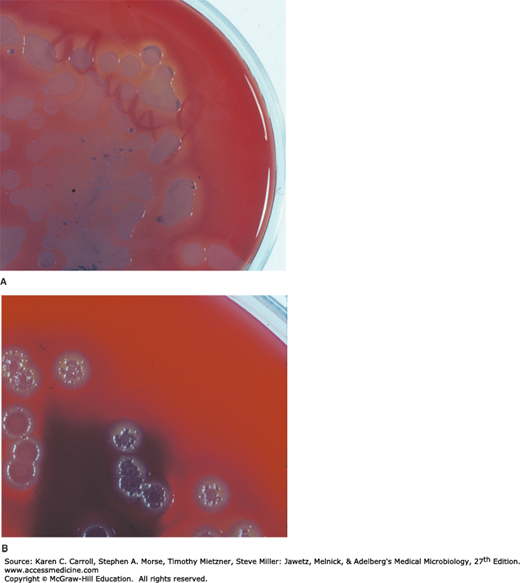
P aeruginosa in a culture can produce multiple colony types (Figure 16-3). P aeruginosa from different colony types may also have different biochemical and enzymatic activities and different antimicrobial susceptibility patterns. Sometimes, it is not clear if the colony types represent different strains of P aeruginosa or are variants of the same strain. Cultures from patients with cystic fibrosis (CF) often yield P aeruginosa organisms that form mucoid colonies as a result of overproduction of alginate, an exopolysaccharide. In CF patients, the exopolysaccharide appears to provide the matrix for the organisms to live in a biofilm (see Chapters 2 and 9).
FIGURE 16-3
Variation in colony morphology of Pseudomonas aeruginosa. A: Green-gray colonies 6–8 mm in diameter on a 10-cm blood agar plate; the blood in the agar around the colonies shows hemolysis. B: Silver-toned dry colonies on a similar blood agar plate; no hemolysis is present (the dark shadow in the lower part of the picture is from a label on the back of the Petri dish). (Courtesy of H Reyes.)
P aeruginosa grows well at 37–42°C; its growth at 42°C helps differentiate it from other Pseudomonas species that produce fluorescent pigments. It is oxidase positive. It does not ferment carbohydrates, but many strains oxidize glucose. Identification is usually based on colonial morphology, oxidase positivity, the presence of characteristic pigments, and growth at 42°C. Differentiation of P aeruginosa from other pseudomonads on the basis of biochemical activity requires testing with a large battery of substrates.
Pili (fimbriae) extend from the cell surface and promote attachment to host epithelial cells. An exopolysaccharide, alginate, is responsible for the mucoid colonies seen in cultures from patients with CF. Lipopolysaccharide, which exists in multiple immunotypes, is responsible for many of the endotoxic properties of the organism. P aeruginosa can be typed by lipopolysaccharide immunotype and by pyocin (bacteriocin) susceptibility. Most P aeruginosa isolates from clinical infections produce extracellular enzymes, including elastases, proteases, and two hemolysins (a heat-labile phospholipase C and a heat-stable glycolipid).
Many strains of P aeruginosa produce exotoxin A, which causes tissue necrosis and is lethal for animals when injected in purified form. The toxin blocks protein synthesis by a mechanism of action identical to that of diphtheria toxin, although the structures of the two toxins are not identical. Antitoxins to exotoxin A are found in some human sera, including those of patients who have recovered from serious P aeruginosa infections.
P aeruginosa produces four type III–secreted toxins that cause cell death or interfere with the host immune response to infection. Exoenzyme S and exoenzyme T are bifunctional enzymes with GTPase and ADP-ribosyl transferase activity; exoenzyme U is a phospholipase, and exoenzyme Y is an adenylyl cyclase.