Postherniorrhaphy Inguinodynia: Causes, Prevention, and Surgical Treatment: Triple-Neurectomy
Parviz K. Amid
David C. Chen
Background
While the recurrence rate of inguinal hernia repairs is significantly reduced by use of mesh and tension-free techniques, postherniorrhaphy chronic pain remains the concern of hernia surgeons around the globe. Based on the classification of pain by the International Association for the Study of Pain (IASP), postherniorrhaphy inguinodynia can be broadly divided into nociceptive and neuropathic pain. There is no sharp line between the nociceptive and neuropathic pain, and the gray zone is further complicated by social, genetic, patient, and psychological factors.
Nociceptive pain is caused by activation of nociceptors by nociceptive molecules due to tissue injury or inflammatory reaction, and transmitted to the brain via A-delta and C-fibers. Nociceptive pain can be reduced by gentle tissue handling, using local anesthesia to reduce production of nociceptive molecules, and avoiding forceful tissue retraction.
Neuropathic pain is caused by direct nerve injury and characterized by inguinodynia with radiation to the scrotum/femoral triangle, paresthesia, allodynia, hyperpathia, hyperalgesia, hyperesthesia, hypoesthesia, and positive Tinel sign. Neuropathic pain can be reduced from the universally reported rate of 5% to 8% to a fraction of 1% by identification of nerves and their protection from direct contact with mesh that can lead to structural changes of nerve fibers. In-depth groin neuroanatomy knowledge is of paramount importance if postherniorrhaphy chronic pain is to be avoided.
Groin Neuroanatomy Within the Inguinal Canal
The ilioinguinal nerve is located over the spermatic cord, covered and protected from the mesh by the investing fascia of the internal oblique muscle (Fig. 1). This protective fascia should not be damaged by removing the nerve from its natural bed. Dissecting the ilioinguinal nerve from the cord and placing it below the inguinal ligament, which was the teaching of a prior era, destroys the protecting fascia of the nerve and risks perineural scaring and direct contact of the nerve with mesh.
The genital branch of the genitofemoral nerve is located under the cord, covered and protected from direct contact with mesh by the deep cremasteric fascia. Although small and difficult to see, its location can be determined by the easily visible “blue line” of the external spermatic vein that is always adjacent to the nerve (Fig. 2). To ensure safety of the nerve it must be kept with the cord while the cord is separated from the inguinal floor under direct vision. Grasping the cord with the thumb and index fingers and pulling it off the floor is also a bad habit from the past, and damages the deep cremasteric fascia, which can also lead to perineural scaring and direct contact of the genital nerve with the implanted mesh.
The iliohypogastric nerve is located between the external and internal oblique
layers covered and protected from mesh by the investing fascia of the internal oblique muscle (Fig. 3). The key step to expose the iliohypogastric nerve is opening the anatomic cleavage between the internal and external oblique layers high enough to expose the internal oblique aponeurosis. This step that takes only a few seconds easily and automatically exposes the iliohypogastric nerve. The iliohypogastric nerve has an easily visible part over the internal oblique aponeurosis; however, below the point marked by the arrow in Figure 4, the nerve has a hidden segment that runs inferiorly and laterally within the internal oblique muscle (Figs. 4 and 6). This segment of the iliohypogastric nerve is the most vulnerable neural structure of the inguinal area because it is not visible within the operative field. Passing suture through the internal oblique muscle, or the so-called conjoined tendon, for its fixation to the inguinal ligament, flat mesh, or plug has the potential risk of injuring the intramuscular segment of the nerve with the needle, or entrapping it by the suture. In less than 5% of patients, the iliohypogastric nerve runs under the internal oblique aponeurosis in a subaponeurotic location. In these cases the location of the nerve must be determined by noting the point of its simultaneous exit from the external and internal oblique layers (Fig. 5). Furthermore, in these instances, no suture or fixating device should be inserted into the internal oblique aponeurosis below the area marked by the “xs” in Figure 5 to avoid injuring the nerve that runs inferiorly and laterally underneath the internal oblique aponeurosis (Fig. 6).
layers covered and protected from mesh by the investing fascia of the internal oblique muscle (Fig. 3). The key step to expose the iliohypogastric nerve is opening the anatomic cleavage between the internal and external oblique layers high enough to expose the internal oblique aponeurosis. This step that takes only a few seconds easily and automatically exposes the iliohypogastric nerve. The iliohypogastric nerve has an easily visible part over the internal oblique aponeurosis; however, below the point marked by the arrow in Figure 4, the nerve has a hidden segment that runs inferiorly and laterally within the internal oblique muscle (Figs. 4 and 6). This segment of the iliohypogastric nerve is the most vulnerable neural structure of the inguinal area because it is not visible within the operative field. Passing suture through the internal oblique muscle, or the so-called conjoined tendon, for its fixation to the inguinal ligament, flat mesh, or plug has the potential risk of injuring the intramuscular segment of the nerve with the needle, or entrapping it by the suture. In less than 5% of patients, the iliohypogastric nerve runs under the internal oblique aponeurosis in a subaponeurotic location. In these cases the location of the nerve must be determined by noting the point of its simultaneous exit from the external and internal oblique layers (Fig. 5). Furthermore, in these instances, no suture or fixating device should be inserted into the internal oblique aponeurosis below the area marked by the “xs” in Figure 5 to avoid injuring the nerve that runs inferiorly and laterally underneath the internal oblique aponeurosis (Fig. 6).
 Fig. 1. Ilioinguinal nerve is located over the cord, covered and protected by the investing fascia of the internal oblique fascia (pointed to by the arrow). |
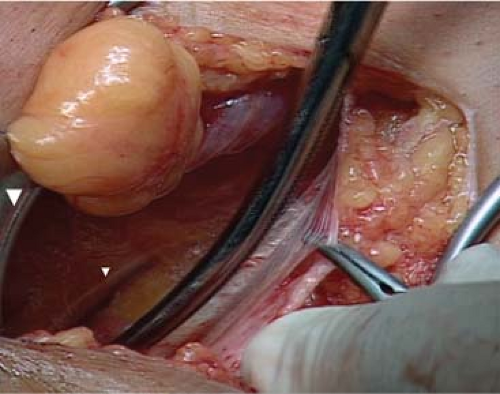 Fig. 2. Inguinal segment of the genital branch of the genitofemoral nerve is located under the cord (pointed to by the arrow), covered and protected by the deep cremasteric fascia. |
Causes of Neuropathic Pain
Neuropathic pain can be caused by (a) structural injuries such as axonotmesis (disruption of axon and myelin sheath with preservation of the connective tissue covering of the nerve), neurotmesis (partial or complete severance of a nerve, with disruption of the axon and its myelin sheath and the connective tissue elements) due to cutting, thermal, or traction injuries leading to traumatic neuroma formation, and myelin degeneration and separation, axon crystallization due to direct contact of nerves with mesh; (b) entrapment injuries by suture, fixating devices, or wrinkled mesh or meshoma.
Triple neurectomy, advocated by us in 1995, is currently a universally accepted surgical treatment for neuropathic pain refractory
to nonsurgical modalities. Neurolysis, which does not address ultrastructural changes of nerve fibers, is no longer recommended. Also, removal of entrapping sutures or fixating devices that leave the injured crushed nerves behind is not recommended. Moreover, we do not recommend single or double neurectomy, as it does not address structural changes of the nerves that are not visible by naked eyes. The nerves should be resected proximal to the field of original hernia repair and as distally as possible. Although there are no data available, we recommend ligation of the cut ends of the nerves to avoid neuroma formation, and inserting the proximal cut end into the muscle to keep the nerve stump away from the future scarring of the operative field. The ilioinguinal nerve can be identified lateral to the internal ring, between the ring and the anterior superior iliac spine. If the nerve cannot be easily seen, it could be found underneath the fat-covered grooves in the internal oblique muscle fibers. The iliohypogastric nerve can be easily found within the anatomic cleavage between the external and internal oblique aponeurosis. After visualization, the nerve should be traced proximally within the fibers of the internal oblique muscle to a point lateral to the field of the original hernia repair. Failure to do so may leave the injured intramuscular segment of the nerve behind. In those instances where the iliohypogastric nerve has a subaponeurotic course, the internal oblique aponeurosis is split below the point of its simultaneous exit from the internal and external oblique aponeurosis to visualize the hidden nerve (Fig. 6). The inguinal segment of the genital branch of the genitofemoral nerve can be identified between the cord and the inguinal ligament and traced laterally to the internal ring where it is severed. An easier alternative is to visualize the nerve within the internal ring through the lateral cruse of the ring.
to nonsurgical modalities. Neurolysis, which does not address ultrastructural changes of nerve fibers, is no longer recommended. Also, removal of entrapping sutures or fixating devices that leave the injured crushed nerves behind is not recommended. Moreover, we do not recommend single or double neurectomy, as it does not address structural changes of the nerves that are not visible by naked eyes. The nerves should be resected proximal to the field of original hernia repair and as distally as possible. Although there are no data available, we recommend ligation of the cut ends of the nerves to avoid neuroma formation, and inserting the proximal cut end into the muscle to keep the nerve stump away from the future scarring of the operative field. The ilioinguinal nerve can be identified lateral to the internal ring, between the ring and the anterior superior iliac spine. If the nerve cannot be easily seen, it could be found underneath the fat-covered grooves in the internal oblique muscle fibers. The iliohypogastric nerve can be easily found within the anatomic cleavage between the external and internal oblique aponeurosis. After visualization, the nerve should be traced proximally within the fibers of the internal oblique muscle to a point lateral to the field of the original hernia repair. Failure to do so may leave the injured intramuscular segment of the nerve behind. In those instances where the iliohypogastric nerve has a subaponeurotic course, the internal oblique aponeurosis is split below the point of its simultaneous exit from the internal and external oblique aponeurosis to visualize the hidden nerve (Fig. 6). The inguinal segment of the genital branch of the genitofemoral nerve can be identified between the cord and the inguinal ligament and traced laterally to the internal ring where it is severed. An easier alternative is to visualize the nerve within the internal ring through the lateral cruse of the ring.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



