Primary Myelofibrosis
Kaaren K. Reichard, MD
Key Facts
Terminology
Definition
Clonal stem cell disorder
Megakaryocytic and granulocytic proliferation with ultimate fibrosis
Clinical Issues
Extramedullary hematopoiesis
Microvascular complications
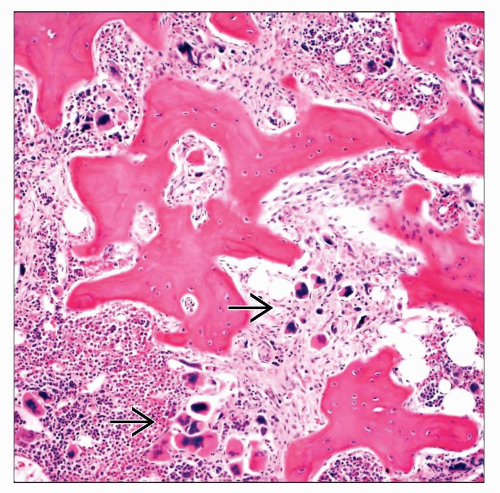
Microscopic Pathology
Early phase
Variable anemia, thrombocytosis, and granulocytic leukocytosis
BM absent/minimal fibrosis
BM pleomorphic megakaryocytes
Late/fibrotic phase
PB leukoerythroblastosis
BM marked fibrosis
BM osteosclerosis
Ancillary Tests
Cytogenetics
Common recurring abnormalities: +8, +9, 13q-, 20q
Not specific for PMF
Molecular genetics
JAK2 V617F mutation present in ˜ 50% of patients
BCR-ABL1 negative
Top Differential Diagnoses
Other classic BCR-ABL1 negative MPNs
Chronic myelogenous leukemia, BCR-ABL1 positive
Secondary causes of leukoerythroblastosis
TERMINOLOGY
Abbreviations
Primary myelofibrosis (PMF)
Synonyms
Chronic idiopathic myelofibrosis
Agnogenic myeloid metaplasia
Myeloid metaplasia with myelofibrosis
Definitions
Myeloproliferative neoplasm (MPN)
Clonal stem cell disorder
Manifests as megakaryocytic and granulocytic proliferation with ultimate fibrosis
PMF term should be used in patients without diagnosis of essential thrombocythemia (ET) or polycythemia vera (PV)
ETIOLOGY/PATHOGENESIS
Molecular Pathogenesis
JAK2 V617F mutation present in ˜ 50% of patients
MPL mutations at codon 515 present in ˜ 10% of patients
BCR-ABL1 fusion absent
Fibrosis Hypothesis
Secondary proliferation of polyclonal fibroblasts
Fibroblasts are stimulated by clonally expanding megakaryocytes via TGF-β
Leukemia Transformation
May be JAK2 negative (even if PMF was originally JAK2 positive)
CLINICAL ISSUES
Epidemiology
Incidence
∽ 0.2/100,000 in United States
Age
Median age at diagnosis: 67 years
Predominantly adults
Gender
No significant sex predilection
Site
Peripheral blood (PB)
Bone marrow (BM)
Spleen
Liver
Presentation
Abdominal fullness
Fatigue
Splenomegaly
Early satiety
Left upper quadrant pain
Musculoskeletal complaints
Fever
Night sweats
Weight loss
Laboratory Tests
Complete blood cell count (CBC)
Peripheral blood smear review
Bone marrow examination
Cytogenetics
Molecular genetics (e.g., JAK2)
Treatment
Only potential cure is allogeneic stem cell transplantation
Toxicity due to myeloablative therapy is prohibitive in many patients
Nonmyeloablative regimens exist
Drug therapy
Targets symptoms
Hydroxyurea
For leukocytosis, thrombocytosis, and splenomegaly
Thalidomide/lenalidomide and steroids
For cytopenias, splenomegaly
Molecular-targeted therapy against JAK2
Splenectomy
High-risk procedure
Near 10% mortality
Prognosis
Median survival: 3.5 to 5 years
Worse than other classic MPNs
Wide range in survival
Prognostic factors
Several prognostic scoring systems
Variables assessed
Age > 65 years
Hemoglobin < 10 g/dL
Leukocyte count > 25 × 109/L
Circulating blasts ≥ 1%
Constitutional symptoms
Leukemic transformation
Poor prognosis
˜ 4-20% of patients
Microvascular events
Thrombosis
Hemorrhage
MICROSCOPIC PATHOLOGY
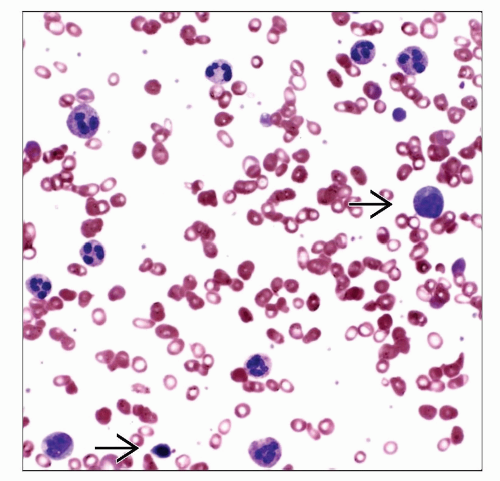
Peripheral Blood
Early/prefibrotic phase
Anemia
Variable thrombocytosis
Platelets may show dysplastic features
Variable granulocytic leukocytosis
Usually mild
No dysplasia
No erythrocytosis
Fibrotic phase
Leukoerythroblastosis
Marked erythroid anisopoikilocytosis including dacrocytes (teardrop forms)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree