Chapter 46 Postoperative Wound Complications (Case 31)
Postoperative context: A 32-year-old man 5 days after exploratory laparotomy for a gunshot wound to the abdomen with increased incisional drainage.
| Hematoma | Seroma | Enterocutaneous fistula |
| Superficial wound infection | Dehiscence/evisceration | Necrotizing fasciitis |
PATIENT CARE
Clinical Thinking
• Evaluate the patient for signs of systemic infection, local infection, or unexpected wound drainage. R/o wound complications that might require immediate surgical attention.
• Evisceration implies that the skin has opened and intra-abdominal contents are exposed. This complication requires immediate stabilization at the bedside and, in most cases, exploration and closure in the OR.
• Necrotizing fasciitis is a serious wound infection that spreads quickly. Tx necessitates urgent wide surgical debridement and broad-spectrum antibiotics.
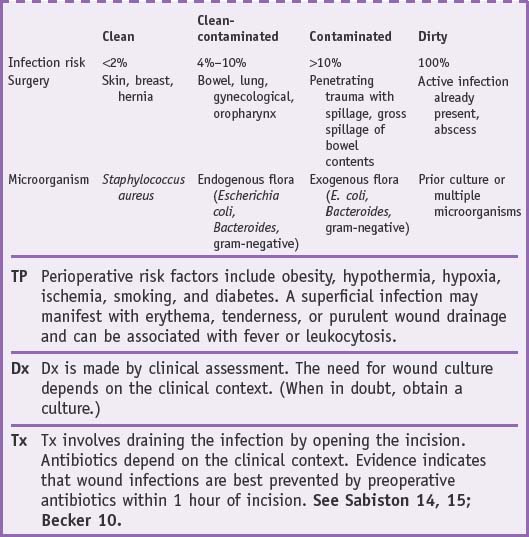
• Superficial wound infections usually require bedside wound exploration to allow adequate drainage.
• Surgical wounds heal by primary intention, by secondary intention, or by delayed primary closure. Apposed skin edges held together by sutures or staples heal by primary intention. A wound left open to granulate over time is healing by secondary intention. Delayed primary closure involves apposing the wound edges after a few days of a wound left open. It has been shown this delay in wound closure increases the tensile strength of the wound and resistance to infection.
History
• Review the details of the surgical procedure. Review the method of closure (staples or sutures, retention sutures, open packing, drains, etc.).
• Determine the timing of the complication in relation to surgery. Foul-smelling serous drainage with crepitus in the first 12 hours may indicate necrotizing fasciitis. Salmon-colored fluid draining within the first week after abdominal surgery implies wound dehiscence. Drainage suggestive of intestinal contents is probably an enterocutaneous fistula, which can present from days to weeks following abdominal surgery.
Physical
• Dressings should be changed daily. Inspect the wound for surrounding erythema, skin breakdown, bleeding, or obvious drainage. Characterize and quantify drainage.
• Palpate the wound gently to elicit skin blanching, tenderness, crepitus, or drainage. The four classic signs of wound infection are redness, swelling, heat, and pain (in Latin: rubor, tumor, calor, dolor). Pain is the most sensitive indicator of infection.
Tests for Consideration
| $30 | |
| $45 | |
| $100 | |
| $66 |
| Clinical Entities | Medical Knowledge |
|---|---|
| Hematoma | |
| PΦ | Hematoma is generally the result of inadequate intraoperative hemostasis and occurs not infrequently in patients who are anticoagulated in the perioperative period. |
| TP | Hematoma may present as bloody wound drainage or an expanding mass and is a clinical dx made at the bedside. |
| Tx | Tx is usually supportive with pain control, ice packs, and local compression. Expanding hematomas that are extremely painful or compromise hemodynamics from compression or blood loss necessitate operative evacuation. Failure to identify the source of a hematoma is not unusual. Due to the potential for airway compromise, neck hematomas should be considered for emergent return to the OR for evacuation and hemostasis. As blood is also an excellent medium for infection, hematomas in contaminated fields should be evacuated. See Sabiston 15, Becker 8. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree