Problem 3 Postoperative hypotension
You are the resident on call for general surgery and called to the ward to review a 70-year-old man who has become increasingly unwell over the course of the day. The nursing staff are concerned about his deterioration. Five days earlier the patient had undergone an Ivor Lewis oesophagogastrectomy and spent the first 3 days uneventfully on the intensive care unit. He was making satisfactory progress and was transferred to the surgical ward on day 3.
With the various possibilities in mind, you head towards the ward.
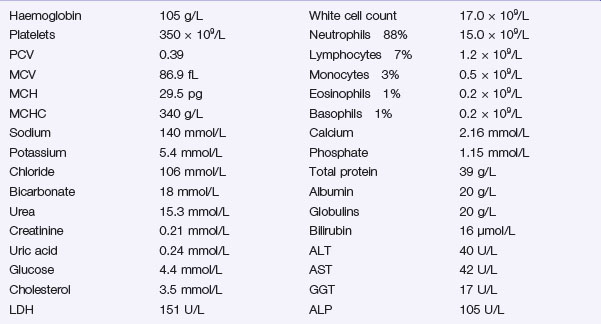
The following results become available:
Investigation 3.2 Arterial blood gas analysis on room air
| pO2 52 mmHg | pCO2 34 mmHg |
| pH 7.29 | Base excess −9.5 |
A portable chest X-ray is performed (Figure 3.1).
The chest effusions are further visualized with a contrast-enhanced CT scan of the chest and abdomen. One sequence is shown (Figure 3.2).
Answers
Cardiogenic shock occurs secondary to a primary pump failure.
There are several potential causes in this case:
You have these thoughts in mind as you head towards the ward.
A.2 Additional information may be available from several sources: