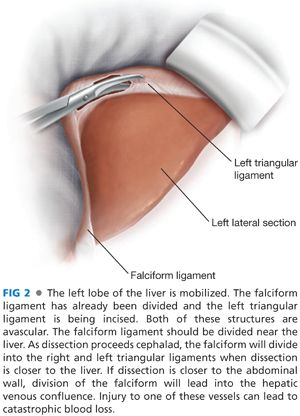
■ The left lateral section of the liver is mobilized to expose the lesser curve of the stomach and the esophageal hiatus: The left triangular ligament is incised. This is avascular. The falciform ligament may also be incised to aid with visualization of the left triangular ligament (FIG 2). The ligament need not be mobilized to its confluence with the falciform to avoid injury to the left hepatic vein. The gastrohepatic ligament is divided. This structure is typically also avascular, but attention should be paid for any accessory or replaced left hepatic artery (FIG 3). This will allow exposure of the esophageal crura.
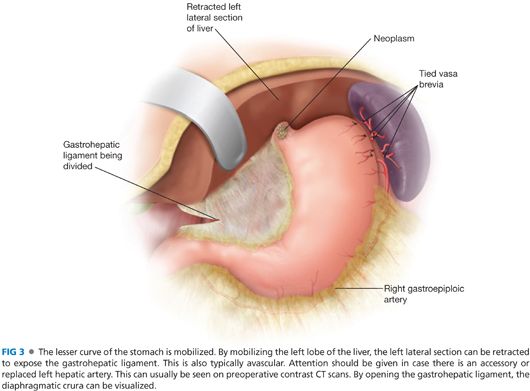
■ The gastrosplenic ligament is divided between clamps and ties. The vasa brevia are individually dissected and divided between ties. Alternative strategies for division of this structure would include an advanced energy device or an articulating 45-mm stapler with vascular loads.
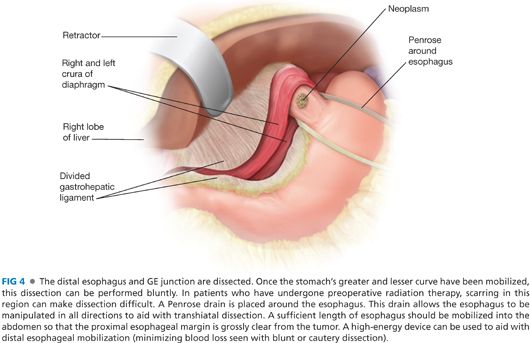
■ The distal esophagus is circumferentially freed using a combination of sharp and blunt dissection. A Penrose drain is placed around the esophagus to aid with retraction (FIG 4). The Penrose drain can be used to retract the esophagus to expose the diaphragmatic hiatus and aid with lower mediastinal dissection. The hiatal attachments of the esophagus are taken down with an advanced energy device. The hiatus should be opened to facilitate dissection of the esophagus. During this dissection, it may be necessary to put pressure on the heart to free the mediastinal attachments of the esophagus. The proximal extent of the tumor and the length of the intraabdominal esophagus will dictate the amount of mediastinal dissection necessary.
■ With the stomach reflected anteriorly, the left gastric vessels are ligated (FIG 5). Prior to ligation, the left gastric artery is test clamped to make sure that flow remains in both the common hepatic artery and the splenic artery. The left gastric artery is ligated at its root off the celiac trunk to facilitate appropriate lymphadenectomy.

GASTROESOPHAGEAL RESECTION AND RECONSTRUCTION
■ Using the NG tube as a guide, place two purse-string sutures in the esophagus proximal to the neoplasm (FIG 6). These will be an alternating horizontal mattress to ensure complete donuts after stapling. Do not allow the sutures to go through the NG tube.

■ Anesthesia should retract the NG tube into the esophagus. Partially divide the esophagus with electrocautery below the purse-string sutures and above the neoplasm. The posterior wall of the esophagus and the purse-string sutures are used to keep the proximal esophagus in an intraabdominal position. The anvil of a circular linear stapling device is placed in the esophagus and the purse-string sutures are tied. The division of the esophagus is completed. The GE junction can now be delivered extracorporally. A proximal surgical margin is sent for frozen section analysis. Typically, a 25-mm circular stapler will be sufficient for reconstruction.
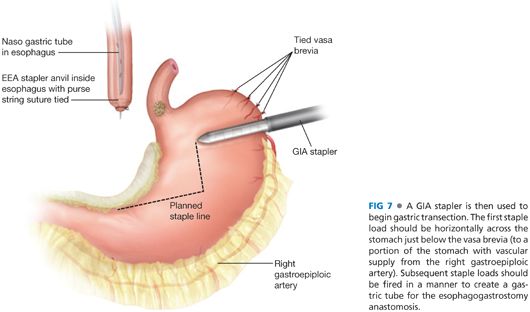
■ Multiple firings of the gastrointestinal anastomosis (GIA) linear stapler are used to both resect the proximal stomach while tubularizing the remaining stomach for the reconstruction. The first staple load is deployed perpendicular to the greater curvature of the stomach. The stapler is fired sequentially toward the lesser curve, creating a gastric tube (FIG 7). The stomach should not be completely transected.
■ A gastrotomy is created along the lesser curve to allow placement of the handle of a circular stapling device. This gastrotomy should be positioned so that it will be resected as part with additional firings of the GIA linear stapler to completely transect the proximal stomach. The stapler is attached to its anvil in the proximal esophagus and fired (FIG 8). The anastomotic donuts are examined to ensure that two intact rings are present. The esophagogastrectomy is completed with additional firings of the GIA stapler to excise the gastrotomy site, the proximal stomach, the tumor, and the distal esophagus. Tension from the proximal esophagus will usually retract the anastomosis into the thorax. A closed suction drain should be placed at the anastomosis. The NG tube should be advanced into the stomach.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


