• Oral anticoagulation therapy (such as Coumadin with INR 2-3) is recommended for AF patients before and after cardioversion for at least 4 weeks regardless of their CHADS2 score.
• Systemic anticoagulation such as Coumadin with INR 2-3 is recommended for all patients for at least 2 months following an AF ablation procedure. Continuation of systemic anticoagulation more than 2 months following ablation should be based on the patient’s risk factors, including assessment with CHADS2 or CHA2DS2VASc score, and other risk factors for stroke and not on the amount of AF or type (paroxysmal, persistent or long-standing persistent AF) of AF.
MANAGEMENT OF PATIENTS WITH HIGH INR
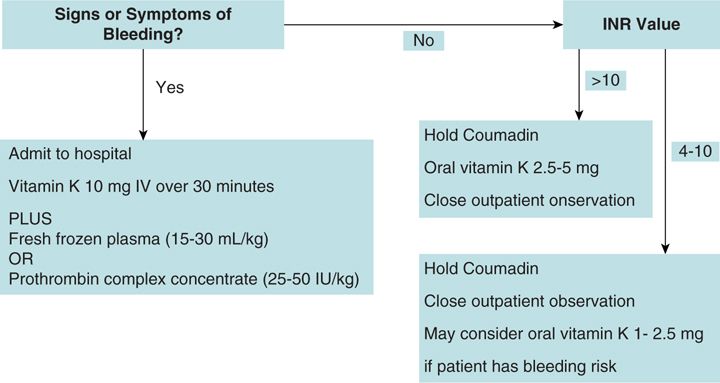
If a patient’s INR is high (≥4.0) or Coumadin therapy needs to be reversed clinically, an algorithm could be followed as suggested by Garcia and Crowther6 and as shown in Figure 27-1.
FIGURE 27-1 Suggested algorithm for the management of patients with international normalized ratio (INR) over 4. Abbreviation: IV, intravenously. (Modified with permission from Garcia DA, Crowther MA. Reversal of warfarin: case-based practice recommendations. Circulation. 2012;Jun 12;125(23):2944-2947).
ALTERNATIVES TO ANTICOAGULATION WITH COUMADIN
• Dabigatran (Pradaxa) and rivaroxaban (Xarelto) are new anticoagulants approved for the prevention of thromboembolic events in AF patients. There is no need for laboratory monitoring for INR or dietary restrictions. However, these agents carry the bleeding risks similar to that of Coumadin and are without a reliable reversal agent.7
• Combined therapy with clopidogrel (Plavix) and aspirin may occasionally be considered if the patient is not a suitable candidate for Coumadin or dabigatran or rivaroxaban. But this dual antiplatelet therapy is less effective for the prevention of thromboembolic events.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree