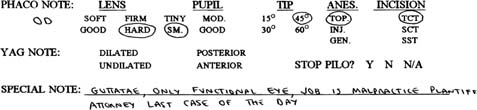
Chapter 28 The best ideas are often not only the most creative, they’re the most efficient as well. There’s a story about a New York City executive who was going to Asia for two weeks on business. She went to her Wall Street bank and requested an immediate loan of $5,000. When asked for collateral, she offered the keys to her Rolls Royce and said, “You keep it until I pay off the loan.” So, the bank gave her the money and parked the car in their underground garage. Two weeks later, the executive was back, bringing in a check for $5,000 plus $15 interest. The loan officer took the payment, then said, “I’m sorry, but I have to ask, you’re obviously wealthy. You own a Rolls. Why did you need to borrow $5,000?” “I didn’t,” she answered, “but where else could I park that car in Manhattan for two weeks and pay only $15?” Ideas, processes, and techniques that add efficiency and creativity to our cataract surgeries are the footings of this text. In this chapter I describe my personal observations regarding prevention and damage control. Indeed, Ashleigh Brilliant has advised, “If you can’t learn to do it well, learn to enjoy doing it badly.” While that may hold true for such joyous activities as playing golf (based upon my personal experience and which explains the sports analogies in this chapter), it would not be acceptable for the enhancement and preservation of vision. Thus, my objective here is to surf through the multiple steps in the cataract removal process and to click onto those that I feel I have at least some potential to be helpful with. This chapter is devoted either to preventing problems or, if they do occur, to recognizing them early and nipping them in the bud before they get bigger. I have been fortunate to have been exposed to several surgeons who I consider to be masters of phacoemulsification. I have learned much from them. And I have observed a common denominator among them: they all major in the minors; that is, they pay a lot of attention to seemingly small details. Even things as basic as patient selection and scheduling should remain in the forefront. Since 1986, I have been employing what I call an individualized “phaco note.” It is created at the time of the preoperative office examination, and is a written game plan for each patient. It includes such things as characteristics of the cataract, how well the pupil dilates, the type of phaco needle to be used, the form of anesthesia to be employed, the planned incision characteristics, and any special considerations (Fig. 28–1). This special considerations section can contain a vast array of information; for example (1) difficult access characteristics such as deep-set eyes, prominent brows, or unusual positioning requirements secondary to back, neck, or breathing abnormalities; (2) delicate corneal conditions such as guttatae, scarring, or thinning; and (3) the need for special instrumentation such as a prechopper, a pupil stretcher, or a vitrectomy kit. The benefits of this phaco note are many. It helps me to begin the visualization process, much as a professional athlete does. Because a copy of it is given to the operating room personnel well in advance, it helps them to have the proper positioning alternatives, special instruments, etc., readily available. And, lastly, it provides a template for my scheduling technicians. I don’t care how many thousands of golf holes I might have played in my life, the next time out I still would prefer to start the round with several “easy” holes, that is, holes that I have a reasonable chance to par or birdie. I definitely don’t want to start off with a 600+ yard par 5 with a narrow fair-way, out-of-bounds both right and left, to an island green the size of a postage stamp! The same with my cataract surgery days. The scheduling technicians know how to interpret these phaco notes and they will make every effort to schedule our cases starting with those that I feel will be technically the easiest to the most difficult. In fact, just to be absolutely certain, there are occasions on which I make notation in that special considerations section to the effect “schedule as the last case of the day.” FIGURE 28–1 An example of the phaco note prepared for every surgery. (Now that I review this particular case again, I think the best prevention pearl for me would be to send it to Dr. Fishkind!) I would never entirely discount the role of luck. But there is also no doubt that the more we can displace luck with preparation and the more we major in such minors as patient selection and scheduling, the greater the potential for a successful surgical outcome. If phaco was a game, winning or losing it would pivot around the surgeon’s ability to understand and control phaco fluidics, and what a complex subject it is! So many variables influence it. Many have been covered in Chapter 25. But let me underscore the prevention aspect of being positive that our phaco incision size properly matches our phaco tip/handpiece configuration. Over the last year, I have visited many operating rooms to observe surgery. I have seen great techniques and beautiful outcomes. But I’ve also seen missed opportunities to prevent snafus. Phaco incision size is a common one, especially with clear cornea or near-clear incisions. My personal bias is toward standard phaco tips with an internal diameter of 0.9 mm. With those, I recommend an internal phaco incision width of 2.8 mm. A larger incision allows for excessive incisional outflow and compromised fluidics. A smaller incision risks restricted outflow and the possibility of a corneal burn. With the downsized phaco tips (as small as 0.6 mm internal diameter) the internal phaco incision might need to be as small as 2.4 mm. The point is that the incision size should be based upon science and not habit. It’s a tough game to win if you go to the plate with two strikes against you. Before I get off my incision size soapbox, let me also make some comments regarding the side-port incision employed by surgeons who prefer the two-hand techniques. Incisional leakage has an untoward effect on phaco fluidics, and the eye doesn’t much care about the location of the leakage. We can create the most balanced phaco incision in the history of cataract surgery and still negatively influence fluidics by creating an unnecessarily large side-port incision. If you routinely create side-port incisions, exactly how large do you intend it to be: 0.5 mm, 1.0 mm, 1.5 mm? Or are you like I was for too many years, when I just took the knife I was handed and poked it in? I had so much incisional leakage through the side port that it put Old Faithful to shame. Thankfully, those days are gone. What is the appropriate side-port incision size? It is dependent on what is used as a second instrument. It should be just big enough to allow entry and exit of the second instrument. And although I’ve not used every chopper, manipulator, and rotator on the market (there are not enough days in one’s lifetime to do so!), I’ve used many of them, and a side-port incision of no greater than 0.5 mm is a decent approximation. I can hear some of you already, “Come on, Dave, you’re telling me there’s a meaningful difference between a 0.5 mm and a 1.0 mm side incision?” But we’re majoring in minors here. It’s not necessarily a back-breaker, but it can be a back-acher. One last thought about this now properly sized side-port incision: don’t use it unless something truly contributory is happening through it. For too many years I would place the second instrument through the side port at the beginning of the phaco process and leave it in the eye until the end. Then I realized that it was the presence of the second instrument (especially through a too-large side incision) that was causing side-incision leakage and causing the posterior capsule to come forward! So I ask myself constantly, “Is my second instrument really advancing this phacoemulsification in a safe and positive fashion, or am I leaving it in the eye simply because it’s convenient to do so?” Although at first it may seem to be an inconvenience to be putting your second instrument in and out of the eye, you will notice improved fluidics with it out of the eye. This will result in improved followability and chamber stability (assuming there is the proper phaco incision/phaco tip combination).
PREVENTION PEARLS AND
DAMAGE CONTROL: PART 1
PATIENT SELECTION AND SCHEDULING
THE GREAT GAME OF PHACO
ONE-HANDED TWO-HANDED PHACO
THE NO-EXCUSE HYDRODISSECTION: THE COLVARD MANEUVER
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree