FIGURE 61-1 Presenting rhythm strip.
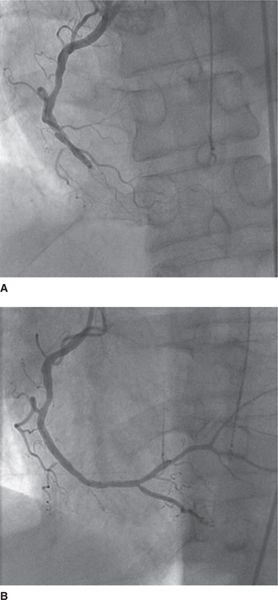
FIGURE 61-3 Angiograms of occluded and revascularized right coronary artery. (A) The initial angiogram of the right coronary artery, which is occluded. (B) The vessel after successful percutaneous intervention.
FIGURE 61-4 Monitor tracing while awaiting hospital discharge. Thirty-five beats of monomorphic ventricular tachycardia are shown. The irregularity and acceleration suggests an automatic mechanism from injured myocardium.
DISCUSSION
The patient under discussion suffered a cardiac arrest in the setting of acute MI. This does not represent a guideline-driven indication for implantation of an ICD.1 The ventricular tachycardia recorded on the day of planned discharge, more than 48 hours after the infarction was nonsustained, accelerating, and likely automatic given the clinical circumstances. This suggests a changing substrate but not necessarily a fixed substrate with scar at risk for later ventricular tachycardia.
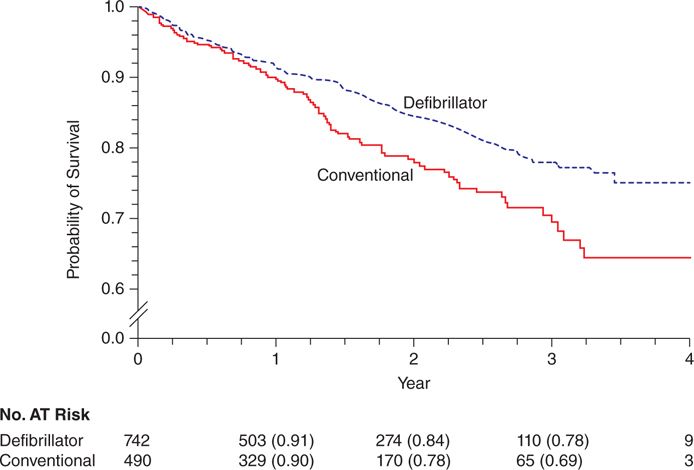
In the Multicenter Automatic Defibrillator Implantation Trial II (MADIT-II), patients with chronic ischemic heart disease, prior MI, LVEF ≤30%, and no requirement for ventricular arrhythmias or electrophysiologic study were randomized to receive either optimal medical therapy (OMT) or OMT with an ICD.2 The study showed a clear benefit from ICD implantation (Figure 61-5). Exclusions to enrollment in MADIT-II included MI within 1 month or revascularization within 3 months of the index MI.
FIGURE 61-5 MADIT-II results. Kaplan-Meier survival probabilities of survival in patients treated with an ICD and conventional medical therapy. There was a benefit from ICD therapy (P = 0.007). Reproduced with permission from Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;Mar21;346(12):877-883.
The device-based therapy guidelines state that primary prevention ICD therapy is indicated in patients with an LVEF of ≤35% due to prior MI who are at least 40 days post-MI and in NYHA functional class II or III.1 Furthermore, since revascularization was performed, implicit in the guidelines is that a 3-month waiting period is indicated for this indication since recommendations were based on MADIT-II, which excluded patients from randomization within that time frame. In addition, the national coverage determination precludes reimbursement by Medicare for devices implanted within these waiting periods.3 Notably, since the arrest occurred in the setting of acute MI, it does not represent an indication for secondary prevention ICD implantation either.
Additional evidence supporting the inadvisability of implanting an ICD within the first month following MI derives from the Defibrillator in Acute Myocardial Infarction Trial (DINAMIT)4 and the Immediate Risk Stratification Improves Survival (IRIS) study.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree