Pregnancy and Infertility
This chapter discusses the biochemical changes that occur in pregnancy and how clinical biochemistry tests can be used in the investigation of infertility.
PREGNANCY AND LACTATION
If the ovum is fertilized, it may implant in the endometrium, which has been prepared by progesterone during the luteal phase. The function of luteinizing hormone (LH) is taken over by human chorionic gonadotrophin (hCG), produced by the chorion and developing placenta. Human chorionic gonadotrophin is similar in structure and action to LH and prevents the involution of the corpus luteum as circulating pituitary gonadotrophin concentrations fall. Consequently, plasma oestrogen and progesterone concentrations continue to rise and endometrial sloughing is prevented. Progesterone is initially produced by the corpus luteum of the ovary for the first 8 weeks of pregnancy, then from implantation of the embryo the placenta takes over progesterone synthesis. During pregnancy the predominant oestrogen is oestriol produced by the placenta. Prolactin concentration gradually increases during the first two trimesters and then rises steeply, to about 8000 mU/L, in the third trimester.
Prolactin, oestrogens, progesterone and (human) placental lactogen stimulate breast development in preparation for lactation. High plasma oestrogen concentrations inhibit milk secretion; lactation can start only when plasma concentrations fall after delivery of the placenta. Initially lactation depends on prolactin. Suckling stimulates secretion of the hormone, but, even during lactation, plasma prolactin concentrations fall progressively post partum and reach non-pregnant levels after 2 or 3 months. Apart from the effects on the breast, the high plasma concentration of prolactin interferes with gonadotrophin and ovarian function and produces a period of relative infertility.
Monitoring pregnancy (placental function)
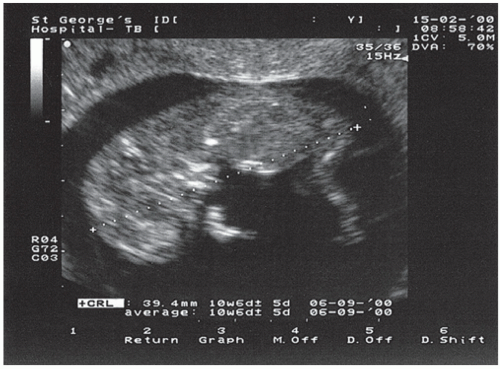
Substances produced by the fetus or placenta (fetoplacental unit) may be measured in maternal plasma or urine to detect fetal abnormalities or to monitor the progress of the pregnancy, for example low urine unconjugated oestriol (E3) is associated with poor pregnancy outcome. Such sampling is relatively safe and simple, but occasionally more invasive testing, such as of amniotic fluid obtained by amniocentesis, may be needed. However, the ability to visualize the fetus using ultrasound (Fig. 10.1) and the use of cardiotocography for detecting fetal heart rate have reduced the need for such tests.
Human chorionic gonadotrophin
The secretion of hCG by the placenta reaches a peak (rising to about 500 000 U/L) at about 13 weeks of pregnancy and then falls. The fetoplacental unit then takes over hormone production, and the secretion of both oestrogen and progesterone rises rapidly. Plasma or urinary hCG concentrations, which give positive results at 1 or 2 weeks after the first missed menstrual period, are most commonly used to confirm pregnancy.
However, by using more sensitive immunoassay techniques, plasma hCG may be detected soon after implantation of the ovum and before the first missed period.
However, by using more sensitive immunoassay techniques, plasma hCG may be detected soon after implantation of the ovum and before the first missed period.
Measurement of plasma hCG is also useful if an ectopic pregnancy is suspected, in conjunction with ultrasonography, or if the patient is being treated for infertility. Serial hCG measurements may be used to assess the progress of early pregnancy; single values are difficult to interpret because of the wide reference range. As a rough guide, plasma concentrations should double every 2 days in a normal pregnancy. Raised plasma hCG not due to pregnancy can be due to gestational or nongestational trophoblastic neoplasia or the menopause.
Human placental lactogen
This is a peptide hormone synthesized by the placenta. It is detectable in maternal plasma after about the eighth week of gestation and has been used to assess the likelihood of threatened miscarriage and to monitor late pregnancy, but now is rarely used.
Detection of fetal abnormalities
Some fetal abnormalities may be diagnosed by tests carried out on maternal plasma or amniotic fluid. Amniocentesis is a procedure by which amniotic fluid is obtained through a needle inserted through the maternal abdominal wall into the uterus and is usually carried out after about 14 weeks’ gestation. The procedure carries a small risk to the fetus. Both the safety and the reliability of the procedure can be improved if combined with ultrasound examination in order to locate the position of the fetus, placenta and maternal bladder.
CASE 1
A 20-year-old woman attended the antenatal clinic in the 17th week of pregnancy for a Down’s syndrome screen test. A plasma α-fetoprotein (AFP) was 67 kU/L (reference median being 38 kU/L for 17 weeks). Her other blood tests were normal.
DISCUSSION
It was feared that the fetus had a neural tube defect because of the raised plasma AFP concentration. However, an ultrasound scan showed a twin pregnancy and no evidence of a neural tube defect. Other causes of a raised plasma AFP concentration include incorrect gestational dating, fetal renal disease, duodenal/oesophageal atresia and ventral wall defects or exomphalos.
Analytical results may be misleading if, for example, the specimen is contaminated with maternal or fetal blood or maternal urine, is not fresh or is not properly preserved. Close liaison between the clinician and the laboratory staff helps to ensure the suitability of the specimen and the speed of the assay. Amniotic fluid is probably derived from both maternal and fetal sources, but its value in reflecting abnormalities arises from its intimate contact with the fetus and from the increasing contribution of fetal urine in later pregnancy.
Detection of neural tube defects
α-Fetoprotein (AFP) is a low-molecular-weight glycoprotein synthesized mainly in the fetal yolk sac and liver. Its production is almost completely repressed in the normal adult. It can diffuse slowly through capillary membranes and appears in the fetal urine, and hence in the amniotic fluid, and in maternal plasma. Severe fetal neural tube defects, such as open spina bifida and anencephaly, are associated with abnormally high concentrations in these fluids. The reason for this is not clear, but the protein may leak from the exposed neural tube vessels.
As well as neural tube defects, the causes of raised AFP concentration in amniotic fluid and maternal plasma include:
multiple pregnancy,
serious fetal abnormalities,
exomphalos.
In some countries, pregnant women attending for antenatal care are offered plasma AFP assay at between 16 and 18 weeks’ gestation to screen for the presence of a fetus with a neural tube defect (although highresolution ultrasound is beginning to replace this test). The gestational age should be confirmed by ultrasound, which should also exclude a multiple pregnancy as a cause of high concentrations.
Positive results should be confirmed on a fresh sample, which, if still high and if the diagnosis has not been confirmed by ultrasound, may be followed by AFP estimation on amniotic fluid. This is a more precise diagnostic test and yields fewer false-positive results than plasma assays if sampling is properly performed. It should be reserved for subjects known to be at risk, either because of a family history of neural tube defects or because of the finding of a high concentration in maternal plasma with a normal or equivocal ultrasound scan.
Amniotic fluid acetylcholinesterase assay is now rarely used to detect certain fetal malformations, including neural tube defects and exomphalos. It gives reliable results up to about 23 weeks’ gestation. The interpretation of the result is less dependent on fetal age than AFP, but is equally invalidated by contamination with fetal or maternal blood. The assay is less widely available than that for AFP.
Detection of Down’s syndrome
Low maternal plasma AFP and unconjugated oestriol, and raised hCG and inhibin A concentrations, measured between 15 and 20 weeks’ gestation, are associated with an increased risk of the fetus having Down’s syndrome (trisomy 21) and used as a second trimester screening test. This combination of tests (quadruple or Quad test) to screen for the congenital disorder is available in specialized laboratories. Fetal nuchal translucency determined by high-resolution ultrasound, along with raised pre-β-hCG and reduced pregnancy-associated plasma protein A (PAPP-A), are used as a first trimester (10-14 weeks’ gestation) screening test; increased nuchal thickness (Fig. 10.1) is associated with chromosomal abnormalities. A definitive test is amniocentesis, which allows the collection of fetal cells for karyotyping. The risk of Down’s syndrome increases with maternal age.
Detection of other fetal abnormalities
Chromosomal abnormalities and some inborn errors of metabolism may be detected by cytogenetic, biochemical or enzymatic assays on cells cultured from amniotic fluid or after biopsy of chorionic villi. These tests are performed only in special centres and usually on individuals with a family history of a genetic condition. Circulating fetal deoxyribonucleic acid (DNA) in maternal blood may also prove to be useful.
Assessment of fetomaternal blood group incompatibility
Rhesus or other blood group incompatibility has effects on the fetus, which may be assessed by measuring amniotic fluid concentrations of bilirubin in conjunction with maternal antibody titres. Normally bilirubin concentrations in amniotic fluid decrease during the last half of pregnancy. The concentrations at any stage correlate with the severity of haemolysis. The result is read off a Liley chart relating optical density of amniotic fluid at 450 nm (an indirect measure of bilirubin) against gestational time. Such tests may allow the optimum time for induction of labour or the need for intrauterine transfusion to be assessed.
Assessment of fetal lung maturity
The examination of amniotic fluid has also been used to assess pulmonary maturity. Immature lungs do not expand normally at birth and may cause neonatal respiratory distress syndrome (hyaline membrane disease), with the need for respiratory support. It is therefore important to have evidence of pulmonary maturity before labour is induced. At about 32 weeks’ gestation, the cells lining the fetal alveolar walls start to synthesize a surface-tensionlowering complex (surfactant), 90 per cent of which is the phospholipid lecithin, which contains palmitic acid. Surfactant is probably washed from, or secreted by, the alveolar walls into the surrounding amniotic fluid, in which both lecithin and palmitic acid concentrations steadily increase. The concentration of lecithin, relative to another lipid, sphingomyelin, which remains constant in amniotic fluid, can be measured. A rise in the lecithin to sphingomyelin ratio may help determine pulmonary maturity, and a ratio less than 2 implies immaturity. This invasive test is rarely indicated now as steroids, which induce surfactant synthesis, are sometimes given to patients who have premature rupture of the membranes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree