Primary Cutaneous CD4+ Small/Medium Pleomorphic T-cell Lymphoma
Aaron Auerbach, MD, PhD
Key Facts
Terminology
T-cell lymphoma of skin with small to medium-sized CD4(+) T cells and usually indolent clinical course
Provisional entity in 2008 WHO Classification of Tumors of Hematopoietic and Lymphoid Tissue
Lacks lesions typical of mycosis fungoides
Clinical Issues
Usually single plaque or tumor
Good prognosis, especially if single lesion
Microscopic Pathology
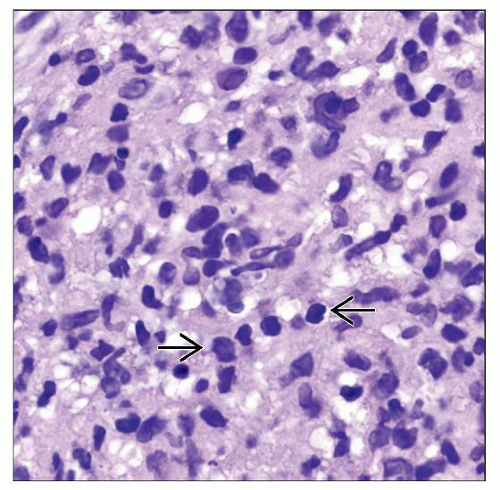
Dense dermal and subcutaneous infiltrate of small/medium-sized pleomorphic T cells
Sometimes focal epidermotropism
Scattered large T cells (< 30% of total)
Background reactive infiltrate
Granulomatous inflammation may be present
Ancillary Tests
CD3(+), CD4(+), CD8(−), CD30(−)
Loss of T-cell antigens
Positive follicular helper T-cell markers (PD1, CXCL13)
Clonal T-cell receptor gene rearrangements
Cytogenetics: No known abnormalities
Epstein-Barr virus small-encoded RNA(−)
Top Differential Diagnoses
Pseudolymphoma of the skin
Mycosis fungoides
Angioimmunoblastic T-cell lymphoma
Peripheral T-cell lymphoma unspecified
Cutaneous B-cell lymphoma
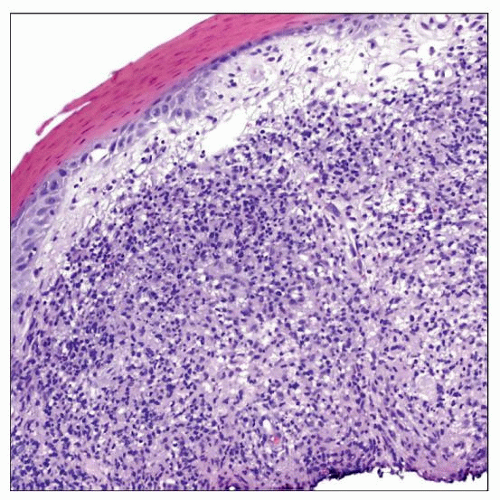 Low-power view of a primary cutaneous CD4(+) small/medium pleomorphic T-cell lymphoma shows a dense lymphoid infiltrate filling the dermis in a diffuse pattern of infiltration. |
TERMINOLOGY
Abbreviations
Primary cutaneous CD4(+) small/medium pleomorphic T-cell lymphoma (SMPTCL)
Synonyms
Idiopathic T-cell lymphomatoid hyperplasia
Definitions
T-cell lymphoma of skin with small to medium-sized CD4(+) T cells, and usually indolent clinical course
Without typical patches/plaques of mycosis fungoides
Provisional entity in 2008 WHO Classification of Tumors of Hematopoietic and Lymphoid Tissue
Nonaggressive natural history, but worrisome histologic and molecular features
ETIOLOGY/PATHOGENESIS
Idiopathic
Cause of this lymphoma unknown Postulated Normal Cell Counterpart
CD4(+) helper T cell
CLINICAL ISSUES
Epidemiology
Incidence
Rare
2% of cutaneous T-cell lymphomas in the Dutch and Austrian Cutaneous Lymphoma Group Registry
Age
Median: 53 years; range: 3-90 years
Gender
M:F = 0.5:1
Site
Head and neck area most common
Upper torso often
Lower extremities rare
Presentation
Single plaque or tumor
Less commonly > 1 tumor nodule
Less commonly ≥ 1 papules
No lesions (patches/plaques) typical of mycosis fungoides
Usually asymptomatic other than skin lesions
No lymphadenopathy
No systemic disease
Laboratory Tests
No known laboratory abnormalities
Natural History
Does not usually disseminate
Rarely, local recurrence is seen
Treatment
Excision
Radiation therapy
Usually nonaggressive therapy
Especially if single lesion
Prognosis
Mostly favorable outcome, especially if solitary lesion or localized to skin
Better prognosis than secondary cutaneous T-cell lymphomas
Better prognosis than primary cutaneous peripheral T-cell lymphoma, not otherwise specified
Nonaggressive disease
Overall 5-year survival: 60-80%
Disease-specific 5-year survival up to 75%
Good prognostic indicators
Solitary lesion
Disease localized to skin
Worse prognostic indicators
Multiple lesions
Large lesions
MACROSCOPIC FEATURES
General Features
Usually single, less often multiple firm lesion(s)
MICROSCOPIC PATHOLOGY
Histologic Features
Dense dermal infiltrate
Sometimes involves subcutaneous tissue
Usually nonepidermotropic
Rarely focal epidermotropism
Growth pattern
Diffuse
Nodular
Size of T cells
Small or medium in most cases
Large cells can also be seen
When present, < 30% of total cells
Pleomorphic with some nuclear irregularity
Other features
Background reactive infiltrate is fairly common
Small reactive lymphocytes, eosinophils, and histiocytes
↑ reactive-appearing B cells also often present
Granulomatous inflammation can be seen
Cytologic Features
Rarely diagnosed by cytology
ANCILLARY TESTS
Immunohistochemistry
T-cell antigens positive
CD2(+), CD3(+), CD5(+), CD7(+)
Rarely loss of 1 or more T-cell antigens
CD7 > CD5, CD2
CD4(+), CD8(−)
Expresses follicular helper T-cell markers
PD1(+), CXCL13(+), Bcl-6(+)
Cytotoxic markers negative
TIA, GZM-B, and perforin
CD30(−), LMP1(−)
Cytogenetics
No known specific abnormalities
In Situ Hybridization
Epstein-Barr virus small-encoded RNA (EBER) negative
PCR
TCR gene rearrangement clonal
60% in one series
IgH immunoglobulin gene rearrangements polyclonal
DIFFERENTIAL DIAGNOSIS
Atypical Reactive Lymphoid Infiltrates (“Pseudolymphomas”) of the Skin
Similarities to SMPTCL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree