![]() LEARNING OBJECTIVES
LEARNING OBJECTIVES
After reading this chapter, the pharmacy student, community practice resident, or pharmacist should be able to:
1. Identify the different players involved in MTM services.
2. Categorize potential payers of MTM services.
3. Evaluate variables to include in the business plan for MTM services.
4. Explain the difference between hard and soft dollar saving.
5. Recognize important components to evaluating documentation software.
 INTRODUCTION
INTRODUCTION
As pharmacists, most of us enter the profession because of a desire to help patients. This mission is exemplified through the practice of medication therapy management (MTM) services. There are a variety of services that pharmacists can offer to help patients better understand their medications and disease states. It is essential to realize that MTM services have different meanings in various health-care groups and can mean evaluation of patient-specific medications, disease-specific management, or a mixture of the two. Generally, reimbursement from insurance companies for MTM is only for face-to-face sessions and telephone consults. In the future, hopefully, reimbursement for telehealth services will emerge. To provide MTM services, one must be aware of the people involved, the barriers, and important financial considerations to grow a successful business.
 IDENTIFY THE PLAYERS
IDENTIFY THE PLAYERS
In providing MTM services, there are many people involved, including the patient and/or caregiver, pharmacist, prescriber, support staff, pharmacy students, and payer. Through professional collaboration, everyone involved works together with the patient to achieve their personal health goals.
The Patient/Caregiver
The patient is the central focus of MTM services. Patients often are caught up in the traditional role of the pharmacist as a medication dispenser. MTM is a new concept to many patients and may initially require more education and persuasion to participate in the service. Patients are often overwhelmed with numerous medications, disease state, and dietary instructions. Patients must feel that you are a credible health-care professional qualified to review both medications and disease states with them. One way to increase patients’ trust in your services would be to mention that you work collaboratively with their physician to share information to make the best therapeutic decisions. To begin, make sure that all information provided is individualized for that specific patient. Start the session with a few general open-ended questions to learn more about the patient and their current state of management. Then, use this information to customize your message specifically to the patient. For example, instead of saying “People with diabetes should be on a statin for cholesterol,” you could say, “I see that Dr. Good has put you on simvastatin, which is a recommended drug for cholesterol in people with diabetes.” Also, if there is a legal caregiver or a spouse present, involve them as much as possible to increase their awareness of how they can be a better support to their loved one. Patients do not respond well to health-care providers who “talk above their head.” Make sure that all information is delivered in a way that is appropriate for the individual’s age and literacy level.
The Pharmacist
Pharmacists should always have a positive attitude about the profession and the services they provide. The pharmacist is a crucial part of MTM services. MTM is a way for you to gain a more intimate relationship with your patients. It may be difficult at first to determine where the line is between patient counseling and providing MTM services. However, MTM focuses on the next level of patient care by addressing things like therapeutic goals, medication nonadherence, or efficacy issues.1
By developing a closer patient—pharmacist relationship, you are also helping to build patient loyalty to your pharmacy. In delivering your services, remember to start with general concepts about their medication or disease state and then move to more specific points. If you develop a basic foundation, your patients are much more likely to understand the information you present and to be able to apply it to their daily lives. Be sure to update all health-care professionals involved in a patient’s care on your findings and education with the patient.
The pharmacist is the advocate for the necessity of MTM to both the patient and payer. To produce a successful MTM business, the pharmacist must take on many different roles, including clinician, marketer, business manager, and collaborator. By participating in medication management services, you are marketing yourself as a medication expert. Therefore, it is imperative to the success of your practice that you live up to the expectations of the patients and prescribers with which you work. Commit yourself to being a lifelong learner by keeping up with current medications, disease state guidelines, health-care issues, immunization recommendations, and professional opportunities. As you gather information from various sources, choose reference articles that are of specific interest to you and contact the author for more information. Pharmacists should be professional at all times when interacting with patients, support staff, and other health-care providers. It is up to the pharmacist to engineer a practice that revolves around patient care and improves the profession.2
The Prescriber
The prescriber is an integral part of MTM and must be included in therapy-altering decisions. Prescribers should also receive updates on your interventions with their patients. As you prepare to provide MTM services, let the prescribers with whom you will be working know what to expect and what services you will provide. As with patients, you must work with the prescriber to cultivate an acceptance of the clinical pharmacist’s role. Keeping them informed about your services will increase their acceptance of your practice and recommendations.
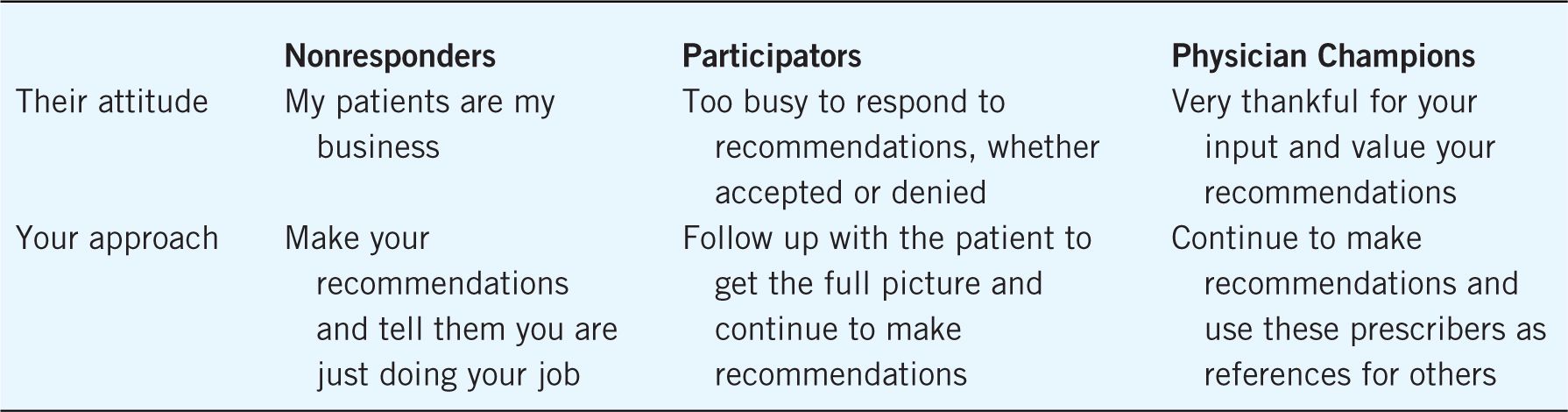
Prescribers are similar to patients in that there is not one overall approach and each intervention must be individualized. Although there is a wide spectrum of collaboration, typically prescribers can be divided into three categories: The Physician Champions, The Participators, and The Nonresponders. The Physician Champions are those prescribers who go beyond merely following recommendations and often consult you on cases. They can also be influential in persuading others to accept your clinical role and recommendations. The Participators are those prescribers who participate in MTM by accepting recommendations, but may not be quite as involved as the Physician Champion. The Participators understand that you are trying to work synergistically for the best interest of the patient. The Participators may not always communicate directly with you. They may fail to include you in the communication loop or update you on the status of your recommendations. To determine the outcome, you must follow up directly with the patient. The Nonresponders are those who reply to your recommendation with comments such as “I don’t need you to do this” or “These are my patients and I will make the therapy decisions.” To these prescribers you politely respond that it is your job to assess the therapy and share therapy recommendations with the prescriber, who may choose not to accept the recommendation. Of course, there are prescribers who fit between categories, or may be best classified on a case-by-case basis.
Support Staff
Developing a solid support staff is key to a successful MTM service. Tasks such as scheduling patients, billing payers, filing documentation, and drawing labs are all great ways that a trained support staff member could lighten the load of the pharmacist. Also, these staff members can assist in marketing strategies and help to create and distribute promotional items. Staff members should be well trained and have sound patient interaction skills. By delegating these tasks, the pharmacist can focus on billable patient interaction time and documentation.
Pharmacy Students
Pharmacy schools are now more actively preparing students to pursue clinical roles. Pharmacy students are an excellent resource when providing MTM services. An instructional training module should be created to best represent the MTM process. Pharmacy students should also be familiar with current guidelines and recommendations for the management of different diseases. The most important point when utilizing a pharmacy student is that they should prepare interview questions ahead of the appointment for the preceptor to review. It is often intimidating for students to initiate patient interactions, and important points can be missed. Create a documentation guide that will ensure that the proper questions are asked. Before becoming the lead interviewer on an MTM case, have the student sit in with you for an appointment as an observer. Then, following the session, ask questions about the patient conversation and highlight pertinent points. The mission to expand MTM services is fulfilled through properly utilizing students and training the next generation of pharmacists.
 IDENTIFY AND ENGAGE THE PLAYERS
IDENTIFY AND ENGAGE THE PLAYERS
There is no question that MTM services provided by pharmacists are a valuable asset to both the patient and the overall health-care system. However, to make this endeavor worth your time you must be compensated for your services. Unlike the dispensing role, there is no tangible product when billing for MTM services, and you are being paid solely for your expertise and time. For the greatest chance of financial stability, structure your practice so that there is a mixture of payer types. There are several different payer sources, which include self-funded employer groups, private insurance employer groups, Medicaid (for applicable states), Medicare Part D prescription drug plans, and self-pay patients.
Self-Funded Employer Groups
Self-funded employer groups are recommended as a target for services because they pay the health-care costs of their employees and greatly benefit from MTM services. Self-funded groups usually comprise greater than 500 employees, but could have as few as 200 employees. For the best outcome, try to aim for those employers who already have some sort of health or wellness initiative. An active wellness initiative shows that the company considers the health and welfare of their employees a priority. Use your networking skills to identify a key person in the organization to approach for brainstorming and to gather information on the services that would best benefit the employer to build your service plan.
There are a few different ways to approach payment for services, including per member per month, per employee per month, price per disease state case, hourly rate, daily rate, or percentage of health-care savings. For example, you could charge $X per member per month for 500 employees or $X per diabetes patient. There is a difference between per member per month and per employee because most plans allow the employee to have dependents who may also be eligible for your services. Whatever your structure, the cost of your services should not exceed the savings the service will generate. For the best participation, persuade the employer to provide some type of incentive for employees to participate. Incentives could be in the form of paid time to exercise, offering discounts on healthier food options for lunch or snack, gym membership discounts, and more. In your initial meetings with the employer to design your service, determine what is important to them. This will help you create reports that are the most meaningful to your client. Also, make sure that expectations and time lines are clear from the planning stages for a smooth transition to providing the services.
Medicare Part D Plans
The Medicare Modernization Act of 2003 developed requirements for MTM programs as away to optimize therapeutic outcomes and control costs for patients. Each Part D plan must include an MTM program within the benefits package. To be included in the MTM program, the plans target members with multiple chronic disease states, multiple covered prescription medications, and incur annual costs that exceed a preset threshold. The Centers for Medicare and Medicaid Services (CMS) determines the range of parameters for inclusion.
At a minimum, sponsors must target at least four of the following seven core chronic diseases: Hypertension, Heart Failure, Diabetes, Dyslipidemia, Respiratory Diseases (such as Asthma, Chronic Obstructive Pulmonary Disease or Chronic Lung disorders), Bone Disease-Arthritis (such as Osteoporosis, Osteoarthritis, or Rheumatoid Arthritis), and Mental Health Diseases (such as Depression, Schizophrenia, Bipolar Disorder, or chronic and disabling disorders).3
CMS has established that the plan must include beneficiaries receiving between two and eight Part D covered medications. However, the specific number and drug classifications included are left for each plan to select. For example, each plan can choose whether any Part D medication can be included, or each can include only those medications directly linked to the targeted disease states. The anticipated incurred medication costs are also a trigger for inclusion into the programs. However, the exact dollar amount of this requirement fluctuates with each CMS update (pharmacists should refer to the latest update for the most recent information). Each individual plan has variations on the different requirements. All plans are required to have person-to-person interaction that can be defined as in-person or telephone interventions. Although plan sponsors are only required to target beneficiaries for the MTM program enrollment quarterly, some plans identify beneficiaries monthly.4
Medicare plans have certain services that are required to be included in the MTM package. The CMS states that plans “must offer a comprehensive medication review (CMR) by a pharmacist or other qualified health-care provider at least annually and perform quarterly medication reviews with follow-up interventions when necessary.” The comprehensive medication review is an interview where the pharmacist reviews all of the patient’s prescriptions, herbal supplements, dietary foods, and over-the-counter (OTC) medication regimens to observe possible noncompliance, misuse, underuse, or therapeutic duplication. The pharmacist should provide patient education as necessary. Often the patient will learn something new during this encounter even about chronic prescriptions. The goal is to offer this person-to-person session as a time for patients to really focus on their therapy and ask questions about the medications they take. Pharmacists should also have patients demonstrate the use of medication devices to confirm proper usage. Plans also require that the patient be provided with some sort of written documentation to summarize the session. This is most commonly fulfilled through a personal medication record, medication action plan, and personalized education recommendations. An efficient platform collects data throughout the intervention and can populate the required documentation during the encounter. In the future, CMS may require a more standardized approach across all plans. Plans are also required to include physician interventions in their program structure.3
Consultations can be performed in a variety of ways including fax, telephone, or mailed communication. As you work with the physicians you will learn which methods of communication are most effective. Individualizing communications with each physician’s preferred method will promote the pharmacist–physician relationship. The Medicare plans are operated through different platforms, providing the opportunity to experience diverse approaches to structuring MTM.
Self-Pay Patients
Patients are often unsure of their insurance coverage for medication management services. Many personal
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


