Overview
The relationship between health, work and wellbeing is complex and best understood using a biopsychosocial approach
There are several different models of occupational health service delivery
An assessment of occupational health needs is key to the delivery of an appropriate service
Communication is an important aspect of practice and should be conducted within a framework of confidentiality and consent
Introduction
Occupational health (OH) is an endeavour which is contributed to by clinicians, technical specialists and professionals from a range of science backgrounds (Box 4.1). Each will have their area of special knowledge (e.g. a physician will primarily be expert in occupational medicine and therefore the diagnosis and management of occupational disease) and all should have an understanding of the beneficial contributions that can be made by other disciplines and the synergies that can result from multidisciplinary working.
- Specialist occupational health physicians
- Specialist nurse practitioners in occupational health
- Other doctors and nurses working in occupational health
- Clinical support workers
- Occupational health technicians
- Psychologists
- Counsellors
- Occupational hygienists
- Health and safety advisers
- Ergonomists
- Epidemiologists
- Toxicologists
- Radiation protection advisers
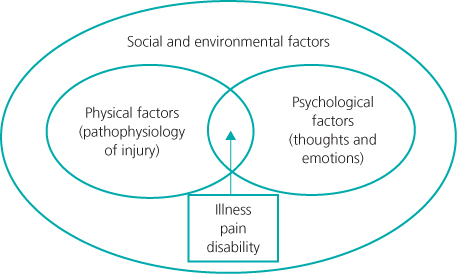
There is now a wider understanding of the need to address the complex interaction between work and health as distinct from workplace safety, and this growing recognition is reflective of the increasing maturity of occupational health as a discipline. The World Health Organization (WHO) 1995 statement on OH (Box 4.2) is still valid today, and emphasizes the concept of the wellbeing of workers; a theme that has been further developed in recent years and has been the subject of a national review in the UK, ‘Working for a Healthier Tomorrow’. The cause and effect relationship between physical hazard and injury is more readily understood in the context of occupational safety whereas a biopsychosocial approach (Figure 4.1) is required to address the altogether more complex issue of health, work and wellbeing.
The objectives of an OH service are influenced by statutory requirements for compliance with health and safety legislation, national and other guidance for occupational fitness, and the need for medical advice to inform management action. Looking beyond these fundamental elements, a complementary definition of occupational health might be, ‘The value added to workers’ health and wellbeing by an employer’s activities to realize key business benefits’. One of the challenges for OH practitioners is to demonstrate that benefit by means of meaningful outcome-based metrics or key performance indicators (Box 4.3).
- health protection
- liaison with treating health professionals
- active work rehabilitation
- workplace health promotion and the support of national health screening programmes
- an advisory function to management and workers, anticipating the benefits and losses that may arise from changes to work or work practices and importantly
- monitoring of its own activities so that meaningful data accrue
Provision of Occupational Health Services
There is statutory provision of OH services in many European countries, including France, Spain, the Netherlands, Belgium, Portugal, Germany, Denmark and Greece. In Italy occupational and environmental health services are provided within the national health service. In the UK there is no regulation requiring the provision of OH services by employers, although all employees of the National Health Service (NHS) should have access to an accredited specialist in occupational medicine.
The WHO has formulated a concept of basic OH services which extends the principles of primary healthcare to occupational health (Box 4.4). The ‘intermediate level’ referred to anticipates a regulatory or inspectorate function provided by an occupational health institution containing both occupational medical expertise and the provision of clinical services. The Occupational Safety and Health Administration (OSHA) in the United States regulates workplaces and enforces health and safety law whereas NIOSH (National Institute for Occupational Safety and Health), a branch of CDC (Centres for Disease Control) conducts research and makes recommendations on matters of occupational health and safety. These twin functions are combined in the UK Health and Safety Executive (HSE), with the Health and Safety Laboratory (HSL) providing technical occupational safety and medical advice particularly to the HSE.
- Available to all working people
- Addressing local needs
- Adapted to local conditions
- Affordable to providers and clients
- Organized by the employer for employees
- Provided by the public sector for the self-employed and the informal sector
- Supported by intermediate level services
The roots of OH in Germany go back to 1884 when Otto von Bismarck set up a social insurance system emphasizing prevention, rehabilitation and compensation from a single source. This insurance-based system sees the federal technical inspection services of the statutory accident insurers assessing the compliance of employers with regulations and adjusting their premiums based on risk.
The organization of OH services in the UK varies, as does their level of service provision. They may be provided by in-house OH departments, external (outsourced) private OH companies, or a combination of the two. The latter can consist of a small corporate OH (or OH plus safety or plus environment or even plus consumer safety) function procuring certain services from contracting bodies. Access to OH services tends to be universal in the public sector and large private companies, whereas the services available to and/or taken up by small and medium-sized enterprises (SMEs) (defined as those with fewer than 250 employees) tend to be limited.
Multinationals often provide comprehensive in-house OH services which are truly multidisciplinary and can influence population health within the regions or even the countries in which they operate by initiatives such as building local health clinics. However, even these multinational companies tend to outsource their OH services to the private sector, sometimes retaining a Chief Medical Officer as an ‘intelligent customer’. In the UK, the public sector is the largest user of OH services, either in-house or contracted. Most NHS OH services are in-house, and many provide commercial OH services to a number of external enterprises (both small local companies and larger industries) as a means of income generation. Large private OH companies tend to focus their activities on large Government or commercial OH contracts.
SMEs, representing a large proportion of the overall UK economy, tend to have limited access to OH services, with the decision to purchase such services often driven either by a need to comply with health and safety legislation, the need for health surveillance or management’s occasional need for medical advice in the case of a sickness absence problem. Where SMEs do procure OH services, they tend to be from smaller private OH companies, individual practitioners, NHS OH services, or local general practices. To address this variability, access to a government-funded OH telephone advice line is now available to all SMEs (and also to GPs who may need occupational health advice for their patients (Health for Work Adviceline www.health4work.nhs.uk)).
Services can be delivered in a number of ways, and can and should use innovative methods where these enhance occupational health. This increasingly includes the use of telemedicine for remote workers, secure online questionnaires, electronic fitness confirmation to facilitate pre-placement, occupational health assessment, and spirometry with remote over-read by a respiratory physiologist to ensure quality standards and consistent reporting.
In order to make an informed decision about OH provision and how this should be delivered, an OH needs assessment should be undertaken. A needs assessment may simply be based on an organization’s health and safety risk assessment; however, an experienced occupational physician is likely to identify pertinent risks to health that may have been overlooked by a health and safety professional, and a workplace visit to inspect the circumstances of work should always be incorporated (Figure 4.2). In addition a thorough assessment would include a consideration of the relevant policies that the company has or should have (e.g. drugs and alcohol, absence management), and relevant occupational health and safety statistics (e.g. workplace accidents, sickness absence data). Also included might be the need for health promotion in that particular work environment (Figure 4.3), and to make recommendations for the involvement of OH in committees such as those owned by human resources, risk management/health and safety, standard setting and communication. The OH needs as perceived by relevant stakeholders (e.g. managers, employees, lawyers, human resources, etc.) should naturally be taken into account
Figure 4.2 Performing a workplace visit allows the circumstances of work to be observed. Wood workshop: note the crushed ventilation exhaust tubing on the floor. Wood dust is a recognized respiratory sensitizer and hardwood dust can cause sinonasal cancer.

Figure 4.3 Cigarette ends in a metal swarf bin at an engineering works. Targeted workplace health promotion can help reduce the risk of occupational respiratory disease, the medical effects of smoking and fire.

Relationships with Others
The procurement, and often the line management of OH services, is usually the responsibility of the human resources function of a business. This can sometimes lead to a skewing of the delivery of OH towards the human resources agenda and away from aspects of provision concerned with legislative compliance and the effects of work on health. The OH practitioner may therefore have to make the case for investigative, preventive and health surveillance activities with support from those responsible for organizational health and safety compliance.
The OH service should have a close working relationship with the risk management/health and safety function as accident and other incident data can inform OH activity whereas OH data may contribute to better risk assessment and therefore prevention. Compliance, policy development and mitigation of legal liability may also be aided by cooperation. There may be other specialist functions within an organization where an interdependency with the OH service should occur such as infection prevention and control in a healthcare setting. The senior management of any organization is probably the most important influence on organizational health as through its actions and policies does the organizational culture develop. It is therefore important that the lead OH clinician has good access to key senior managers, who will act as champions for occupational health. Generally a holistic approach to occupational health is aligned with organizational aims, since the health of the workforce is assured and individuals feel secure and valued at work
The Government’s role in occupational health in the UK had until about 2006 been limited to that of enforcement and guidance through the efforts of the HSE, although greater emphasis was given to safety. This has in part been redressed by the current HSE strategy in which one of the aims is ‘To specifically target key health issues and to identify and work with those bodies best placed to bring about a reduction in the incidence rate and number of cases of work related ill health’. The HSE’s parent body, the Department of Work and Pensions (DWP) has done much to highlight the role of OH. With the Department of Health, the DWP commissioned Dame Carol Black’s seminal review, and the Government’s response has included some useful initiatives in the health and work sector. Examples are the introduction of ‘Fit notes’, the inclusion of work-based outcomes in guidance from the National Institute for Health and Clinical Excellence, and educational projects for GPs designed to increase their confidence in dealing with work-related matters. However, although the HSE publishes annual statistics on health and safety, these relate to its activities rather than the ‘occupational health of the nation’, and at a local level workplace health is not a matter normally to be addressed in the reports of Directors of Public Health. Furthermore, although GPs have been encouraged to become more aware of work and health the recording of a patient’s occupation is not often done and may therefore inhibit the recognition of work-related issues and informed advice on a return to work (Figure 4.4).
Figure 4.4 To advise on fitness for work a doctor would need to know at least the patient’s job. A welder in a foundry uses air arc gouging, note the fume, intense light including UV, heat and several trip hazards.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree