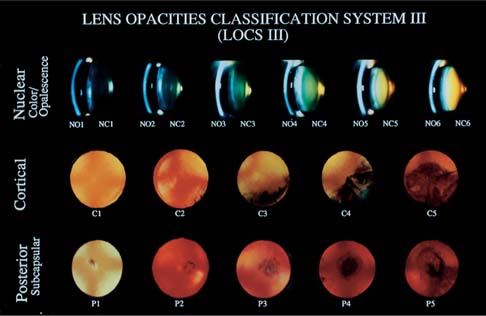
Chapter 29 This chapter discusses my key steps for complication avoidance. But complications do occur, and so I describe the less common but most helpful maneuvers I favor to minimize damage and regain control of the situation. The discussion is not comprehensive. Rather, I present my personal favorites. These pearls work for me today, with my current technique. I am always looking for new and better pearls. As in any human endeavor, a surgeon will benefit from skills that add to strengths and compensate for weaknesses. Read this chapter with an open mind, and try to identify elements that resonate with your own current technique and skill set. Some special steps in the preoperative evaluation will help ensure a good outcome on the day of surgery. In addition to a comprehensive preoperative examination including dilated lens and fundus exam, the surgeon must evaluate the patient from the perspective of the operative day. Is the patient oriented and able to cooperate? Do medical conditions, such as respiratory distress or spinal deformity, make a supine positioning impossible? Particularly if topical anesthesia is being considered, does the patient exhibit a high level of anxiety, or squeeze uncontrollably during applanation pressure measurement? Before narrowing in on the slit-lamp exam, take a moment to look at the orbital configuration. Deep-set eyes, high orbital rims, or a narrow palpebral fissure all argue for a temporal incision. In the eagerness to examine the lens, don’t forget to note and institute preoperative treatment for blepharitis. A history of epiphora may indicate lacrimal outflow obstruction and risk of infection; press on the lacrimal sac. Corneal guttae are easily overlooked; if present, preoperative pachymetry is a better indicator of physiologic endothelial pump function than specular microscopy. In any case, the patient needs to be informed of the increased risk of postoperative corneal decompensation, and the surgeon should put a prominent reminder in the admission note to use particular vigilance, such as extra dispersive viscoelastic, to protect the depleted endothelium. The dilation of the pupil must be noted. Synechiae from prior surgery or inflammation will need to be lysed at the beginning of the surgery. A poorly dilating pupil may mask the presence of underlying pseudoexfoliation, with the combined operative risks of poor dilation and potentially weak zonular support. If pseudoexfoliation material cannot be seen on the limited amount of visible anterior capsule, look carefully for pseudoexfoliation dandruff at the edge of the pupil and on the endothelium. Even if none is seen, the surgeon should note the potential in the admission note as a reminder to look carefully for pseudoexfoliation once the pupil is mechanically stretched at surgery. Preoperative accurate assessment of the cataract itself is very helpful in preparation for a smooth operative procedure. Use of the Lens Opacities Classification System (LOCS) devised by Leo T. Chylack, Jr. and coworkers helps consistent grading of the cataract and encourages a disciplined approach to lens evaluation. The published grading system (Fig. 29–1) was devised as a cataract research tool, but I keep a copy in each examination lane as a clinical guide. FIGURE 29–1 The Lens Opacities Classification System, revision III (LOCS III). (Courtesy of Leo T. Chylack, Jr., M.D.) The key insight of the grading scheme is the separation of nuclear brunescence from nuclear opacification. Each of these aspects is graded on a scale of 1 to 6. Most clinicians pick up the habit in residency of simply glancing at a cataract and jotting down “3+ NS” for a moderately advanced senile cataract that is well along in nuclear sclerosis (hardening). Yet we cannot directly judge nuclear hardness at the slit lamp. A patient may complain of multiplopia and have progressive myopic shifting of the spectacle correction, with a modest amount of green-brown coloration but a high degree of haze in the central nucleus and less haze in the periphery. The rating would then be NC 2 (minimal color) and NO 5 (very significant opalescence). An elderly patient with 20/40 distance, J 1 near vision might have a dark brown but relatively clear lens, similar to the color of Coca-Cola. The rating might be NC 6 or NO 3. In both cases, the rating is much more meaningful than 2+ NS or 4+ NS, respectively. The first patient needs surgery; the second may not.
PREVENTION PEARLS AND
DAMAGE CONTROL: PART 2
PREOPERATIVE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree