Polyarteritis Nodosa
Surya V. Seshan, MD
Key Facts
Terminology
Necrotizing inflammation of medium-sized or small arteries without glomerulonephritis or vasculitis in arterioles, capillaries, or venules
Clinical Issues
HBV association in ˜ 36% of PAN cases
Up to 77/million in endemic areas for hepatitis B viral infection
Adult: Peak at 5th to 7th decade
Multisystemic involvement
Rarely, ANCA positive
Kidney frequently involved (70-80%)
New onset hypertension, sometimes malignant range
Cyclophosphamide and steroids for severe cases, remission in 90%
Image Findings
Angiography localizes microaneurysms
Microscopic Pathology
Intralobar, arcuate, and, rarely, interlobular arteries affected (medium-sized vessels)
Characteristic features are fibrinoid necrosis and transmural and periarterial inflammation
Late arterial lesions include aneurysms and stenosis
Top Differential Diagnoses
Kawasaki disease
ANCA-related small vessel vasculitides
Systemic lupus erythematosus
Fibromuscular dysplasia
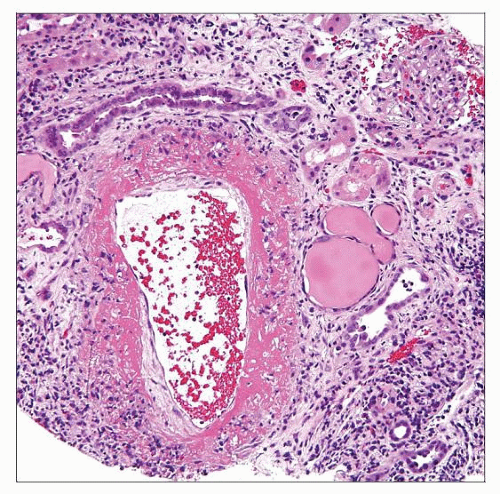 Kidney biopsy in polyarteritis nodosa (PAN) shows circumferential, transmural fibrinoid necrosis and active inflammatory infiltrate composed of neutrophils and lymphocytes. |
TERMINOLOGY
Abbreviations
Polyarteritis nodosa (PAN)
Synonyms
Macroscopic polyarteritis
Classic polyarteritis nodosa
Kussmaul and Maier periarteritis nodosa
Definitions
Chapel Hill Consensus Conference criteria
Necrotizing inflammation of medium-sized or small arteries without glomerulonephritis or vasculitis in arterioles, capillaries, or venules
American College of Rheumatology criteria
Weight loss ≥ 4 kg, livedo reticularis, testicular pain or tenderness, myalgias, weakness or leg tenderness, mono- or polyneuropathy, diastolic BP > 90 mmHg, elevated BUN or creatinine, hepatitis B virus, biopsy diagnosis of small or medium-sized arteries, arteriography with aneurysms or occlusions in visceral arteries
3 or more of the above criteria have high sensitivity and specificity for diagnosis
EULAR/PRINTO/PRES criteria for childhood PAN
Necrotizing vasculitis, angiographic abnormalities, and either skin involvement, myalgia/muscle tenderness, hypertension, peripheral neuropathy, or renal involvement
ETIOLOGY/PATHOGENESIS
Infectious Agents
Hepatitis B virus (HBV)
Accounts for ˜ 36% of PAN cases
Possibly other bacterial and viral infections
Hepatitis C virus (HCV)
Rarely HIV, Epstein-Barr virus
Other
HBV immunization
Exposure to silica-containing compounds
In majority, etiology is unknown
Pathogenesis
Immunologically mediated
Believed to be chronic immune-complex mediated disease
Resembles chronic serum sickness model
Probably a T-cell-mediated immune component
Antigen unknown
May be microbial or autoantigen in vessel wall
Participation of neutrophilic and mononuclear inflammatory infiltrate (T cells and macrophages)
Weakness in vessel wall leads to thrombosis or fibrosis and microaneurysm formation
Chronic, cyclic insults support presence of different stages of vasculitis
CLINICAL ISSUES
Epidemiology
Incidence
2-31/1,000,000 in Europe and USA
Some studies have included cases now classified as microscopic polyangiitis
Up to 77/1,000,000 in endemic areas for hepatitis B viral infection
Age
Adults: Peak at 5th to 7th decade
Children: 7-11 years
However, less common in children
Gender
Male predilection (M:F = 2:1)
Ethnicity
2x higher prevalence in Europeans vs. others
Specific HLA haplotypes
Involves all ethnic groups
Presentation
Multisystemic involvement
Clinical symptoms related to ischemia and are dependent on organ involved and disease severity
Constitutional symptoms: Fever, malaise, weight loss, myalgia, abdominal pain
Renal
Kidney frequently involved (70-80%)
Focal renal infarction (˜ 30%)
Microaneurysms (˜ 65%)
Hematuria, proteinuria (˜ 20%)
Loin pain
Acute renal failure
New onset hypertension, sometimes malignant range
Rare: Rupture of kidney with perirenal hematoma
Massive retroperitoneal and peritoneal hemorrhage following rupture of arterial aneurysm
Heart
Ischemic heart disease
Neurologic (10%)
Focal defects, hemiplegia, visual loss, mononeuritis multiplex
Skin
Varied lesions: Palpable purpura, necrotic with peripheral gangrene, livedo reticularis, ulcers
Subcutaneous nodules
Skeletal muscle and mesentery (30%)
Gastrointestinal, peripheral nerves, skin (50%)
Laboratory Tests
Anemia, leukocytosis, thrombocytosis
Elevation of ESR and C-reactive protein
Positive hepatitis B serology in some cases
No specific serologic tests
No significant association with ANCA
Rarely, ANCA positive (usually perinuclear) by indirect IF only, when overlap with microscopic polyangiitis
Treatment
Steroid therapy is 1st line of therapy; remission in 50% of patients
Cyclophosphamide and steroids for severe cases; remission in 90%
Plasma exchange/plasmapheresis in refractory cases
HBV-associated PAN needs antiviral therapy
Prognosis
Fulminant disease with < 5-year survival
40% of patients have relapse
5 factor score (FFS) estimates prognosis
Scores renal (Cr > 1.6 mg/dL, proteinuria > 1 gm/24 hr), GI, cardiac, and CNS involvement
Lower score correlates with better 5-year survival
IMAGE FINDINGS
Ultrasonographic Findings
Pulsed and color Doppler ultrasonography
Localization of microaneurysm (seen in 50-60%)
Computed Tomography Angiography
Microaneurysms often seen at artery bifurcations
Tc-99m DMSA uptake scanning detects patchy renal parenchymal disease
MICROSCOPIC PATHOLOGY
Histologic Features
Glomeruli
Mostly varying degrees of ischemic collapse associated with vessel involvement
Global glomerulosclerosis with tubular atrophy in healed cortical scars
Normal histology of glomeruli located away from vasculitis
Rarely, focal crescentic glomerulonephritis (pauci-immune type)
Suggests overlap of PAN and microscopic polyangiitis
Rarely, positive ANCA reported
Tubules and interstitium
Acute ischemic infarction in distribution of affected artery
Tubular simplification, atrophy, and mild interstitial fibrosis
Active &/or chronic interstitial and periarterial inflammation
Arteries
Intralobar, arcuate, and, rarely, interlobular artery affected (medium-sized vessels)
Small arterioles and capillaries lacking muscular coat are not affected
Obliterative arteritis (acute, subacute, or chronic)
Characteristic features are fibrinoid necrosis and transmural and periarterial inflammation
Fuchsinophilic/eosinophilic amorphous fibrinoid material in areas of necrosis
Destruction of medial smooth muscle
Disruption of internal and external elastic laminae
Moderate to intense inflammatory infiltrate
Neutrophils, eosinophils with karyorrhexis
Activated T-lymphocytes and monocytes/macrophages
Varying degrees of luminal narrowing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



